Meu SciELO
Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Enfermería Global
versão On-line ISSN 1695-6141
Enferm. glob. vol.17 no.52 Murcia Out. 2018 Epub 01-Out-2018
https://dx.doi.org/10.6018/eglobal.17.4.319491
Reviews
Nursing interventions in dermatitis associated to incontinence- integrative literature review
1 PhD, IPP-Portugal; CICS. NOVA. UÉvora Portugal. helenarco@ipportalegre.pt
2 PhD, Professor Coordinator. ICBAS. Retired. Portugal
3 RN, Centro Social e Paroquial de São Tiago - Urra: Unidade de Convalescença e Unidade de Longa Duração e Manutenção, Portugal
4 RN, Santa Casa da Misericórdia de Alter do Chão: Unidade de Média Duração e Reabilitação e Unidade de Longa Duração e Manutenção, Portugal
Introduction:
Dermatitis associated to Incontinence is defined as a damage of the skin connected to the exposure to urine and/or faeces, a type of contact dermatitis, which causes a great discomfort and pain, that has a difficult treatment, extended in time and expensive. The main goal is the identification of the interventions to adopt in the prevention, management and treatment of the dermatitis associated to incontinence.
Methods:
The used method is the integrative review of literature, performed in established data bases: EBSCO host Web - CINAHL Plus, MEDLINE and Bon. The main question of this review was: “Which are the most adequate nursing care to incontinence associated dermatitis?
Results:
Eleven articles were selected and the results were grouped into three dimensions: I. the first presents the characterization of incontinence-associated dermatitis around two categories (definition of incontinence associated dermatitis and differentiation of incontinence / pressure ulcer), II. Related to the issues of diagnosis and evaluation and III. On interventions appropriate to quality care and divided into three categories (prevention, treatment, education and training).
Conclusion:
The comprehensive nature of the integrative review has revealed to us the need for investment in training and adoption of an evidence-based practice that will lead us to a higher quality nursing care.
Keywords: nurse; nurse care; dermatitis associated to incontinence
INTRODUCTION
Incontinence is a common condition, uncomforTable and potentially disabling in the geriatric population. Its predominance is superior in prolonged inpatient facilities and on users that receive long duration care at home that is also one of the main causes of institutionalisation. Sometimes, people are reluctant on discussing the matter because they consider that the incontinence is a part of the aging process1 .
Due to the implications resulting of this situation, the Wound Ostomy and Continence Nurses Society2 and the several editions of the International Consultation on Incontinence3 , namely Abrams et al (2013), they mention continuously the necessity of intervention.
The incontinence can be urinary, faecal or combined. There are several types of urinary incontinence, with different origins, being the most usual of stress, urgency, leakage and functional1 . Getting to understand the typology is crucial to plan the treatment.
It is true that incontinence affects a lot of people especially in the older segments, requiring proper care where the treatment and the intervention needs of an efficient evaluation and diagnosis.
The determination of the compromised function, performing the physical and/or cognitive differentiation is imperative to plan the interventions, where it should be implemented strategies to promote the continence while the conditioning factors are not treated4)(5 .
The interventions may be developed in various dimensions such as the education for health with the change life styles and habits, pyscoemotional and behavioural treatment, as the person is followed by an interdisciplinary team where it is included the systematization of the nursing assistance. During the supervision, it should also be determined the existence of numerous myths associated and accepted by the community, many of them related with food, with the prevalence of the reduction of the ingestion of liquids fallacy to solve the problem, giving origin to the bladder irritation, increasing this way the probability of risk of infection. In the other hand we cannot be unware to the fact of the ingestion of food with caffeine, carbonated drinks, spicy food the acid of some fruit juices, that operate as vesical irritant, increasing the probability of the occurrence of involuntary urinary losses, with all the consequences that come from it4)(5)(6 .
One of the collateral effects may be the development of skin problems, like dermatitis associated to incontinence (DAI) and pressure ulcers (UPP)1)(6 .
DAI is a skin inflammation that occurs when urine and/or faeces get in touch with it. The moisture associated to skin damage may become a problem by the arising of the pH. It is revealed through the presentation of dermatitis signs like erythema, oedema and blisters in the bottom region, causing pain, and it may also occur fungal, bacterial or allergic infections6 .
