Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Enfermería Global
versión On-line ISSN 1695-6141
Enferm. glob. vol.18 no.53 Murcia ene. 2019 Epub 14-Oct-2019
https://dx.doi.org/10.6018/eglobal.18.1.302341
Articles
ICU admissions for obstetric causes
1Nurse. Specialist in Intensive Care by the School of Public Health of Ceará (ESP/CE). Fortaleza, CE, Brazil.
2PhD student in Nursing from the Federal University of Ceará (UFC). Fortaleza, CE, Brazil.
3PhD student in Clinical Care in Nursing and Health at the State University of Ceará (UECE). Fortaleza, CE, Brazil.
4Master student in Clinical Care in Nursing and Health from the State University of Ceará (UECE). Fortaleza, CE, Brazil.
5Nurse graduated from the Metropolitan College of Grande Fortaleza (FAMETRO). Fortaleza, CE, Brazil.
Theobjectivewas to analyze the admission of women of childbearing age to an Obstetric Intensive Care Unit. A cross-sectional, documentary and retrospective study was carried out in an Obstetric Intensive Care Unit, located in Fortaleza/Ceará, with women of childbearing age admitted to the unit in 2016. Data were collected from 106 medical records that met the inclusion criteria during the month of April 2017, using a semi-structured form, and analyzed by means of descriptive statistics. The majority of the women were between 20 and 29 years old, common-law married, with complete secondary education, primiparous, had initiated prenatal care in the first trimester of pregnancy, and attended 4 to 6 consultations. Among the direct obstetric causes (61.1%), the most frequent were Eclampsia (34.4%), HELLP syndrome (15.1%) and Severe preeclampsia (11%). The indirect obstetric causes (38.9%) included Renal insufficiency (13.5%), Acute lung edema (11.5%) and Heart disease (9.6%). Data revealed a fragile health care for women within the pregnant-puerperal cycle.
Keywords: Intensive Care Units; Obstetrics; Health profile
INTRODUCTION
Approximately 73% (1,771,000 out of 2,443,000) of all maternal deaths worldwide occurred due to direct obstetric causes. Indirect obstetric causes, in turn, accounted for 27.5% (672,000). Hemorrhage (27.1%), hypertensive disorders (14%) and sepsis (10.7%) were the main obstetric causes of maternal deaths1. Direct obstetric causes are disease that are typical of the pregnant‐puerperal cycle; indirect causes are the complications of diseases existing before pregnancy2.
In Brazil, in the last two decades, there has been a 51% reduction in the number of maternal deaths. However, like other Latin American countries, Brazil did not presented favorable conditions for achieving the goal of reducing maternal mortality rate by 75% until the year 2015, as expressed in the United Nations Millennium Declaration. Such change was not possible due to the precarious health care conditions associated with preexisting chronic diseases, which become obstetric risks during the pregnancy. Thus, maternal death is considered a conundrum for collective health and a worrying public health problem, because the epidemiological indices remain high in the Brazilian territory3)(4.
In the state of Ceará, in 2014, the obstetric causes of maternal death included 30% of hypertensive syndromes, 15% of complications during labor, 11% of hemorrhage and puerperal infections, 8% of abortion, 6% of Embolism and 19% of other direct obstetric causes5.
Regarding the obstetric complications of hospitalization of women during gestation in the state of Paraná in 2010, the main were the lower urinary tract infection (31.0%), systemic arterial hypertension (9.2%), altered glycemic levels (13.1%) and premature rupture of the membranes (34%). Critical clinical conditions of women during pregnancy, childbirth, abortion and puerperium and the need for specific care to reduce the risk of health problems lead to the admission of these women to Obstetric Intensive Care Units (ICU)6.
In order to minimize these epidemiological indices and reduce the number of maternal deaths in Brazil, the Ministry of Health (MH) created strategies to reach the 5thmillennium goal, with emphasis on the creation of the Stork Network in 2011 that has as one of its objectives the decrease of maternal and infant mortality, particularly in the neonatal component7.
