Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Enfermería Global
versión On-line ISSN 1695-6141
Enferm. glob. vol.17 no.52 Murcia oct. 2018 Epub 01-Oct-2018
https://dx.doi.org/10.6018/eglobal.17.4.289311
Originals
Prevalence of health assistance infection in patients hospitalized in intensive therapy unit
1 Enfermera. Alumna concluyente de la residencia en Enfermería en Unidad de Terapia Intensiva del Programa de Residencia Multiprofesional del Hospital Universitario Onofre Lopes (HUOL/UFRN). Brasil. a.elza@uol.com.br
2 Enfermera. Doctora en Ciencias de la Salud CCS/UFRN, Maestra en Enfermería por la Universidad Federal de Rio Grande do Norte - UFRN. Profesora del curso de de Enfermería de la Universidad Federal do Rio Grande do Norte - UFRN . Brasil.
3 Maestra en Enfermería por la Universidad Federal do Rio Grande do Norte. Enfermeira do Hospital Universitário Onofre Lopes - HUOL. Brasil.
4 Enfermero. Maestro en Enfermería por la UFRN. Profesor del curso de Enfermería de la Universidad Federal do Rio Grande do Norte - UFRN. Brasil.
5 Fisioterapeuta. Profesora Adjunta III - FACISA/UFRN. Doctora en Ciencias de la Salud (UFRN). Jefe de la Clínica Escuela de Fisioterapia de FACISA. Brasil.
6 Maestra y Doctora en Enfermería por la Universidad Federal de Rio Grande do Norte - UFRN. Profesora del curso de Enfermería de la Universidad Federal do Rio Grande do Norte - UFRN. Brasil.
Objective:
To determine the prevalence of Infection Related to Health Care (IRHC) in patients admitted to the Intensive Care Unit (ICU).
Method:
Descriptive, retrospective study, with a quantitative approach. Data were collected through a form completed from infection notifications, followed by analysis of the results of microbiological tests available on the MV 2000i system.
Results:
The patients admitted to the ICU were female, elder and came from other inpatient units of the institution. The prevalence rate of infection was 5.3% confirmed by positive culture, and the respiratory system was the most frequent site of infection (42.5%). Most isolates were gram-negative pathogens (71.05%), highlighting the Acinetobacter sp. The antibiogram showed that Klebsiella sp. was resistant to ampicillin and amoxicillin plus clavulanic acid. Regarding Pseudomonas sp., 50% were resistant to imipenem, cefepime and ciprofloxacin. All Acinetobacteres were resistant to ceftazidime, followed by ceftriaxone and cefepime.
Conclusion:
The prevalence of IRHCs in critically ill patients represents a huge challenge, not only for professionals, but also for health managers and the whole society, justifying the need and relevance of actions aimed at prevention and control.
Descriptors: Nosocomial Infection; Intensive Care Units; Microbial Drug Resistance
INTRODUCTION
Health Care-Related Infections (HCRI) are adverse events that persist in the country's public health scenario and relate to increased hospitalization time, morbidity and mortality and costs of care1 .
Infection rates in teaching or university hospitals are higher in the Brazilian scenario, a fact that is justified by the typical characteristics of these institutions, such as: diversity of pathologies, practice of high complexity procedures, prolonged hospitalization periods, interaction with several health professionals and students in the area. Furthermore, they are acquiring technical skill by performing invasive procedures, which constitutes additional risk for contamination2 .
According to Ordinance No. 2,616 of the Brazilian Ministry of Health, hospital infection is the one that arises after 72 hours of hospitalization, or before, since it relates to diagnostic and/or therapeutic procedures performed with the patient, as well as after hospital discharge3 . Information on hospital infection rates are consolidated in many hospitals in the country, are little known or old4 .
Worldwide, it is estimated that almost half a million cases of HCRI occur each year in Intensive Care Units (ICUs)5 . Since the specificities of this sector make it an environment conducive to infections, such as the clinical severity of the patients, the need for prolonged hospitalization, immunosuppressive therapy, routine antimicrobial use and consequent resistance to microorganisms, and the use of invasive devices such as: Central Venous Catheter (CVC), Delay Urinary Probe (DUP), and Orotracheal Tube (OTT) ventilation support 6 .
