Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Enfermería Global
versión On-line ISSN 1695-6141
Enferm. glob. vol.19 no.57 Murcia ene. 2020 Epub 16-Mar-2020
https://dx.doi.org/eglobal.19.1.366661
Originals
Guillain Barré syndrome: epidemiological clinical profile and nursing care
1Nurse. Resident of the State University of Western Paraná. Brazil.denisehoffmannrigo@yahoo.com.br
2Nursing Professor at the State University of Western Paraná. Brazil.
3Physician of the Epidemiological Surveillance Division of Cascavel City Hall. Brazil.
Objective
To know the socio-demographic, clinical epidemiological and care characteristics of patients hospitalized with GBS in a school hospital in the West of Paraná.
Methodology
This is a quantitative, retrospective study about the socio-demographic characterization, clinical epidemiology and care of hospitalized patients with GBS in a school hospital from 2013 to 2017. Totaling 23 patients whose electronic records were analyzed. All statistical analyzes were performed in the XLStat program (2010).
Results
The majority of the patients presented ages ranging from 51 to 60 years (31.12%), followed by ages 41 to 50 (13.04%) and under 15 (13.04%), male (60.87) , with most presenting previous infectious symptoms such as myalgia, headache, fever, diarrhea. The symptoms related to GBS presented in the period from four to nine days before admission included the ascending, symmetrical form with a decrease in muscle strength. During the hospitalization they underwent procedures such as bladder catheterization and peripheral venous puncture. Among the laboratory exams, the blood test and diagnosis of electro-urography were highlighted. The main treatment was immunoglobulin. Most of the patients presented high dependence for nursing care according to Fugulin's patient classification system.
Conclusion
The development of studies that allow the knowledge of the characterization of a specific group of patients affected by a disease considered rare, constitute instruments for health planning.
Key words: Guillain-Barré syndrome; Epidemiology; Hospitals of Teaching
INTRODUCTION
Guillain-Barre Syndrome (GBS) is considered an acute inflammatory polyneuropathy with the highest occurrence today, usually presenting as a symmetrical flaccid symmetric ascending and areflexia. 1
Regarding the incidence this can vary according to geographic region and sex. In Western countries the incidence varies from 0.89 to 1.89 per 100,000 people (mean of 1.11) and in children from 0.5 to 1.5 per 100,000 people, with a slight predominance in males. There is a 20% increase in the chance of acquiring the disease every ten years after the first decade of life. Most cases are preceded by upper respiratory tract infections or diarrhea caused by viral conditions. The main etiological agents are Campylobacter jejuni (up to 30% of cases) and cytomegalovirus (in up to 10% of cases). In the clinical diagnosis, neurological examination points to symmetrical weakness of the lower limbs with absent or decreased osteotendinous reflexes and pain. The main complementary tests are electroencephalography (EMG) and cerebrospinal fluid analysis. In the first, there are specific alterations for each clinical form of the disease and in the liquor of the albino-cytological dissociation.2
In Cascavel / PR there was an increase in cases of GBS in the years 2007 and 2008, with records of 2.1 and 4.5 cases per 100,000 inhabitants from August / 2006 to July / 2007 and from August / 2007 to July / 2008, respectively, exceeding the recommended incidence of one case / 100,000 inhabitants. Given the context of the disease in the State of Paraná, the State Department of Health of Paraná, from 2016 determined the mandatory notification of the disease and implemented the state protocol for surveillance of GBS and other serious acute neurological diseases post-infectious in the State. 3
GBS is a pathology considered to be rare, and its annual incidence is generally low, but it is a disease occurring worldwide and independent of factors such as age, sex, social class and life habits. It is a rapidly evolving disease whose recovery and healing can occur within weeks to months, with complications and evolution to a potentially fatal form, requiring rapid diagnosis. In spite of the severity, GBS presents a good prognosis, with approximately 95% of the cases recovering completely and only 2 to 5% evolving to death, but there is no prospect of recovery after two years of evolution of the pathology.4)(5)
At this juncture, the present study aimed to know the socio demographic, clinical epidemiological and care characteristics of patients hospitalized with GBS at a school hospital in the West of Paraná from 2013 to 2017.