Follow-up of pregnant women through prenatal care, with at least 6 consultations, as recommended by the Ministry of Health, related to specific tests during pregnancy, maternal immunization, nutritional support appropriate to this clientele, and early identification and treatment of diseases, are essential for avoiding diseases and maternal and neonatal risk during pregnancy8.
The role of nurses during prenatal care is important because they are the health professionals that are closer to the patients and have the ability to create bonds with them. In the case of pregnant women, they have a holistic view of the woman, and gestation is not the single focus of the nursing consultation. Nurses seek to support these women in their anxieties, fears, desires and they clarify their doubts9)(10. They are also important professionals in health promotion and disease prevention11.
The motivation to develop the present research emerged from reading on the theme in scientific journals that regard obstetric causes as the main responsible for admissions of women to ICUs and the high rate of maternal mortality. This reading sharpened the interest in knowing the reality regarding obstetric causes of hospitalization and risk of maternal death or near miss. In addition, the theme studied contemplates the National Agenda of Health Research Priorities in Brazil - ANPPS12.
Thus, the objective was to analyze the admissions of women of childbearing age to an Obstetric Intensive Care Unit.
METHOD
This is a cross-sectional, documentary and retrospective study. The research site was an Obstetric ICU belonging to a University Hospital Complex located in Fortaleza/Ceará, Brazil.
The research population consisted of women of childbearing age admitted to the obstetric ICU during the year 2016. The total number admissions of women to this sector were 229, of which 189 were due to obstetric causes. However, only 106 medical records were located by the Medical and Statistical Archive Service (SAME), which represented the final sample of the study. It was not possible to perform a new search of the missing medical records due to the established collection period. The inclusion criteria used were: Hospitalizations of women of childbearing age in the obstetric ICU with health problems that are exclusive of the pregnant-puerperal cycle in the year 2016; women with an outcome of the period of hospitalization (death; transfer to another sector or health unit; hospital/medical discharge or discharge upon request); information on hospitalizations present in ICU record books during the year 2016; and presence of medical records in the SAME. The missing medical records were excluded from the present study.
Data were collected during April 2017 from medical records using a semi-structured form with open and closed questions on sociodemographic, clinical and obstetric variables. The form was prepared by the researcher.
The collected data were tabulated in a Microsoft Excel spreadsheet. After data collection and tabulation, statistical analyses were started, using the double typing technique, and using the Statistical Package for the Social Sciences (SPSS) for Windows version 23.0. They were then organized into Tables and graphs and analyzed using descriptive statistics, evaluating frequencies, means and percentages. The Chi-square (X2) and Likelihood Ratio (LR) tests were applied.
The study was submitted to the MEAC's Ethics and Research Committee (REC) and approved by the Research Commission assigned by the institution, under CAAE 65067417.9.0000.5037, according to the National Health Council (NCH), through Resolution 466 of December 12, 201213.
RESULTS
The information of 106 medical records was incomplete and this made it difficult to accurately interpret the data.
With regard to the sociodemographic profile of the participants, it was observed that the majority was between 20 and 29 years old, with a mean of 24 ± 6.5 years, were common-law married, brown, came from Fortaleza and were originally from the countryside of Ceará, had completed secondary education, did not perform paid activities, and had no children. These data are shown inTable 1.
Table 1. Sociodemographic characterization of study participants. Fortaleza-Ceará-Brazil, 2017.

Source:Direct search
Regarding the clinical characterization of the study participants, the data showed that there was prevalence of 1 to 3 gestations, with a mean of 1; primiparity; absence of history of abortion; and non-submission to procedures in previous pregnancies because they were mostly in the first gestation at the moment in which the data were recorded. With regard to prenatal care, the participants started attending consultations in the 1stgestational trimester; attended 4 to 6 consultations, with a mean of 6.2 ± 2.3. However, in 46 medical records, there was no record of the month of start of prenatal care, neither of the number of consultations, intercurrences and hospitalizations during the pregnancy cycle. At the time of admission to the ICU, the majority of the women was in the immediate puerperium and remained in the sector between 0 and 10 days, according toTable 2.