Given a global concern with issues aimed at minimizing adverse reactions to patients at health services, the Ministry of Health creates, through Administrative Rule 529/2013, the National Patient Safety Program (NPSP) in order to search for a safe care practice, based on protocols established by the World Health Organization (WHO). Hand hygiene practice consisted of one of the protocols established by the document and a determining factor in the occurrence of infections in ICUs7 .
By understanding that the occurrence of infection in a hospital environment involves several factors internal and external to the individual, there is need for preventive, educational and epidemiological control measures aimed at controlling and reducing its appearance, in order to achieve accepTable rates according to the public profile and types of procedures performed by the institution4 .
Therefore, characterization, as well as the dissemination of infection rates in the hospital environment are relevant to sensitize the professionals of the multiprofessional health team, especially those working at the ICU, to the severity of the problem. Also, encouraging the adoption of measures that aim to prevent and minimize these diseases, contributing to a reduction in length of stay and morbidity and mortality rates. Moreover, the nurse is a professional who plays an important role in the adoption of measures of prevention and control of the ICU environment. Therefore, the study aimed to determine the prevalence of health care-related infection (HCRI) in patients admitted to an intensive care unit (ICU).
METHODOLOGY
This is a descriptive, retrospective, quantitative study, carried out at a university hospital, located in the city of Natal, state of Rio Grande do Norte. The institution is a reference in medium and high complexity in several specialties for the whole state, providing beds for clinical, surgical hospitalizations and cardiac emergencies.
The population consisted of all patients who performed cultures of biological material during hospitalization in the general adult ICU, from October 2014 to April 2015.
Suring the studied period, 749 patients were admitted to the ICU. In the study period, the Nosocomial Infection Control Commission (NICC) reported 40 infections per laboratory criterion in 33 patients, and five presented more than one infection in the respective period.
In order to select the sample, the study adopted the following inclusion criterion: patients aged 18 years old or more who underwent cultures during ICU stay. Patients with negative cultures and with diagnosis of pneumonia without laboratory criteria were excluded. Thus, the final sample consisted of 33 patients with laboratory-confirmed infection.
The data collection used a form, with sociodemographic variables (gender, age, origin, length of hospital stay and outcome) and clinical variables (type of patient, presence of community infection, isolated microorganism, infection focus and sensitivity) built by the researchers based on literature. Initially, the knowledge of infection reports was obtained through NICC records and the results of microbiological exams and the electronic medical record of the patients available in the MV 2000i® system.
The statistical data analysis used simple measures such as: distribution of absolute and relative frequencies. However, in order to study the association between hospital infection and types of procedures, the prevalence ratios were calculated. The Tables show the most significant data.
The study was carried out after approval by the Research Ethics Committee of the Federal University of Rio Grande do Norte (UFRN), with CAEE nº 36086414.0.0000.5537 in 2014, according to determinations of Resolution 466/12 of the National Health Council (8 .
RESULTS
There was a prevalence of infection of 5.3%. Table 1 below presents the sociodemographic characteristics and clinical data of the patients.
The data in Table 1 show that most of the respondents were female, with 21 (63.6%). The distribution by age group revealed that the minimum age was 18 years and the maximum, 92 years. However, the highest percentage was between 62 and 92 years (54.6%), with a mean age of 61.65 years and standard deviation of 14.90.
As to the origin of the hospitalized patients, 26 (78.8%) had been transferred to the ICU after hospitalization at other units of the same institution. Most of these patients underwent surgeries and procedures at the surgical and/or hemodynamic center of the institution, corresponding to 20 (60.6%) of the sample. Regarding the length of ICU stay, it ranged from two to 66 days, with an average of 27.42 days and a standard deviation of 13.85.
Of the surveyed patients, 31 (94%) did not have a previous diagnosis of community infection, while the others, 2 (6%) individuals, were diagnosed with pneumonia and the other with central nervous system infection. Regarding the clinical outcome, 19 (57.6%) patients were discharged from the ICU and 14 (42.4%) died.