DAI is documented in clinical practice as a current and persisting problem that is, often, wrongly diagnosed and mistaken with UPP.
Several factors interact in a synergic way to cause iatrogenic skin damage. These situations have an implication with the patients, through the increase of the pain and suffer, as well as for the health system, through the increase of costs and internment duration in the hospital. The structural elements of the health system interact and may affect these results. A positive example is the introduction of financial incentive to prevent UPP7 .
The paradigm shift to a vulnerability appreciation of the patients’ skin integrity, having a particular attention to the elderly, is the most effective way to face the challenges that the health systems endure. A wide and innovative approach of security is critical to handle with the increasing of age and patient’s complexity, the rising of the fiscal challenges and the key expectancy that the health care are safe.
Keeping the patients’ skin integrity is a priority and a challenge for the health professionals, where the nurses have an important role. The structure and the process by which the nursing care are provided may influence the results, thus the need of available scientific evidence, in order to tackle gaps on the provision of care and on the identification of risk factors. It also will be crucial the development of a prevention strategy, treatment and management so that the care may be improved and therefore the patients’ life quality3)(5)(6 .
Supported on this concern, we decided to make a review of the literature having as a main goal identifying the interventions to adopt in the prevention, management and treatment of the dermatitis associated to incontinence.
METHOD
It was developed an integrative review, as it was a way of research that uses several sources of bibliographic information to obtain results and references of various authors, with the aim of substantiate theoretical and scientifically a certain subject through synthesis of knowledge and the incorporation of the results of the work that were found. The review was guided by a set of criteria well defined for the gathering of data, analysis and presentation of results, supporting the process of decision making in health and the phenomena that interfere in it8),(9 , namely: 1) Identification of the problem and formulation of the main question/ hypothesis of research as a starting point (formulation of the question PICO); 2) establishment of inclusion and exclusion criteria of studies, articles or guidelines; 3) Selection of the phenomena of interest to extract of the stablished research; 4) Evaluation of the gathered literature; 5) Interpretation of the results; 6) Synthesis and presentation of the obtained results.
With the aim of obtaining a higher consistency in the research and selection of the intended literature, it was defined two reviewers with academic and scientific experience on the subject, which met with a way to identify and formalize the intended analysis.
After the reflection and discussion about the research subject, it was formulated the main question of this review: Which nursing care are more suiTable to the dermatitis associated to incontinence?.
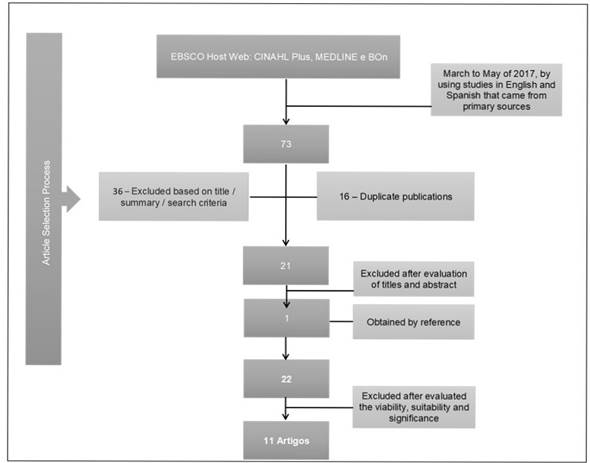
Anchored on the main question, it emerged the research words “nurse”, “nurse care” and “incontinence associated dermatitis”, assisting the research with the Boolean operator “and”, combining this way the various stablished words. These words had in mind the indexation basis and the descriptors MeSH. The bibliographic research was made between March and May of 2017, by using studies in English and Spanish, that came from primary sources. The stablished data bade were EBSCO Host Web: CINAHL Plus, MEDLINE and Bon. As inclusion criteria we stablished: elderly and adults and nursing care to people with dermatitis associated to incontinence. The exclusion criteria that were stablished: children and nursing care on other type of dermatitis.
The exclusion was then made on the basis of title/ abstract/ criteria of research. The time lapse selected was between 2007 and 2017, excluding automatically all the previous articles. The duplicated articles were also eliminated.