Table 2. Clinical characterization of study participants. Fortaleza-Ceará-Brazil, 2017.

Source:Direct search
Eclampsia (34.4%), HELLP Syndrome (15.1%), and Severe Preeclampsia (SPE) (11%) were identified as groups of direct obstetric causes (61.1%). As for obstetric indirect causes (38.9%), there were seven groups, the more important being Renal insufficiency (13.5%), Acute pulmonary edema (11.5%), and Heart disease (9.6%).
Table 3. Distribution of direct and indirect obstetric causes of ICU admission. Fortaleza-Ceará-Brazil, 2017.
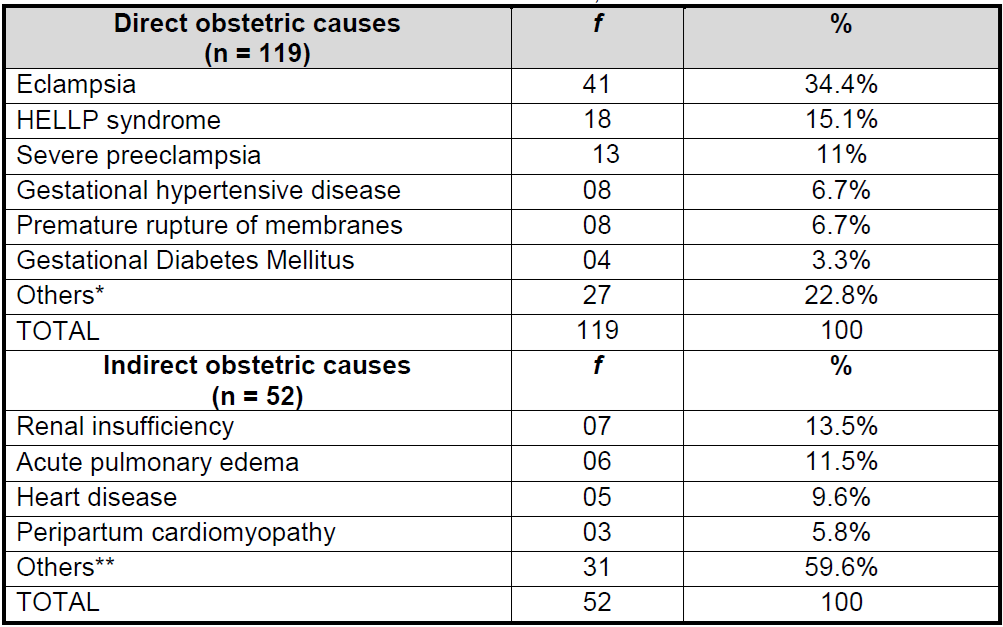
*Uterine rupture, Uterine suture, Cesarean section, Prolonged gestation, Premature rupture of ovary membranes, Gestation of 28 weeks, Premature rupture of Amniotic membrane, Premature labor, Postpartum hemorrhage, Severe vaginal bleeding, Abortion, Fetal death, Maternal instability, Placenta previa, Post-operative immediate delivery, Laceration, Curettage, Uterine atony, Fetal distress.
**Hemoperitoneum, Malloy Weiss Syndrome, Thyrotoxic Syndrome, Chung Staus Syndrome, Electrolyte disorders, Deep vein thrombosis, Pulmonary thromboembolism, Hemorrhagic shock, Chronic Obstructive Pulmonary Disease, Respiratory Arrest, Pyelonephritis, Appendicitis, Bacterial Meningitis, Anemia, Hyperthyroidism, H1N1, Epilepsy, Peripartum heart failure, Hemorrhagic stroke, Hypovolemic shock, Rheumatic heart disease, Mitral and aortic insufficiency, Monitoring of penicillin sensitization, Hypovolemia, Hypotension, Hypothyroidism, Liver dysfunction, Sepsis, Pneumonia.