The respiratory system was the most frequent site of infection with 17 (42.5%) cases, followed by urinary 10 (25%), bloodstream 9 (22.5%), vascular catheter 3 (7.5%) and nervous system 1 (2.5%).
Table 2 Frequency of microorganisms associated with HCRI cases in patients admitted to the ICU from October 2014 to April 2015. Natal, RN, 2015.

Of the microorganisms isolated in the cultures, the highest frequency was gram-negative bacteria, corresponding to 27 (71.05%) cultures, being Acinetobacter sp. the most prevalent pathogen, followed by gram-positive bacteria, 8 (21.05%) cases, and finally the fungi, with 3 (7.9%) cases. In two culture results, the microorganisms were not identified and were only defined as non-fermenting gram-negative bacilli, as shown in Table 2 .
Table 3 Susceptibility profile of microorganisms isolated in cultures according to antibiogram. Natal, 2015.
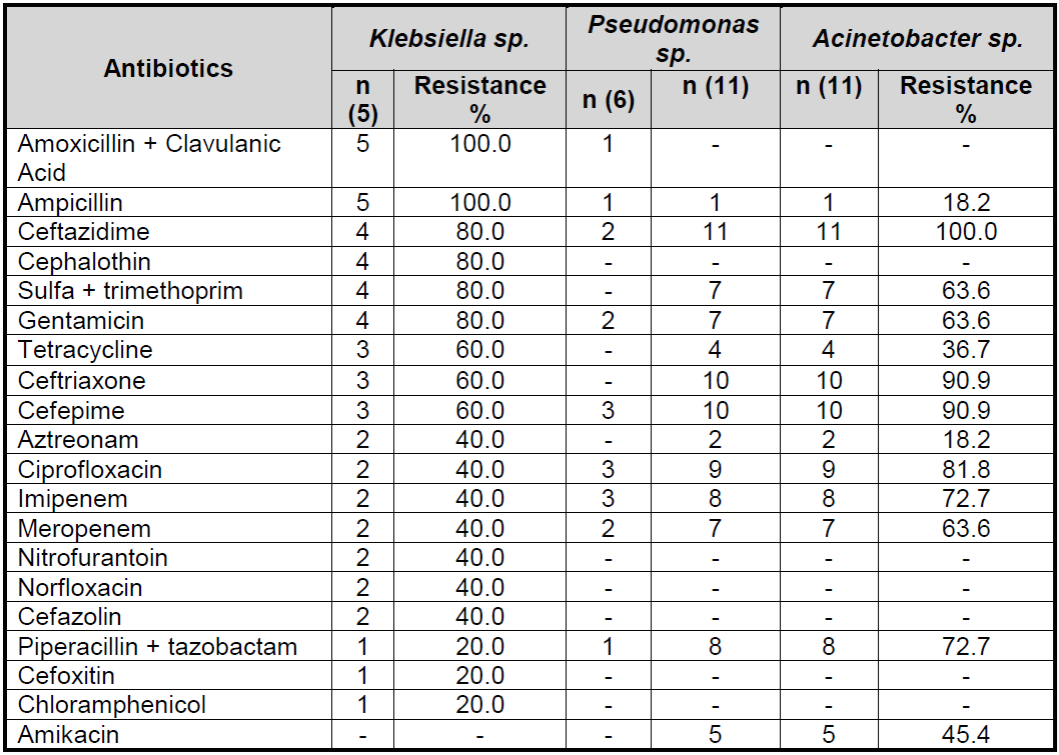
Table 3 represents the percentage of resistance and sensitivity to the antibiotics of the three most frequent microorganisms that were isolated in the cultures of patients hospitalized in ICU. In this sense, Klebsiella sp. was 100% resistant to penicillin: ampicillin and amoxicillin plus clavulanic acid. Half of the Pseudomonas sp. presented resistance to imipenem, cefepime and ciprofloxacin. All Acinetobacteres were resistant to ceftazidime, followed by ceftriaxone and cefepime.