METHODOLOGY
This is a quantitative, retrospective, descriptive research that presents a socio-demographic, clinical epidemiological and assistance characterization of patients hospitalized with GBS in a school hospital in the West of Paraná from electronic medical records. Currently, this hospital has 210 active beds, being a reference in the Western region for the care of traumatology and neurology covering 25 municipalities that make up the 10th Regional Health Department of the State of Paraná - PR (SESA-PR). 6
The search for patients with the diagnosis of GBS was first performed by the International Statistical Classification of Diseases (ICD 10 - G61.0 GBS) 7 in the electronic medical record system Tasy Philips (hospital health management system) and later confirmed by the immunoglobulin release list of the hospital's central pharmacy for the period from January 2013 to December 2017. The data obtained in the first search were crossed with the latter in order to guarantee that there would be no loss of patients / medical records. The study population initially counted 28 patients with the diagnosis of GBS.
The inclusion criterion for the study included all the patients who had a medical diagnosis for GBS hospitalized at a school hospital in the west of Paraná for the study period. Exclusion criteria were all patients whose medical records did not show evolution of the neurologist and / or who did not present registered data regarding the proposed characterization. In this way, 23 patients were diagnosed with GBS, whose records were analyzed.
The data collection was done from the records in the patient's electronic records, seeking out socio-demographic information, clinical epidemiology, and care related to hospital admissions. The data collection instrument was constructed based on the surveillance protocol of the GBS of the State of Paraná 3 and included socio-demographic data: sex, age, schooling, marital status, profession, municipality of residence; epidemiological clinical data: symptoms prior to hospitalization, signs and symptoms at admission and discharge, laboratory and imaging tests performed; medicines used; procedures performed; data based on Fugulin's classification. 8
The collected data was arranged in Excel spreadsheets for constitution of the database and subsequent descriptive analysis of the results found for the socio-demographic characterization, clinical epidemiology, exams and medications used.
The drugs were grouped according to classification system Anatomical Therapeutic Chemical (ATC) 9) for the second level, which indicates the main therapeutic group.
The care data was analyzed according to Fugulin's patient classification system (PCS) 8, performed by nurses during hospitalization and recorded in an electronic medical record, considering the first and last classification. This classification allows assessing the care complexity and the evolution of hospitalized patients. To do this, we use an instrument composed of twelve areas of care: mental state, oxygenation, vital signs, motility, ambulation, feeding, body care, elimination, tissue integrity, therapeutic, dressing, time spent in the dressing. Each area of the care evaluated receives a score of one to four points and the sum of these points ranges from 12 to 48, indicating an increasing complexity of the patient's care, corresponding to: minimal care (12 to 17 points), intermediate care (18 to 22 points); high dependence (23 to 28 points); semi-intensive care (29-34 points) and intensive care (35-48 points).
After that, the Chi-square test of Independence was applied to the sociodemographic, clinical epidemiological, care, examination, and medication variables, associating them with the patient's gender, in order to verify the association between them. For the clinical classifications of the disease at different times (onset of symptoms / admission and discharge period, and for the first and last classification of Fugulin) the McNemar Chi-square test was also applied to evaluate whether the periods of admission and discharge were statistically different.
All statistical analyzes were performed in the XLStat (2010) program 10, assuming a significance level of 5%, where p <0.05 indicates that the categories are statistically different, that is, "p significant", and p> 0 , 05 indicates that the categories are not statistically different, are equal, ie "non-significant p".
The research was developed respecting all the ethical precepts according to Resolution 466/12 of the National Health Council (NHC), with the favorable opinion of the Research and Ethics Committee (REC) of Unioeste under No. 2,748,437.