Source:Direct search
Regarding the clinical outcomes of the study participants during the ICU stay, the majority (77%) was transferred to another sector, 13% had hospital/medical discharge and there were only 4% of cases of maternal death, according to theGraph 1.

Source: Direct search
Graph 1. Clinical outcomes of study participants. Fortaleza-Ceará-Brazil, 2017.
Between the association between the clinical outcome death and sociodemographic and clinical characteristics of the participants, it was observed that cases of maternal deaths were not directly associated with age, schooling, parity, initiation of prenatal care, number of consultations, obstetric causes, and length of stay in the ICU. However, there was a relationship between the causes of deaths and complications during ICU stay, according toTable 4.
DISCUSSION
The present research, concerning sociodemographic aspects, corroborates a study carried out in 2012 in the same municipality of Fortaleza in a Public Hospital ICU in which the participants were predominantly in the age group of 20 to 34 years (52.7%), originally from the countryside of the state of Ceará (50%), married (55.56%), with more than 8 years of schooling (58.3%), and did not perform paid activities (83.3%)14.
In a cohort study developed in British Columbia, Canada, between 2005 and 2010 depicting maternal morbidity and perinatal outcomes among rural versus urban women, there was an association between death or severe maternal morbidity and rural residence15). It is believed that pregnant and puerperal women living in the countryside of the state of Ceará have difficulties to access services of greater complexity and technological density; they are referred to the capital when there is a complication and/or health problem. However, even women residing in places where more complex obstetric care is available may have complications due to prevenTable causes.
The level of education of women is a conditioning factor to prenatal care adherence. Low maternal schooling is associated with the emergence of risk situations for the mother/child binomial. It is assumed that the higher the level of schooling, the greater is the understanding of the need for specific care during pregnancy, as well as the early onset of prenatal care16.
Regarding the clinical data, a prevalence of primiparous women (52.8%) was identified in this study .These women started prenatal care in the first trimester (41.5%), and attended 4 to 6 consultations (31.1%), with a mean of 6.2 ± 2.3 consultations.
These data are reinforced by a study on the clinical profile of primiparous women treated in a high-risk maternity hospital in which 52 (71.2%) women started prenatal care in the 1stgestational trimester; 34 (46.6%) attended 4 to 6 prenatal consultations, and 32 (43.8%) attended 7 or more; 73 were primiparous women; only 6 (8.2) required ICU care, and they remained in the sector for 1 to 5 days17. The variable ICU care differed from the findings of the present study, in which 100% of the women had been admitted to the ICU, of which 66% were in the immediate puerperium (66%), and remained in the sector for 0 to 10 days (93.4%). This fact is explained by the fact that this hospitalization period is conducive to the recovery from complications that arose during the immediate or late puerperium, to the detriment of obstetric causes18.
Regarding prenatal consultations, these should happen in a monthly basis up to the 28thweek of gestation, biweekly between the 28thand 36thweek, and weekly in the end19, totaling at least 6 regular and complete consultations.
Direct and indirect obstetric causes may lead women during the pregnant-puerperal cycle to need ICU care because gestation causes organic changes that require greater attention and specialized assistance.
Obstetric causes of admission to the ICU showed that Eclampsia 41 (34.4%) was the main direct obstetric cause, followed by HELLP syndrome 18 (15.1%) and Severe preeclampsia 13 (11 %). As indirect causes, Renal insufficiency 07 (13.5%), Acute pulmonary edema 06 (11.5%) and Heart disease 05 (9.6%) prevailed.
These findings are in line with a previous study performed in the same intensive care unit where the main obstetric causes of hospitalization were Hypertensive syndromes 198 (53%), of which 69 (17.7%) were eclampsia and 66 (17%) severe preeclampsia. Cardiac problems 35 (9%) were also significant for admission20. However, it should be considered that this research was carried out from January 2012 to December 2014, while the data of the present study refer only to the year 2016.