DISCUSSION
The prevalence rate of infection was 5.3% for infections confirmed with positive culture of biological material at the ICU under study. Other studies found larger results, with values of 23.4% and 27%, respectively9)(10 .
The data obtained regarding the gender of the patients confirmed the predominance of the female gender, unlike what other studies found, with a frequency greater than male2)(11)(12 . Another study found similar age, with a mean of 63.02 years10 .
Thus, the data show that the elderly population represents an age group that needs health services more frequently, a fact that is justified by the natural aging process and the presence of chronic diseases, requiring highly complex resources 11 .
The length of stay of patients in the ICU was high and a study carried out at a teaching hospital in the state of Pernambuco found similar result, with a mean of 21 days and a standard deviation of 20 days13 . The long stay at the ICU presented a strong relationship with colonization by multiresistant microorganisms for the occurrence of HCRI, because, with the prolonged hospitalization time, the patient is exposed to other risk factors resulting from his/her clinical severity, need for invasive procedures and the risk of cross-infection14 . As observed in the present study, 60.6% of the patients were surgical and, due to the need for prolonged hospitalization, they were colonized or infected by pathogenic microorganisms.
In 6% of the sample, there was diagnosis of prior community infection, which implies a greater chance of infection during ICU stay compared to patients without previous infection6 .
The mortality rate found was 42.4%. Other studies found similar data, in which 42.5% and 50% of the patients died during ICU hospitalization9)(12 . The mortality rate at the ICU is known to be high, varying between 9 and 38% depending mainly on the profile of the assisted clientele. When it comes to mortality in patients who developed HCRI, this rate can reach 70% of the cases14 .
Multi-resistant microorganisms often fail to cause infection, but only colonization thus constitutes a hidden reservoir for the spread of these pathogens, and a large number of these patients receive antimicrobial treatment even without an indication15 . The frequency of positive cultures identified at the ICU and presented in this research does not determine the occurrence of infection in the patient, since correlation with the clinical evolution of the patient is necessary, since determinants of the individual, such as immunity, may not allow the infectious process.
Pneumonia acquired at the ICU associates with an increased hospitalization time and higher hospital costs, and may relate to ventilation-associated pneumonia (VAP) and to non-ventilated patients16 . As pointed out in the present study, in most ICUs, VAP is the most common among infections associated with invasive devices17 . A retrospective study of four ICUs from a public hospital in Fortaleza (CE) revealed a superiority of respiratory infections, corresponding to 65.3% (132) of the cases, followed by a 17.8% infection of the bloodstream and 16.9% Urinary Tract Infection (UTI) 18 .
VAP is recognized as the main infection causing high hospital mortality, especially when associated with antibiotic resistant bacteria, ranging from 20% to 70% of the cases and relates to a worse clinical outcome when caused by P. aeruginosa and A. baumannii18) . In this study, the frequency of these pathogens was 23.5% and 35.3%, respectively. A study carried out at an ICU of a teaching hospital in Recife (PE) found approximate results, with superiority of Acinetobacter sp. in 23.9% of the sample13 . The high occurrence of VAP associated with A. baumannii occurs due to its ability to form biofilms on the surface of the orotracheal tube, predisposing colonization in the lower respiratory tract of the individual19 .
UTI is characterized by the presence of an invading microorganism in any component of the urinary tract and accounts for about 30% of infections common in the hospital environment20 . When related to bladder catheterization, its contamination may occur during insertion of the catheter resulting from failure of aseptic technique; by ascending periurethral way, through the extraluminal environment between the probe and the urethral lumen; by intraluminal contamination13 .
UTIs in the hospital environment have a microbial profile different from those acquired in the community, generally related to gram-negative bacteria such as: Pseudomonas aeruginosa, Proteus sp., Klebsiella sp., Enterobacter sp., and some gram-positive bacteria such as Enterococcus and Staphylococcus, and Candida sp. fungi21 . In this study, Klebsiella sp. and Citrobacter were present in 60% of cases of UTI. They usually make up the microbiota of the man's intestine, mainly in the feces, so, due to its proximity to the genito-urinary tract, it and other enterobacteria commonly occur in the UTI22 .