From the initial research were identified seventy-three articles, from which thirty-six were excluded by the title, abstract or because they didn’t adjust to the stablished research criteria and sixteen were repeated, and for posterior reading were selected twenty-one. In addition to the twenty-one articles resulting from the initial research, it also turned up an article obtained by reference, gathering twenty-two in the final set for analysis (figure 1 ).
In the execution of this article was observed some ethical questions related with academic integrity principles, by making citations and references, regarding the loyalty to the author10 .
RESULTS
The 22 determined articles were afterwards evaluated according to viability, suitability and significance, defining the evidence level11),(12 .
After a complete and exhaustive reading only eleven were selected for the results acquisition, with two references of level II, one of level V and eight of level VII (figure 2 ).
The results derive from the content analysis made to eleven selected articles, having emerged three dimensions: the first one gives us account of the DAI characterization made in two categories: definition on dermatitis associated to incontinence (A13 , B14 , C15 , D16 , F18 , H20 , I21 , K23 ) and differentiation from DAI/UPP (A13 , B14 , K23 ), the second related to matters of Diagnosis and Evaluation (A13 , B14 , C15 , D16 , I21 ) and the third one linked with the suiTable Interventions to care provision with quality and that subdivided in three categories: Prevention (C15 , E17 , G19 , I21 , J22 ), Treatment (B14 , D16 , I21 ) and Education and Training (F18 , G19 , I21 , K23 ).
DISCUSSION
Definition of dermatitis associated to incontinence
The definition and characterization of dermatitis associated to incontinence was in the majority of the analysed articles, described as a common and visible disturb and that may be considered like a type of contact dermatitis which occurs on patients with urinary incontinence (IU) and/ or faecal. It is usually characterized by a skin irritation that occurs when urine or faeces comes into contact with the perineal area, at times associated with an erythema, pain and uncomforTable dermatological symptoms, causing a significant discomfort and that interferes on the quality of life. Regarding the prevalence, three articles elaborated on the DAI prevalence, referring that in the Japanese elderly14 with incontinence, using diapers or absorbent pad, that DAI prevalence was of 17%. Voegeli15 claims that DAI prevalence varies from 5,6% to 50%, being higher when there is faecal incontinence. He also mentions that is quite common, that doesn’t come as a surprise when it is reported all over the world as a significant problem, given to the large number of affected people, DAI prevention and the management presents an important financial burden for the health systems. Also Payne22 refers that IU affects over 6 million people in the United Kingdom and around 1% of the adults has faecal incontinence, being DAI very common in people that retaining measures (absorbent underpants, pads or diapers), causes discomfort due to the skin damage. Concerning this also Beeckman et al13 mention that patients with faecal incontinence and urinary incontinence are in a higher risk that those that only have urinary incontinence.
The differentiation of dermatitis associated to incontinence/ pressure ulcer
Another category emerging in this dimension was the necessity of making a differentiation between dermatitis associated to incontinence and pressure ulcer.
Such results support other studies already made like Holroyd24 and Campbell, Coyer & Osborne25 . This is because some risk factors of UPP are also cited as risk factors of other iatrogenic skin injuries, like DAI. This is due to the fact of the answer to this potential harmful forces that act out on the skin, being highly influenced by the tissue tolerance and being unique for each individual, as this factor is linked to any iatrogenic skin damage.