In Recife, more than half of the women admitted to a reference obstetric ICU in the year 2014 had a sociodemographic profile of low schooling and a clinical profile of first pregnancy and cesarean history, with complications responsible for maternal near miss, which in these cases were caused by premature births and acute thrombocytopenia associated with gestational hypertensive disorders, such as HELLP syndrome21.
In a control case study in Pernambuco, hypertensive disorders 17 (22.7%) were the main direct obstetric cause and AIDS 57 (9.4%) was the indirect obstetric cause of admission to obstetric ICU22.
In the South of Brazil, between 2005 and 2009, 775 women of childbearing age were admitted to obstetric ICUs; obstetric complications accounted for 12.3% of these hospitalizations. Among the complication, gestational hypertension syndromes were the most frequent, representing 71.3% of the cases and accounting for 31.3% compared to other obstetric causes23.
In an ambidirectional cohort study performed with patients admitted to the obstetric ICU of the Institute of Comprehensive Medicine of Recife between 2005 and 2010, the main causes of hospitalization in the pregnant-puerperal cycle were heart disease 88 (17.6%), followed by deep venous thrombosis (DVT) 55 (11%) and acute pulmonary edema 30 (6%)24.
Despite the significant reduction in the maternal mortality rate by 43 per cent from 1990 to 2013 worldwide, it is estimated that 303,000 women die each year from complications of pregnancy and childbirth25. Brazil achieved the same reduction for the period analyzed4.
Regarding clinical outcome, 77% of the women admitted to the obstetric ICU were transferred to another sector, mainly the nursing ward, 13% were discharged from hospital, and only 4% died. The death rate of other Brazilian studies ranged from 2.2%26to 20%18.
An analysis performed with women hospitalized for obstetric causes in an ICU of a Public Hospital in Paraná presented a higher rate of maternal mortality, in which 20% died. This fact can be justified by the number of consultations which was low, and in order to convey enough information, the content was addressed with more emphasis18. The main causes for maternal death were age between 16 and 43 years (mean of 28.7 years and standard deviation - SD = 7.5), common-law marriage, brown skin color (69.7%), no paid activity, low schooling and non-realization of prenatal care (17%); and 26.2% had six or more prenatal consultations22.
With respect to the association between clinical outcome and complications during hospitalization in the ICU, no association with age group and number of prenatal consultations was observed. There was an association with complications during hospitalization, with ap-value of 0.02. These women died despite the short hospitalization time, in which the first case died on the first day of hospitalization, the second remained for 6 days, and the last two women remained only one day. The four women had the same complication: non-reversed cardiorespiratory arrest.
A study of the causes of maternal mortality according to levels of hospital complexity showed that in the reference hospitals for high-risk pregnancies, the direct obstetric causes of maternal deaths were: pre-eclampsia/eclampsia (28 cases), urinary tract infection (15), puerperal infection (12) and abortion (12). In the reference hospitals for low-risk pregnancies, they were hemorrhage (21), embolism (12) and anesthetic complications8. The number of maternal deaths (48) from indirect obstetric causes was higher in reference hospitals for high-risk pregnancies. The study also concluded that Brazilian women are subject to death due to causes already controlled in many countries, especially the most developed countries27.
In the United States, primary and secondary chronic hypertension is the main obstetric cause of admission of women to hospitals during pregnancy, and it is strongly associated with adverse outcomes of the pregnant-puerperal cycle, especially maternal death28.
CONCLUSION
We conclude that the prevalent sociodemographic profile of the women was age group from 20 to 29 years (50.9%), brown skin color (92.5%), common-law marriage (40.5%), complete high school (35.8%) and absence of paid activities (43.4%). Regarding the clinical profile, they were primiparous (52.8%), started prenatal care in the first trimester of pregnancy (41.5%), and attended from 4 to 6 (31.1%) consultations, with a mean of 6.2 ± 2.3.