RESULTS
In the descriptive analysis of the results, it was observed that within the studied period we had an ascending distribution of cases in the years of 2013 with 17.5%, 2014 with 21.5%, 2016 and 2017 with 26% respectively, with exception of the year 2015 with 8.69%. The majority of cases presented ages ranging from 51 to 60 years (31.12%), followed by ages 41 to 50 years (13.04%) and children under 15 years (13.04%). Of the total, 60.87% were males and 39.13% females, with the majority being married (65.22%) and Catholic (65.22%). As for schooling, 39.13% did not present such data on enrollment, 26.09% had complete Elementary School and 13.04% incomplete Elementary School. The municipality of residence in the city of Cascavel-PR was the most frequent (56.52%) followed by Campina da Lagoa and Santa Tereza do Oeste with 8.70%. Regarding the profession of the patients, 60.87% did not present this data in registry, 13.04% were farmers and 8.70% of the household. Finally, 100% of the patients had hospital discharge.
Regarding the general symptoms prior to hospitalization, the majority of patients presented myalgia (73.91%), headache (56.52%), fever (39.13%), and dysphagia (17.39%) respectively.
The duration of the onset of symptoms, until admission/hospital admission of the patient lasted from four to six days (34.78%), followed by seven to nine days (21.74%) and one to three days (17.39%). In 86.96% of the cases, the presence of motor deficiency was verified, mainly