Furthermore in the review that we are presenting, three of the articles incorporate registration unities in this category. Starting by the fact that incontinence is a risk factor for the pressure ulcers, but DAI may occur in the absence of any other factor and vice-versa, since moisture is associated to a major coefficient of friction, reducing the tissue tolerance to pressure. In the Sugama, Sanada, Shigeta, Nakagami and Konya14 article, they assume simultaneously that DAI may rise the pressure ulcer risk, since skin weakness rises susceptibility to rubbing and pressure. They point out that moisture damage are complex to distinguish from pressure ulcers in their earlier stadium. In order to make the distinction, it is emphasized, for example, that UPP usually present themselves as a unique injury, circular and symmetrical on a bone prominence and with defined edges. On the other hand, the moisture injuries may have an irregular form, with poorly defined edges, arising frequently in the adipose tissue of the bottom, perineum, and internal parts of the thighs, scrotum and vulva. The differentiation of both is important not only for the selection of a suiTable intervention plan as to report properly the incidence of UPP. The authors point out the importance of the acquisition of the correct history for the determination of the ethology subjacent to the injury. They alert also to the necessity of the implementation of valid tools of observation of injury by moisture to avoid confusion, wrong diagnosis and inadequate treatment or preventive measures. Jacobson, Wright23 , who sustained in a project of practice improvement, expose that after undertake a training, it was verified a significant improvement on DAI classifications on the part of nurses. Also the use of wounds photos helped to reduce the wrong classification and the confusion between DAI and UPP.
A healthy skin has a function of maintaining a physical barrier against the attacks of the external environment, preventing the entrance of harmful and pathogenic substances, functioning as a defence mechanism, acting simultaneously as an important moisture barrier, avoiding the excess in gaining or loosing liquids.
In contrast the urea in the urine may be divided by the skin bacteria to form an ammonia highly alkaline modifying the pH and interrupting in this way the barrier. In a faecal incontinence situation, the changing to a more alkaline pH activates the enzymes in the faeces, increasing the damage caused to the epidermis. When in presence of liquid faeces, richer in digestive enzymes (lipases and proteases), combined with their high content of water, they become particularly damaging to the skin15 .
Diagnosis and evaluation
Five of the analysed articles made reference to diagnosis and DAI evaluation, highlighting the clinical history and tracing the risk factors, are very important, meeting the articles that the International Consultation on Incontinence3 have been disclosing, where they reinforce the need of the realization of the incontinence diagnosis as soon as possible, acting with the goal of treatment and prevention of complications. Beeckman’s et al13 article made a reference to the need of DAI evaluation being incorporated in the skin general evaluation and performed as a part of a program of care in prevention/containment of the pressure ulcer, this evaluation is settled on clinical observation and visual inspection. It was also highlighted the need to be alert to some risk factors to have in mind when someone does an evaluation, namely ins cases of skin of the elderly, since here the barrier function is reduced due to ageing, reducing also the skin resistance to the moisture exposure14),(16 . Simultaneous, the chemical and physical stimulus because of skin cleansing and friction as a mechanical factor, arise the permeability and susceptibility. When an urine loss occurs during resting in bed, women are more susceptible to develop DAI due to their anatomical structure, from the perineum until the coccyx and the sacrococcygeal. In older women, it is also observed a rise of the moisture content and of the pH in the skin of the bottom region as a result of urinary incontinence even without diarrhea. Again, it is enumerated the risk factors for the development of DAI14),(15: faecal/ urinary/ mixed incontinence, the use of occlusive products, weakened skin condition, reduced mobility, diminished cognitive consciousness, incapacity of maintaining a personal hygiene, pain, arise of body temperature, medicine (like steroids and antibiotics), poor nutritional state and severe illnesses. It is also necessary an evaluation with adequate tools15 , presenting as example the Assessment and Intervention Tool (IADIT), Incontinence-associated dermatitis and its severity (IADS), Skin Assessment Tool and Skin Excoriation Tool For Incontinent Patients - Health Improvement Scotland. The author also gives an important contribute for the development of the knowledge of DAI classification: he points 3 stadium, dividing the observation in severity and signals. Being that in I stadium the skin is intact although in risk, presenting a normal appearance when compared to the rest of the body; in II stadium, category 1 of severity, the skin is red but intact, presenting an erythema with or without an oedema; in III stadium, category 2 of severity the skin is red and damaged, presenting vesicle, blisters and erosion or even infection. In the article of Payne21 he draws the attention for the use of inadequate products, for example, those that are not absorbent enough, showing lateral leakage, are too small, are not changed when is necessary and when this change is not followed by the adequate hygiene. Such considerations meet some other studies where it is proved that weakened and damaged skin may evolve to infection, wounds and after to UPP15 .