Most of the participants in the study were admitted to the ICU for direct obstetric causes (61.1%), with the most prevalent being Eclampsia (34.4%), HELLP Syndrome (15.1%) and SPE (11%). Indirect obstetric causes (38.9%) included Renal insufficiency (13.5%), Acute pulmonary edema (11.5%) and Heart disease (9.6%). The main clinical outcome was transfer to another sector (77%). There was a low maternal mortality rate (4%), but with a significant association between deaths and complications during the ICU stay,p-value 0.002.
The limitating factors of the study were: incomplete or non-provision of information on the procedures of previous pregnancies, number of prenatal consultations, initiation of prenatal care, number of hospitalizations, and number of complications during pregnancy as well as other sociodemographic and clinical data and the non-location of medical records by SAME.
The data revealed a fragile health care for women within the pregnant-puerperal cycle. The identification of this collective health problem can contribute to the formulation and support to public policies, health management strategies, and professionals engaged in the planning and implementation of actions aimed at preventing complications and consequent death of women of productive age.
REFERENCIAS
1. Say L, Germmill A, Tuncalp O, Moller AB, Daniels J, Gulmezoglu AM, et al. Global cause of maternal death: a WHO systematic analysis. The Lancet Global Health [Internet]. 2014 [acesso em 2017 fev 02]; 2(6): 323-333. Disponível em: http://www.thelancet.com/journals/langlo/article/PIIS2214-109X(14)70227-X/abstract. [ Links ]
2. Botelho NM, Silva IFMM, Tavares JR, Lima LO. Causas de morte materna no Estado do Pará, Brasil. Rev Bras Ginecol Obstet [Internet]. 2014 [acesso em 2017 fev 02]; 36(7): 290-295. Disponível em: http://www.scielo.br/pdf/rbgo/v36n7/0100-7203-rbgo-s0100-720320140004892.pdf. [ Links ]
3. Brasil. Ministério da Saúde. Secretaria de Vigilância em Saúde. Departamento de Análise de Situação de Saúde. Saúde Brasil 2011: uma análise da situação de saúde e a vigilância da saúde da mulher. Ministério da Saúde, Secretaria de Vigilância em Saúde, Departamento de Análise de Situação de Saúde. Brasília: Editora do Ministério da Saúde, 2012 [acesso em 2017 fev 02]. Disponível em: http://bvsms.saude.gov.br/bvs/publicacoes/saude_brasil_2014_analise_situacao.pdf. [ Links ]
4. Brasil. Portal Brasil. OMS: Brasil reduz mortalidade materna em 43% de 1990 a 2013 [acesso em 2016 jul 20]. Disponível em: http://www.brasil.gov.br/saude/2014/05/oms-brasil-reduz-mortalidade-materna-em-43-de-1990-a-2013. [ Links ]
5. Ceará. Informe Epidemiológico Mortalidade Materna [acesso em 2015 nov 2015]. 2015. Disponível em: http://www.saude.ce.gov.br/index.php/boletins#. [ Links ]
6. Veras TCS, Mathias TAF. Principais causas de internações hospitalares por transtornos maternos. Rev Esc Enferm USP [Internet]. 2014 [acesso em 2017 fev 02]; 48(3): 401-408. Disponível em: http://www.scielo.br/pdf/reeusp/v48n3/pt_0080-6234-reeusp-48-03-401.pdf. [ Links ]
7. Brasil. Portaria n 1.459, de 24 de junho de 2011. Institui, no âmbito do Sistema Único de Saúde - SUS - a Rede Cegonha. Diário Oficial da República Federativa do Brasil, 8. Brasília, DF, 2011 [acesso em 2015 nov 15]. Disponível em: http://dab.saude.gov.br/portaldab/smp_ras.php?conteudo=rede_cegonha. [ Links ]