Central Vascular Catheters (CVC) are routinely implanted devices in critical patients for treatment and care assistance. Nevertheless, it is a means of disseminating local or systemic infections, depending on the type of catheter, handling techniques, frequency of manipulation in addition to the individual's susceptibility13 .
In the etiology of these infections, Staphylococcus sp. is the most frequent pathogen. However, gram-negative bacilli, such as Candica sp. and Enterococcus are also involved. Differently from the results of the present study, in which Pseudomonas sp. and Acinetobacter sp. were isolated, which are pathogens frequently involved in infections when the patient underwent excessive antimicrobial therapy23 .
Bloodstream infections, which, in this study, was the third most common ICU infection, present two common explanations of colonization. The first concerns the migration of microorganisms from the skin to the incision, causing colonization of the catheter tip. The second results from catheter contamination, usually by manipulation, resulting in colonization of the catheter by migration of microorganisms. In addition, factors such as catheterization time, catheter material type, system handling techniques, ability of adherence of organisms, among others, are involved18 .
The most frequent pathogens isolated in this type of infection were Acinetobacter sp. with 33.3% of the cases, followed by Staphylococcus sp. with 22.2% cases, and one case of E. coli, Klebsiella, leuriform structures and non-fermenting bacilli. Differently from what another study24 observed, with a sample of 170 blood cultures, infections by Staphylococcus aureus and S. epidermidis corresponded to 58.5% of the sample and Acinetobacter baumanni, to 3.3% of the sample.
A study carried out at the ICU of a public hospital in Paraná identified 2.08% of infections in the Cerebrospinal fluid (CSF), corroborating with results observed in the present study, having as the isolated pathogen Acinetobacter sp. .( 25 . The prevalence of isolated microorganisms in cultures corroborates a study carried out at a hospital in João Pessoa (PB), which reported Pseudomonas aeruginosa, Acinetobacter and Klebsiella Pneumoniae, with frequencies of 31.58%, 15.79% and 10.53% respectively10 .
In the 1970s, gram-negative bacilli were more prevalent than gram-positive bacilli; however, with increased use of cephalosporins and invasive procedures by patients, gram-positive infection has been increasing in the hospital setting. As in the present study, another study17 showed a higher frequency of gram-negative microorganisms (54.86%), followed by gram-positive (24.55%) and Candida (19.43%).
The genus Acinetobacter sp., which has an important characteristic for survival in different types of environment (soil, water, vegeTables, animals, skin and gastrointestinal tract of healthy humans), was the most identified pathogen in the studied cultures, corresponding to 29% of the notification cases, due to their ability to undergo nutritional and metabolic adaptations. The species A. baumannii is an opportunistic microorganism that frequently affects patients in the hospital environment, rarely isolated in the community, in immunocompromised individuals or undergoing invasive procedures, causing bacteremia, respiratory, urinary, soft tissue and meningitis infections. Its pathogenicity relates to its ability to adhere to inanimate surfaces and to form biofilms, susceptibility to antimicrobial resistance and to acquire genetic material from independent genera, resulting in a versatile pathogen, complicated to control and eliminate19)(26 .
Staphylococcus aureus was the most isolated gram-positive microorganism present in 10.5% of the cases and related to infections of the blood and respiratory tract. This is naturally present in the human skin, representing a pathogenic risk when there is a rupture of the skin barrier or immunosuppression18 .
Antimicrobial resistance is an event that affects developed and underdeveloped countries, and the occurrence of multidrug resistance has been increasing in health services and in the community. This problem is aggravated by the lack of innovation for the creation of new antibiotics, with the risk of returning to a pre-antibiotic period27 .
An important factor related to the occurrence of persistent infections and the phenomenon of antimicrobial resistance constitutes the formation of biofilms. It is characterized as a community of bacteria that are organized in a polymeric matrix in the extracellular environment, being able to unite with biotic and abiotic surfaces, increasing its capacity of adaptation in the most diverse environments28 .