Nursing interventions
Prevention
DAI prevention must be directed to all the incontinent patients with the goal of promoting positive results and avoiding injuries and damage on the patient. There is also the need to develop protocols for DAI prevention and treatment that should respect two fundamental points related with incontinence situations. These two points are highlighted on work developed in internment environment and in the community, including the evaluation of the incontinence situation (reducing the exposition of the patient’s skin to several agents) and the use of a structure skin care regimen (clean and protect the skin whenever there is an incontinence episode)1)(4)(26 .
Within the prevention, it is verified that “the systematic observation and with the suiTable instruments mobilization “it is fundamental15),(17),(19),(20),(22 , since the approach of a DAI evaluation helps on the patients identification with a high risk of developing complications. It is sustained that the clinical history and complete evaluation, while they are essential for the implementation of an effective treatment plan. There is the need to search for DAI whenever we visit the incontinent patients or being given care, the professionals having the obligation of being particularly aware of this risk, monitoring the pressure areas21 . This an important intervention area of nursing, it will be fundamental to be aware even when the patient refers a simple erythema or a skin rash. In order to make an effective prevention it is also essential the use of materials and adequate techniques having as aim the skin cleansing, hydration and protection. Beeckman et al13 claim that a correct skin cleansing and the use of protective have demonstrated to reduce DAI incidence, being indicated products with similar pH to the skin. This expert panel says that the skin of patients that are incontinent should be cleaned after each elimination episode. The suiTable hygiene is strengthened on several of the selected articles for this review17),(19),(21),(22 . The perianal cleansing should involve products whose pH range doesn´t interfere with the skin integrity (pH between 5,4 and 5,9), pointing out that the frequent washing with water and soap using rubbing as a way to remove dirt, it results in a decrease of this integrity. The use of a regular soap and water is not recommended, because the soap pH is too alkaline e may contribute to the skin irritation.
Concerning the hydration and protection, we verified to be recommended that after cleaning, the skin should be protected against new contact with urine/faeces, involving the use of protective products or of barrier, as emulsions that form a small layer on the surface, repelling potential irritant agents15),(16),(17 . These cleansing products may reduce some adverse effects of soap due to its chemical composition and help in the maintenance of an ideal pH level. They have as a purpose to remove the dirt as well as the irritant substances, apart from being promotors of a good sanitation. Many of which have the ability of hydrate helping to restore and preserve the skin barrier. The protective nowadays mostly use are dimethicone and zinc oxide based17 .
Still in the protection field, the papers made with incontinent people5,(26 advise the use of adequate contention measures, namely underpants, diapers and disposable pads, made of materials superabsorbent that try to maintain the fluids away from skin, being essential the regular change of the dirty products. Also Sugama, Sanada, Shigeta, Nakagami, Konya14 alert, in the context of study made by the authors, to the adequate need of the pad structure. It should be designed to absorb the urine in the frontal area, with the intention of minimize the bottom exposure to urine, while avoids that it flows back to the pad surface. Also Payne20 made a reference to the size and shape of the contention device (pad, diaper), to contain elimination products so that they do not get in contact with the skin.
Treatment
Concerning the treatment of DAI, it was verified the need of evaluation and intervention that should be multi professional, in some cases because it needs a following in dermatology. The DAI severity determines the treatment. In moderate cases, it should kept a clean skin (it may imply the training of caregivers), to verify the need of some other type of absorbent, if they are being used correctly and with a frequent change. In more extreme cases, it should be followed the previous recommendations of hygiene and the establishment of an adequate therapeutic in an infection case. It is also recommended the observation by a specialist in dermatology. The catheterism shouldn’t be used as a preventive measure of long duration, it may although be considered as a short term measure in more severe cases20 .
The treatment of these injuries should also include the skin protection against the additional exposure to irritants and to the establishment of a proper environment to healing16 . Such includes verification of the existence of urinary infection as a cause, the use of suiTable absorbents and with a bigger absorbent capacity, having the necessity of an adequate change. In case of masculine incontinence, it may reach for the use of systems of urinary collection. When the damage on the skin is severe and/or painful, it may be considered the placement of a vesical catheter during the healing process.
Teaching and training
In relation to the teaching and training category, it should and may be done in two fronts, in a way to the professionals and in the other to the patient and caregivers.