8. Souza MAC, Souza THSC, Gonçalves AKS. Fatores determinantes do near miss materno em uma unidade de terapia intensiva obstétrica. Rev Bras Ginecol Obstet. [Internet]. 2015 [acesso em 2017 fev 02]; 37(11): 498-504. Disponível em: http://www.scielo.br/pdf/rbgo/v37n11/0100-7203-rbgo-37-11-00498.pdf. [ Links ]
9. Guerreiro EM, Rodrigues DP, Silveira MAM, Lucena NBF. O cuidado pré-natal na atenção básica de saúde sob o olhar de gestantes e enfermeiros. Rev. Min. Enferm., [Internet]. 2012 [acesso em 2017 fev 02]; 16(3): 315-323. Disponível em: http://reme.org.br/artigo/detalhes/533. [ Links ]
10. Barreto CN, Ressel LB, Santos CC, Wilhelm LA, Silva SC, Alves CN. Atenção pré-natal na voz das gestantes. Rev Enferm UFPE [Internet]. 2013 [acesso em 217 fev 09]; 7(6): 4354-4363. Disponível em: http://www.revista.ufpe.br/revistaenfermagem/index.php/revista/article/view/4355/pdf_2724. [ Links ]
11. Martins QPM, Ferreira GSM, Aragão AEA, Gomes FMA, Araújo LM, Ferreira FISl. Conhecimentos de gestantes no pré-natal: evidências para o cuidado de enfermagem. Sanare [Internet]. 2015 [acesso em 2017 fev 08]; 14(02): 65-71. Disponível em: https://sanare.emnuvens.com.br/sanare/article/viewFile/827/498. [ Links ]
12. Brasil. Ministério da Saúde. Secretaria de Ciência, Tecnologia e Insumos Estratégicos. Departamento de Ciência e Tecnologia. Agenda nacional de prioridades de pesquisa em saúde. Brasília : Editora do Ministério da Saúde, 2015. Disponível em: http://brasil.evipnet.org/wp-content/uploads/2017/07/ANPPS.pdf. [ Links ]
13. Brasil. Conselho Nacional de Saúde. Resolução nº466. Normas regulamentadoras de pesquisas envolvendo seres humanos. Brasília; 2012. Disponível em: http://conselho.saude.gov.br/resolucoes/2012/Reso466.pdf. [ Links ]
14. Souza CF, Okubo BMR, Pontes DS, Silva DHM, Viana MCC, Correia JW. Perfil clínico-demográfico de pacientes em ciclo grávido-puerperal admitidas em uma Unidade de Terapia Intensiva em Fortaleza. Rev Saúde Públ. [Internet]. 2015 [acesso em 2017 fev 08]; 8(1): 30-42. Disponível em: http://esp.saude.sc.gov.br/sistemas/revista/index.php/inicio/article/viewFile/272/288. [ Links ]
15. Lisonkova S, Haslam MD, Dahlgren L, Chen I, Synnes AR, Lim KI. Maternal morbidity and perinatal outcomes among women in rural versus urban áreas. CMAJ [Internet]. 2016 [acesso em 2017 fev 10]; 188: 17-18. Disponível em: http://www.cmaj.ca/content/early/2016/09/26/cmaj.151382.abstract. [ Links ]
16. Rezende CL, Souza JC. Qualidade de vida das gestantes de alto risco de um centro de atendimento à mulher. Psicólogo informação [Internet]. 2012 [acesso em 2017 fev 10]; 16(16): 45-69. Disponível em: http://pepsic.bvsalud.org/pdf/psicoinfo/v16n16/v16n16a03.pdf. [ Links ]
17. Moraes PGS, Holanda VR, Pinheiro HDM. Perfil epidemiológico de primíparas atendidas em uma maternidade de alto risco. Enfermagem Obstétrica [Internet]. 2014 [acesso em 2017 fev 10]; 1(2): 45-50. Disponível em: http://www.enfo.com.br/ojs/index.php/EnfObst/article/view/9. [ Links ]