The resistance of Klebsiella sp. has an important characteristic that is the antimicrobial resistance intrinsic to ampicillin, because it possesses the chromosomal beta-lactamase (SHV1), guaranteeing ability to resist in the most adverse means of selective pressure by antibiotics29 . This resistance profile was 100% in the present study.
Nevertheless, Klebisiela pneumoniae oxytoca has the K1 enzyme, which has a broader behavior when compared to SHV1, and about 20% of them have the capacity to produce this beta-lactamase and become resistant to all penicillins, cefotaxin, cefetriaxon, aztreonan, but without resistance to carbapenics (30 .
Frequently, infections caused by Pseudomonas aeruginosa are resistant to third- and fourth-generation cephalosporins and carbapenems (such as imipenem and meropenem)18 , corroborating the present study, with a 50% resistance to cefepime and imipenem.
There is a growing increase in the isolation of non-fermenting gram-negative bacteria, such as Acinetobacter and Pseudomonas, which are resistant to third- and fourth-generation cephalosporins, thus carbapenems become the main drug for the treatment of these microorganisms31 , corroborating the research data, which identified 100% resistance of Acinetobacter sp. to ceftazidime, and 90.9%, to ceftriaxone and cefepime. However, the resistance of Acinetobacter sp. to the class of carbapenems currently relates mainly to the production of class D b-lactamases26 . As identified in the present study, in which this pathogen presented resistance to imipenem and meropenem of 72.7% and 63.6%, respectively.
From the above, we can observe that multidisciplinary health team that works in the ICU should have knowledge on the resistance profile of microorganisms in order to raise awareness and allow the adequacy of precautionary measures in addition to adequate medical prescription of antibiotics. The main and most economical measure to be practiced by the team is the constant washing of hands, as they are an important means of conducting pathogens18)(32 .
Nurses play an important role in the success of infection control programs in critical care, as they perform many measures that reduce the risk of infection that are part of their routine, such as handling the vascular catheter, artificial airway and oral hygiene15 . In addition to continuing education activities, active surveillance, epidemiological and antimicrobial and control of multiresistant microorganisms, allowing returning this data to the team32 .
The prescription of antibiotics performed by the intensivist physician consists of a task that requires deep technical and scientific knowledge. For a critical patient, there are several pathophysiological changes due to severe acute disease or sepsis, such as increased capillary permeability, poor volume distribution and increased interstitial space, hepatic and/or renal impairment affecting pharmacokinetics/ pharmacodynamics of antimicrobials. Thus, optimal empirical microbial therapy provides adequate mode of administration and dosage. It should be adapted, if necessary, in the presence of microbiological results of cultures, for reduction of frequency of doses and/or narrowing of the antimicrobial spectrum 15 .
CONCLUSION
The prevalence of Health Care-Related Infection (HCRI) in patients admitted to an intensive care unit (ICU) was 5.3%, representing a lower value than what the literature describes. The analysis of participants' sociodemographic data revealed that most of them were elders and female.
The execution of surveillance cultures in the admissions of patients in the studied ICU is a routine activity, with greater attention to individuals with long hospital stay, from other hospital institutions and with previously diagnosed infection. In the studied group, gram-negative bacteria, especially Acinetobacter sp., the most common pathogen and characterized as an opportunistic microorganism that frequently affects patients in the hospital environment, caused most infections.
Retrospective data collection made it impossible to follow the clinical evolution of the hospitalized patients, regarding changes in the clinical condition after the introduction of the antibiotic, and the need for readjustment of the antibiotics, which would be relevant for discussion, thus configuring a limitation.
The control of HCRI represents a difficult task, requiring joint action of the multiprofessional team that provides assistance to the critical patient, through the hygiene of the hands of professionals, adequacy of materials and equipment, human resources; use of collective and individual protection equipment; disinfection of the environment; epidemiological surveillance, identification of multiresistant pathogens and adequate treatment, continuing education for staff, among other measures that are essential to reduce HCRI rates.
The NICC has a relevant role in the hospital and especially in critical sectors such as the ICU through the standardization of practices and routines necessary to reduce these rates and improve the quality of care.