in ascending and symmetrical form (69.57%). The muscle strength decreased in 95.65%, of which 47.83% were in lower limbs (LL) and 43.48% in lower limbs and upper limbs (UL). About 34.78% of the patients had decreased muscle tone, 26.09% had cervical musculature impairment, 21.74% had respiratory muscles, and 17.39% had face musculature. Only 8.70% of the patients remained hospitalized in the Intensive Care Unit (ICU) (Table 1). Regarding the hospitalization time, an average of 34 days was obtained, varying between the longer time of 81 days and the shorter time of five days of hospital stay.
Table 1. Absolute (AF) and relative (RF) frequencies of symptom onset until admission of GBS patients * (NA: not applicable; lower limbs (LL); upper limbs (UL).
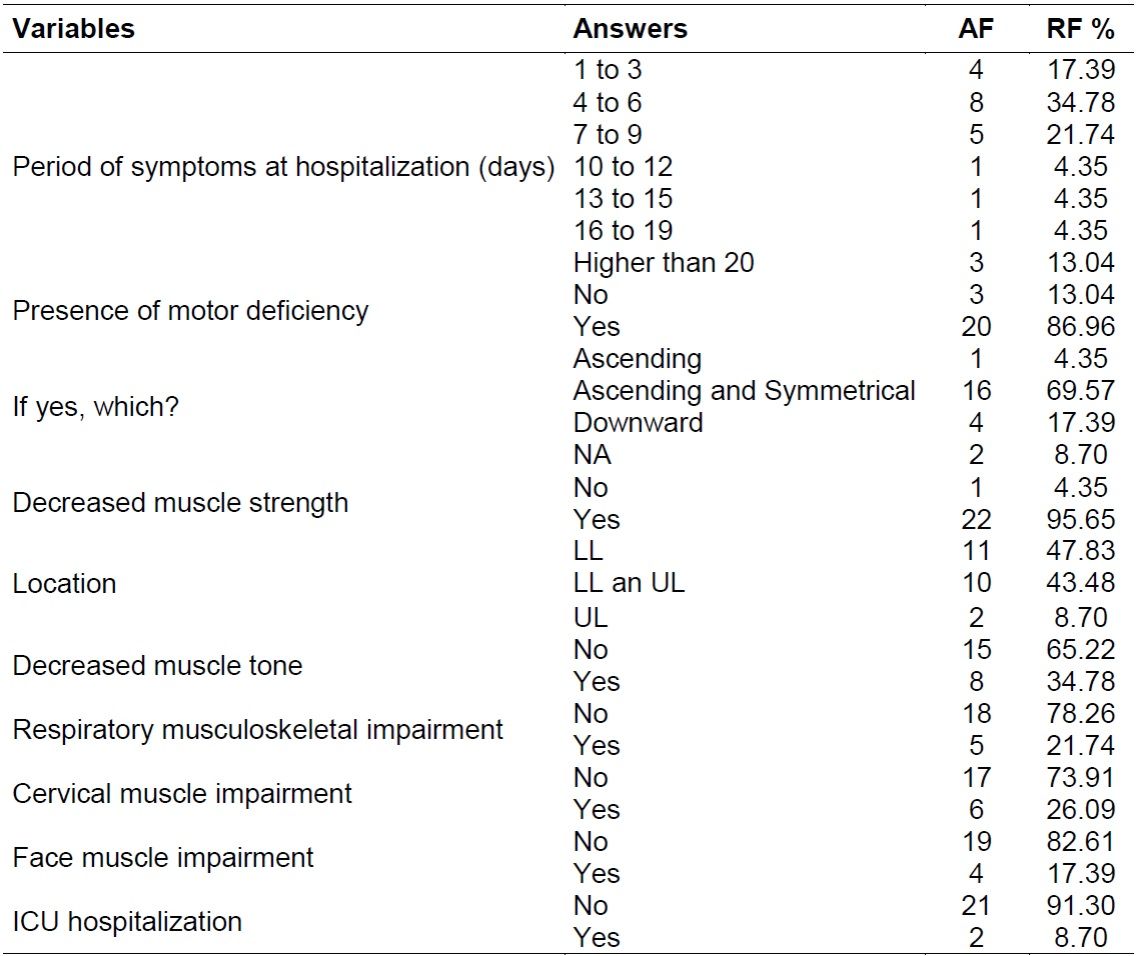
*GBS: Guillain-Barré syndrome.
Source: Data research, 2018.
Regarding the hospital discharge period, 65.22% of GBS patients still had motor deficiency, the majority being upward and symmetrical (47.83%). The same was observed for the reduction of muscle strength (73.91%), especially in LL (47.83%). Only 8.70% of the patients had a decrease in muscle tone, and only 4.35% in the musculature of the face. None of these showed impairment of the respiratory and cervical musculature (Table 2).
Table 2. Absolute (AF) and relative (RF) rates in the hospital discharge period of GBS patients (NA: not applicable; LL; UL).
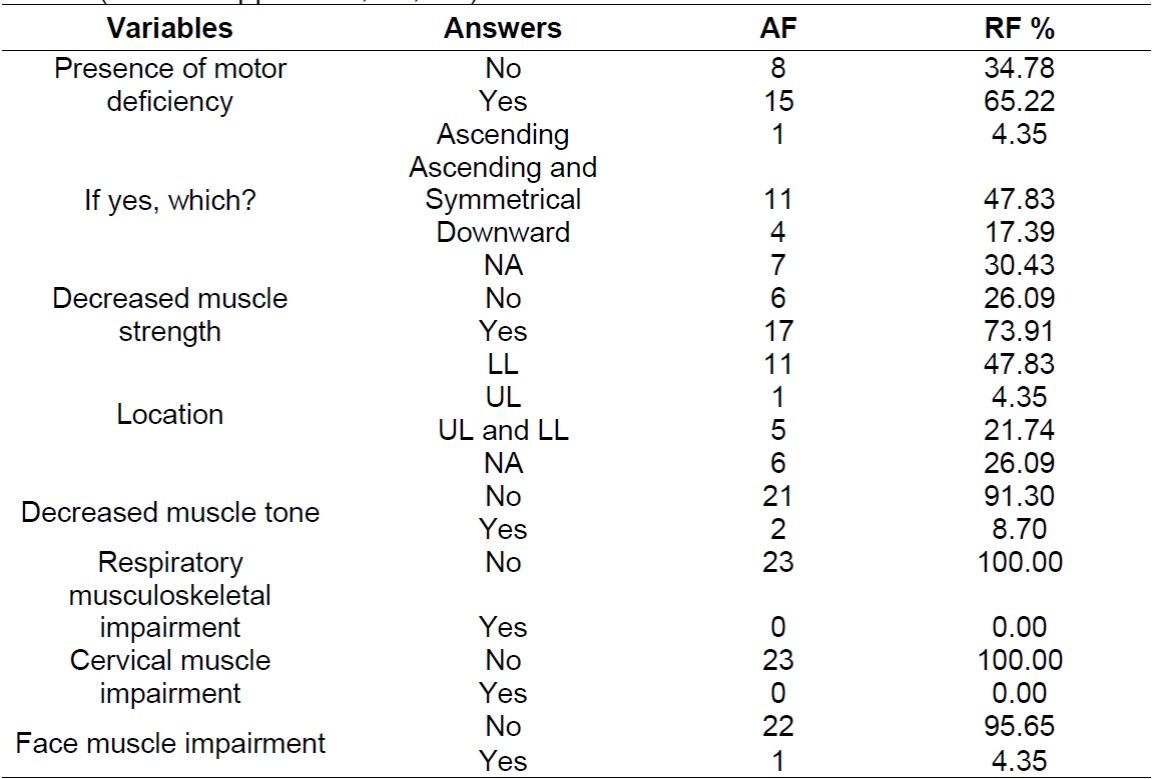
*GBS: Guillain-Barré syndrome.