18. Tonin KA, Oliveira JLC, Fernandes LM, Sanches MM. Internação em unidade de terapia intensiva por causas obstétricas: Estudo em hospital público de ensino. Rev Enferm. [Internet]. 2013 [acesso em 2017 fev 10]; 3(3): 518-527. Disponível em: https://periodicos.ufsm.br/reufsm/article/view/9157/pdf. [ Links ]
19. Brasil. Ministério da Saúde. Secretaria de Atenção à Saúde. Departamento de Atenção Básica. Atenção ao pré-natal de baixo risco. Brasília: Editora do Ministério da Saúde, 2012. [ Links ]
20. Saintrain SV, Oliveira JGR, Saintrain MVL, Bruno ZV, Borges JLB, Daher EF et al. Fatores associados à morte materna em unidade de terapia intensiva. Rev Bras Ter Intensiva. [Internet]. 2016 [acesso em 2017 fev 10]; 28(4): 397-404. Disponível em: http://www.scielo.br/pdf/rbti/v28n4/0103-507X-rbti-28-04-0397.pdf. [ Links ]
21. Oliveira LC, Costa AAR. Near miss materno em unidade de terapia intensiva: aspectos clínicos e epidemiológicos. Rev Bras Terapia Intensiva [Internet]. 2015 [acesso em 2017 fev 11]; 27(3): 220-227. Disponível em: http://www.scielo.br/pdf/rbti/v27n3/0103-507X-rbti-20150033.pdf. [ Links ]
22. Leite RMB, Araújo TVB, Albuquerque RM, Andrade ARS, Neto PJD. Fatores de risco para mortalidade materna em área urbana do Nordeste do Brasil. Cad Saúde Pública [Internet]. 2011 [acesso em 2017 fev 11]; 27(10): 1977-1985. Disponível em: http://www.scielo.br/pdf/csp/v27n10/11.pdf. [ Links ]
23. Agnolo CMD, Gravena AAF, Romerio-Lopes TC, Rocha-Brischiliari SC, Carvalho MD Barros, Pelloso SM. Mulheres em idade fértil: causas de internação em Unidade de Terapia Intensiva e resultados. ABCS Health Sci. [Internet]. 2014 [acesso em 2017 fev 02]; 39(2): 77-82. Disponível em: https://www.portalnepas.org.br/abcshs/article/view/626/641. [ Links ]
24. Coêlho MAL, Coutinho LK, Coutinho I, Hofmann A, Miranda L, Amorim M. Perfil de mulheres admitidas em uma UTI obstétrica por causas não obstétricas. Rev Assoc Med Bras.[Internet]. 2012 [acesso em 2017 fev 02]; 58(2): 160-167. Disponível em: http://www.scielo.br/pdf/ramb/v58n2/v58n2a11.pdf. [ Links ]
25. World Health Organization. Maternal mortality. 2016 [acesso em 2017 jul 15]. Disponível em: http://www.who.int/mediacentre/factsheets/fs348/en/. [ Links ]
26. Medeiros TMC, Visgueira AF, Moraes HMPL, Araujo KRS, Ribeiro JF, Crizóstomo CD. Perfil das pacientes admitidas na unidade de terapia intensiva obstétrica de uma maternidade pública. Revista de Enfermagem UFPE [Internet]. 2016 [acesso em 2017 fev 12]; 10(10):3876-82. Disponível em: http://www.revista.ufpe.br/revistaenfermagem/index.php/revista/article/view/3685. [ Links ]
27. Soares VMN, Souza KV, Azevedo EMM, Possebon CR, Marques FF. Causas de mortalidade materna segundo níveis de complexidade hospitalar. Rev Bras Ginecol Obstet.[Internet]. 2012 [acesso em 2017 fev 02]; 34(12): 536-543. Disponível em: http://www.scielo.br/pdf/rbgo/v34n12/02.pdf. [ Links ]
28. Bateman BT, Bansil P, Hernandez-Diaz S, Mhyre JM, Callaghan WM, Kuklina EV. Prevalence, trends, and outcomes of chronic hypertension: a nationwide sample of delivery admissions. American journal of obstetrics and gynecology [Internet]. 2012 [acesso em 2017 fev 08]; 206: e1-e8. Disponível em: https://www.ncbi.nlm.nih.gov/pubmed/22177190 [ Links ]
Received: August 16, 2017; Accepted: November 09, 2017











 texto en
texto en 