REFERENCIAS
1. Brasil. Anvisa. Agência Nacional de Vigilância Sanitária. Série: Segura do paciente e qualidade em serviços de saúde. Medidas de prevenção de infecção relacionada à assistência à saúde. 2013; 92. [ Links ]
2. Garcia LM, César ICO, Braga CA, Souza GAAD, Mota EC. Epidemiological profile of hospital infections by multidrug-resistant bacteria in a hospital of northern Minas Gerais (Brazil). Rev Epidemiol Control Infect.2013;3(2):45-49. [ Links ]
3. Brasil. Ministério da Saúde. Portaria n. 2.616, de 5 de novembro de 2002. Dispõe sobre a regulamentação das ações de controle de infecção hospitalar no país. Diário Oficial da República Federativa do Brasil, Brasília (DF). 1998. [ Links ]
4. Abegg PTGM, Silva LL. Hospital infection control in intensive care unit: retrospective study. Semina: Ciências Biológicas e da Saúde. 2011; 32(1): 47-58. [ Links ]
5. Kelly D, Kutney-Lee A, Lake ET, Aiken LH. The critical care work environment and nurse-reported health care-associated infections. American Journal of Critical Care.2013;22(6):, 2013: 482-488. [ Links ]
6. Oliveira AC, Kovner CT, Silva RS. Infecção hospitalar em unidade de tratamento intensivo de um hospital universitário brasileiro. Rev Latino-Am Enfermagem. 2010;18(2):97-104. [ Links ]
7. Brasil. Ministério da Saúde. Documento de referência para o programa nacional de segurança do paciente. Brasília: Ministério da Saúde; 2014. [ Links ]
8. Brasil. Conselho Nacional de Saúde. Resolução nº 466, de 12 de dezembro de 2012. Dispõe sobre pesquisas e testes em seres humanos. Diário Oficial da República Federativa do Brasil. Brasília (DF); 2012. [ Links ]
9. Finger-jardim F, Bosso RP. Prevalência de infecção nosocomial: um estudo retrospectivo em uma unidade de terapia intensiva. Rev Vittalle. 2011;23( 2):57-64. [ Links ]
10. Figueiredo DA, Vianna RPT, Nascimento JA. Epidemiologia da Infecção Hospitalar em uma Unidade de Terapia Intensiva de um Hospital Público Municipal de João Pessoa-PB. Rev bras ci Saúde. 2013;17(3):233-240. [ Links ]
11. Favarin SS, Camponogara S. Perfil dos pacientes internados na unidade de terapia intensiva adulto de um Hospital Universitário. Rev Enferm UFSM. 2012: 2(2):320-329. [ Links ]
12. Nangino GO, Oliveira CD, Correia PC, Machado NM, Dias ATB. Impacto financeiro das infecções nosocomiais em unidades de terapia intensiva em hospital filantrópico de Minas Gerais. Rev Bras Ter Intensiva.2012;24(4):357-361. [ Links ]
13. Gomes AC, Carvalho PO, Lima ETA, Gomes ET, Valença MP, Cavalcanti ATA. Characterization of infections related to health care in the intensive care unit. Rev enferm UFPE on line.2014;8(6):1577-1585. [ Links ]
14. Oliveira AC, Paula AO, Iquiapaza RA, Lacerda ACS. Infecções relacionadas à assistência em saúde e gravidade clínica em uma unidade de terapia intensiva. Rev Gaúcha Enferm. 2012;33(3):89-96. [ Links ]
15. Montero JG, Lerma FA, Galleymore PR, Martínez MP, Rocha LA, Gaite FB et al. Combatting resistance in intensive care: the multimodal approach of the Spanish ICU "Zero Resistance" program. Critical Care. 2015;19(1):114. [ Links ]
16. Ranzani OT, Prina E, Torres A. Pneumonia nosocomial na unidade de terapia intensiva: é possível prever a falha do tratamento? Rev Bras Ter Intensiva. 2014; 26(3): 208-211. [ Links ]