In what concerns the professionals, we are alerted to the fact that the urinary and/or faecal incontinence management is often a neglected area, and it may become more as a ritual and less in care based on evidence22 . It is highlighted the need of extra time for the nurses to complete the best practises and education modules and DAI documentation, it is also necessary the proper training to be developed the best care and make a differential diagnosis between DAI and UPP22),(23 .
About the patients and caregivers, it is necessary to guarantee the teaching when the nurses are not there, and it should also be made a previous evaluation, verifying if it is the patient to perform his own hygiene or if it is being made by a caregiver, if they have the ability to do the self-care, if they remain a long time with dirty diapers between changes and if they have knowledge to attend the needs17),(18 . The teaching is though fundamental in the implementation of care, even if they are preventive or healing.
In a general way and as recommended by the Wound, Ostomy and Continence Nurses Society it is key to identify the cause in order to promote the suiTable treatment. It is crucial to maintain the skin dried and clean, using products with a pH similar to the skin and applying barrier products to protect from constant moisture, and to ensure the hydration and protection. The proved hydrant effect is consistent with the evidence of an epidermis well hydrated, reducing the irritation caused by the contact with urine/faeces/moisture.
The elderly are particularly sensitive to damage associated to moisture, due to the change of structure and skin function, they should use products with high capacity of absorption like pads, diapers and cushion underpants that promote the comfort.
In any situation, it is essential to carefully examine the skin, with the aim of differentiate dermatitis from UPP. Beside these, it may occur other skin damage that result from the interaction of several external factors that the person may be subjected, as comorbidities, rubbing forces by mobility limitation, poor nutrition and sensitive and cognitive alterations and in these cases the attention should be increased. It also may have a special care on the patients with mobilization difficulties, because the weight of these products, after the total urine and faeces absorption, when is not changed, may increase the falling risk.
CONCLUSION
DAI is common in people that use contention measures (absorbent underpants, pads or diapers), becoming very uncomforTable by damage caused in the skin, it affects the quality of life. It may be prevented by keeping the skin cleaned. The adoption of a structured skin care regimen is essential to prevention and treatment, so it is necessary a supported evaluation, and it important to verify the type of incontinence, if it only faecal urinary or both, sporadic or complete, to characterize the person and the caregivers (when it is the case). It should exist an intervention plan that includes the evaluation and the management of the incontinence causes, and the care should be directed in three fronts: clean, hydrate and protect the skin before being placed the contention device. It will be also important to ensure the quality of these devices and the teaching to the patient and to the caregiver, as well as to provide the suiTable treatments, mobilizing a multidisciplinary team.
The incontinence prevention and management as well as the associated dermatologic complications are essential in the maintenance and promotion of the quality of life of people and the management of treatment costs for the institutions. As an operating area of nurses, it is necessary a consistence professional, competent and in a suiTable number to reach the goals, it will also be important an investment in training and on the adoption of practice based on the evidence that conducts to the performance of quality care.