17. Deleri N, Ozayar E, Degerli S, Sahin S, Koç F. Three-year evaluation of nosocomial infection rates of the ICU. Rev Bras Anestesiol. 2013; 63(1):73-84. [ Links ]
18. Barros LM, Bento JNC, Caetano JA, Moreira RAN, Pereira FGF, Frota NM et al. . Prevalência de micro-organismo e sensibilidade antimicrobiana de infecções hospitalares em unidade de terapia intensiva de hospital público no Brasil. Rev Ciênc Farm Básica Apl. 2012; 33(3): 429-435. [ Links ]
19. Howhors A, O'Donoghue M, Feeney A, Sleator RD. Acinetobacter baumannii An emerging opportunistic pathogen. Rev Virulence.2012; 3(3):243-250. [ Links ]
20. Barros SKSA, Kerbauy G, Dessunti EM. Infecção do trato urinário relacionada ao cateter: perfil de sensibilidade antimicrobiana. Rev Rene. 2013;14(4): 1005-1013. [ Links ]
21. Silva NFV, Kimura CA, Coimbra MVS. Perfil de sensibilidade antimicrobiana das Pseudomonas aeruginosa isoladas de pacientes da unidade de tratamento intensiva de um hospital público de Brasília. Rev Revisa. 2012;1(1):19-24. [ Links ]
22. Coelho IC, Silva FL, Nunes MRCM, Lopes LS, Carneiro LP, Ferreira PHPB. Avaliação da suscetibilidade da klebsiella pneumoniae aos betalactâmicos. Rev Epidemiol Control Infect. 2015; 5(2). [ Links ]
23. Marques PB, Carneiro FMC, Ferreira AP. Perfil bacteriano de cultura de ponta de cateter venoso central. Rev Pan-Amaz Saude. 2011:2(1):53-58. [ Links ]
24. Alves, LNS, Oliveira CR, Silva LAP, Gervásio SMD, Alves SR, Sgavioli GM . Hemoculturas: estudo da prevalência dos microrganismos e o perfil de sensibilidade dos antibióticos utilizados em Unidade de Terapia Intensiva. J Health Sci Inst. 2012; 30(1): 44-47. [ Links ]
25. Santos RP, Mariano LG, Takahashi LS, Erdmann MF. Prevalência de infecção hospitalar em unidade de terapia intensiva - um estudo retrospectivo. Rev Enferm UFSM.2014;4(2):410-418. [ Links ]
26. Martins AF, Barth AL. Acinetobacter multirresistente - um desafio para a saúde pública. Rev Scientia Medica. 2013; 23(1):56-62. [ Links ]
27. Fears R, Meulen V. What do we need to do to tackle antimicrobial resistance? Rev The lancet global health. 2014; 2(1):73-84. [ Links ]
28. Macia MD, Rojo-Molinero E, Oliver A. Antimicrobial susceptibility testing in biofilm-growing bacteria. Clin Microbiol Infect.2014; 20(10):981-990. [ Links ]
29. Santana TCFS, Maião RC, Monteiro SG, Carmo MS, Figueiredo PMS. Perfil de resistência de Escherichia coli e klebsiella spp isoladas de urocultura de comunidade do município de São Luis-MA no período de 2005-2008. Rev Patol Trop.2012;41(3):295-303. [ Links ]
30. Perna TDGS, Puiatti MA, Perna DH, Pereira NMM, Couri MG, Ferreira CMD. Prevalência de infecção hospitalar pela bactéria do gênero klebsiella em uma Unidade de Terapia Intensiva. Rev Soc Bras Clin Med. 2015;13(2):119-123. [ Links ]
31. Santos SO, Brezolin D, Honer R. Acinetobacter spp. e Pseudomonas aeruginosa resistentes aos carbapenêmicos no Hospital Universitário de Santa Maria, Rio Grande do Sul. Sci Med.2014;24(2):150-155. [ Links ]
32. Stube M, Herman CTS, Benetti ERR, Stumm EMF. The nurse in the prevention of infection in intensive care. J Nurs UFPE on line.2013;7(12):6989-6997. [ Links ]
Received: March 20, 2017; Accepted: May 27, 2017











 texto en
texto en 