REFERENCIAS
1. Sparks M. Incontinence and associated skin care. Long-Term Living. 2011; 60(9): 22-25. Acedido em 3 de maio de 2016. Disponível em: https://www.iadvanceseniorcare.com/print/article/incontinence-and-associated-skin-care [ Links ]
2. Wound, Ostomy and Continence Nurses Society. Role of the wound ostomy continence nurse or continence care nurse in continence care. WOCNS. 2009; Acedido em 3 de dezembro de 2017. Disponível em: http://c.ymcdn.com/sites/www.wocn.org/resource/resmgr/Publications/Role_of_the_WOC_Nurse_or_Con.pdf [ Links ]
3. Abrams P, Cardozo L, Khoury S, Wein A. Incontinence. 5rd International Consultation on Incontinence. International Consultation of Urologic Diseases, International Continence Society, International Society of Urology. 2013; Acedido em 14 de dezembro de 2017. Disponível em: http://www.icud.info/PDFs/INCONTINENCE%202013.pdf [ Links ]
4. Valença M, Albuquerque A. Rocha G, Aguiar A. Cuidados de Enfermagem na Incontinência Urinária: um Estudo de Revisão Integrativa. ESTIMA- Rev Ass Bra de Est. 2016; 14(1): 43-49. Acedido em 14 de dezembro de 2017 em: https://www.researchgate.net/publication/304366242_Cuidados_de_enfermagem_na_incontinencia_urinaria_um_estudo_de_revisao_integrativa [ Links ]
5. Imamura M, Williams K, Wells M, McGrother C. Lifestyle interventions for th e treatment of urinary incontinence in adults. Cochrane Database of Systematic Reviews. 2015; Issue 12. Art. No.: CD003505. [ Links ]
6. Zulkowski K. Diagnosing and Treating Moisture-Associated Skin Damage. Advances in Skin & Wound Care. 2012; 25(5): 231-236. [ Links ]
7. Campbell J, Coyer F, Osborne S. The Skin Safety Model: Reconceptualizing Skin Vulnerability in Older Patients. J Nurs Scholarsh. 2015; 48(1): 14-22. [ Links ]
8. Botelho L, Cunha C, Macedo M. O método da revisão integrativa nos estudos organizacionais. Gestão e Sociedade. 2011; 5(11): 122-136. Acedido a 28 de Outubro de 2016. Disponível em https://www.gestaoesociedade.org/gestaoesociedade/article/view/1220 [ Links ]
9. Sousa L, Marques-Vieira C, Severino S, Antunes, A. A Metodologia de Revisão Integrativa da Literatura em Enfermagem. Revista Investigação em Enfermagem. 2017, Novembro; 21(2): 17-26. [ Links ]
10. Nunes L. Considerações Éticas a atender nos trabalhos de investigação académica de enfermagem. Setúbal: Departamento de Enfermagem ESS|IPS; 2003 [ Links ]
11. The Joanna Briggs Institute. The Joanna Briggs Institute Reviewers' Manual 2015 Methodology for JBI Scoping Reviews. Adelaide, Joanna Broggs Institute. 2015; Acedido em: https://joannabriggs.org/assets/docs/sumari/Reviewers-Manual_Methodology-for-JBI-Scoping-Reviews_2015_v2.pdf [ Links ]
12. Santos D, Silva F, Saldanha E, Lira A, Vitor A. Cuidados de enfermagem ao paciente em pós-operatório de prostatecyomia: revisão integrativa. Rev. Eletr. Enf. [Internet]. 2012-Jul-Set, 14(3): 690-701. Acedido a 16 de dezembro de 2017. Disponível em: https://www.revistas.ufg.br/fen/article/view/14980 [ Links ]
13. Beeckman D, Campbell J, Campbell K, Chimentão D, Coyer F, Domansky R, et al. Proceedings of the Global IAD Expert Panel. Incontinence associated dermatitis: moving prevention forward. Wounds International 2015. Acedido a 6 de Março de 2017. Disponível em: http://www.woundsinternational.com/consensus-documents/view/incontinence-associated-dermatitis-moving-prevention-forward [ Links ]
14. Sugama J, Sanada H, Shigeta Y, Nakagami G, Konya C. Efficacy of an improved absorbent pad on incontinence-associated dermatitis in older women: cluster randomized controlled trial. BMC Geriatrics 2012; 12(22): 1-7. Acedido a 6 de Março de 2017. Disponível em: http://search.ebscohost.com/login.aspx?direct=true&db=mdc&AN=22642800&lang=pt-br&site=ehost-live [ Links ]
15. Voegeli D. Incontinence-associated dermatitis: new insights into an old problem. British Journal Nursing [BJN]. 2016; 25(5): 256-262. Acedido em 7 de Março de 2017. Disponível em: http://search.ebscohost.com/login.aspx?direct=true&db=mdc&AN=26972998&lang=pt-br&site=ehost-live [ Links ]
16. Sampedro M, Varela L, Caro R. Lesiones por humedad. Revision de conocimientos. Revista Enfermería Global. 2015; 14(2), 325-334. Acedido em 18 de Abril de 2017. Disponível em: http://search.ebscohost.com/login.aspx?direct=true&db=lth&AN=110800378&lang=pt-br&site=ehost-live [ Links ]
17. Bianchi J. Top Tips on Avoidance of Incontinence- Associated dermatitis. Wounds UK. 2012; 8(2): S6-S8. Acedido em 28 de Abril de 2017. Disponível em:http://search.ebscohost.com/login.aspx?direct=true&db=ccm&AN=104406110&lang=pt-br&site=ehost-live [ Links ]
18. Beldon P. Incontinence-associated dermatitis: protecting the older person. British Journal of Nursing [BJN]. 2012; 21(7), 402-407. Acedido em 5 de Maio de 2017 em: http://search.ebscohost.com/login.aspx?direct=true&db=mdc&AN=22585017&lang=pt-br&site=ehost-live [ Links ]
19. Beeckman D, Verhaeghe S, Defloor T, Schoonhoven L, Vanderwee, K. A 3-in-1 perineal care washcloth impregnated with dimethicone 3% versus water and pH neutral soap to prevent and treat incontinence-associated dermatitis: a randomized, controlled clinical trial. Journal Of Wound, Ostomy, and Continence Nursing: Official Publication Of The Wound, Ostomy And Continence Nurses Society [JWOCN]. 2011; 38(6): 627-634. Acedido em 19 de Março de 2017. Disponível em http://search.ebscohost.com/login.aspx?direct=true&db=mdc&AN=21952346&lang=pt-br&site=ehost-live [ Links ]
20. Payne D. Managing and preventing incontinence-associated dermatitis. British Journal of Community Nursing. 2015- Maio; 20(5), 231-233. Acedido em 2 de Maio de 2017. disponível em: http://search.ebscohost.com/login.aspx?direct=true&db=mdc&AN=25993371&lang=pt-br&site=ehost-live [ Links ]
21. Payne D. Not just another rash: management or incontinence-associated dermatitis. British Journal of Community Nursing. 2016- Setembro; 21(9), 434-440. Acedido em 6 de Maio de 2017. Disponível em: http://search.ebscohost.com/login.aspx?direct=true&db=mdc&AN=27594057&lang=pt-br&site=ehost-live [ Links ]
22. Baadjies R, Karrouze I, Rajpaul K. Using no-rinse skin wipes to treat incontinence-associated dermatitis. British Journal of Nursing. 2014; 23(20): 22 - 28. Acedido em 23 de Abril de 2017. Disponível em http://search.ebscohost.com/login.aspx?direct=true&db=ccm&AN=103916375&lang=pt-br&site=ehost-live [ Links ]
23. Jacobson T, Wright T. Improving Quality by Taking Aim at Incontinence-Associated Dermatitis in Hospitalized Adults. Medsurg Nursing. 2015 Maio-Junho; 24(3): 151-157. Acedido em 2 de Maio de 2017. Disponível em: http://search.ebscohost.com/login.aspx?direct=true&db=mdc&AN=26821450&lang=pt-br&site=ehost-live [ Links ]
24. Holroyd S. Incontinence-associated dermatitis: identification, prevention and care. British Journal of Nursing [BJN]. 2015; 24(9): 37-43. Acedido em 3 de maio de 2017. Disponível em: http://search.ebscohost.com/login.aspx?direct=true&db=mdc&AN=25978474&lang=pt-br&site=ehost-live [ Links ]
25. Campbell J, Coyer F, Osborne S. The Skin Safety Model: Reconceptualizing Skin Vulnerability in Older Patients. J Nurs Scholarsh. 2016 Jan; 48(1):14-22. 2015-Outubro; 14-22. Acedido em 3 maio de 2017. Disponível em: http://onlinelibrary.wiley.com/doi/10.1111/jnu.12176/pdf [ Links ]
26. Nazarko Linda. Use of continence pads to manage urinary incontinence in older people. British Journal of Community Nursing. 2015 - agosto; 20(8):378-384. Acedido em 14 de dezembro de 2017. Disponível em: http://web.a.ebscohost.com/ehost/pdfviewer/pdfviewer?vid=11&sid=9331752b-579e-40ec-af19-06cf290b5767%40sessionmgr4008 [ Links ]
Received: January 25, 2018; Accepted: March 03, 2018











 texto em
texto em