Source: Data research, 2018.
Of the patients with GBS, the minority had comorbidities such as: hypertension (26.09%), cancer (13.04%) and diabetes mellitus (4.35%).
During the hospitalization period, the most frequently performed procedures were bladder catheterization (69.57%) and peripheral venous catheter puncture (100%), and the other procedures (oral-tracheal intubation, nasogastric probing, drainage and central venous catheter puncture) performed in less than 13% of cases.
When analyzing the association of the previous symptoms of the variables related to hospitalization, the onset of symptoms until the period of hospitalization, symptoms presented by patients at the time of hospital discharge, different comorbidities and procedures performed during hospitalization and their associations with the different sexes there was no statistically significant association (p> 0.05).
Regarding the laboratory tests, it was observed that all the patients had a blood test; 95.65% glucose, potassium, sodium, partially activated thromboplastin time (KPTT) and C-reactive protein (CRP); 91,30% glutamic-pyruvic transaminase (GPT), glutamic-oxalacetic transaminase (GOT), prothrombin time (PT) and urea; 82.61% of total bilirubin and fractions, chlorine, creatinine and liquor routine; 65.22% Hemosiderosis Velocity Rate (HVR) and Venereal Disease Research Laboratory (VDRL) in CSF; 60.87% pro-calcitonin; 56.52% lactic acid and gasometry; and 52.17% magnesium. Other tests were performed less frequently (less than 50%).
As to imaging and diagnostic exams, the only one performed in the majority of patients was electromyography (90.48%), followed by cranial tomography (45.45%) and chest X-ray (31.82%).
When analyzing the class of medicines used and the amount consumed, it was verified that: 91,30% of the patients used a medicine of class "J06" (immunoglobulins); 78.26% a drug of class "A03" (Antispasmodic, anticholinergic and propellant agents); 73.91% a drug of class "B01" (Antithrombotic agents); 60.87% a medicine of class "NO2" (analgesics); 52.17% a medicine of class "M01" (anti-inflammatory); 52.17% two drugs of class "A02" (Antacids and proton pump inhibitors); 47.83% a "C02" (Antihypertensive) and "C03" class (diuretics); 39.13% between one and two medicines of class "B05" (Blood substitutes and solutions for infusion).
In order to evaluate the care complexity of patients with GBS, data were collected from Fugulin's patient classification system (PCS), with 21 patients presenting this classification available in electronic medical records.
When the analysis of the patient's first and last Fugulin classification was performed, no statistical difference was observed (p> 0.05), making the two periods statistically equal.
Comparing the patients who maintained, improved or worsened their classification in the first and last evaluation, it was verified that in the classification of Fugulin only 20% of the patients presented improvement of the picture and 80% maintained the classification of high dependence. Among the areas of care evaluated to classify the patient, there was a 10% significant improvement for tissue integrity, and for the other areas less than 5% improvement. Oxygenation was the area that most demonstrated significant worsening (20%) (Table 3).
Table 3. Relative frequencies (%) and percentage of maintenance, improvement and worsening of the areas evaluated in the Fugulin classification, for the first and last classification of patients with GBS. p: value of the McNemar Test.
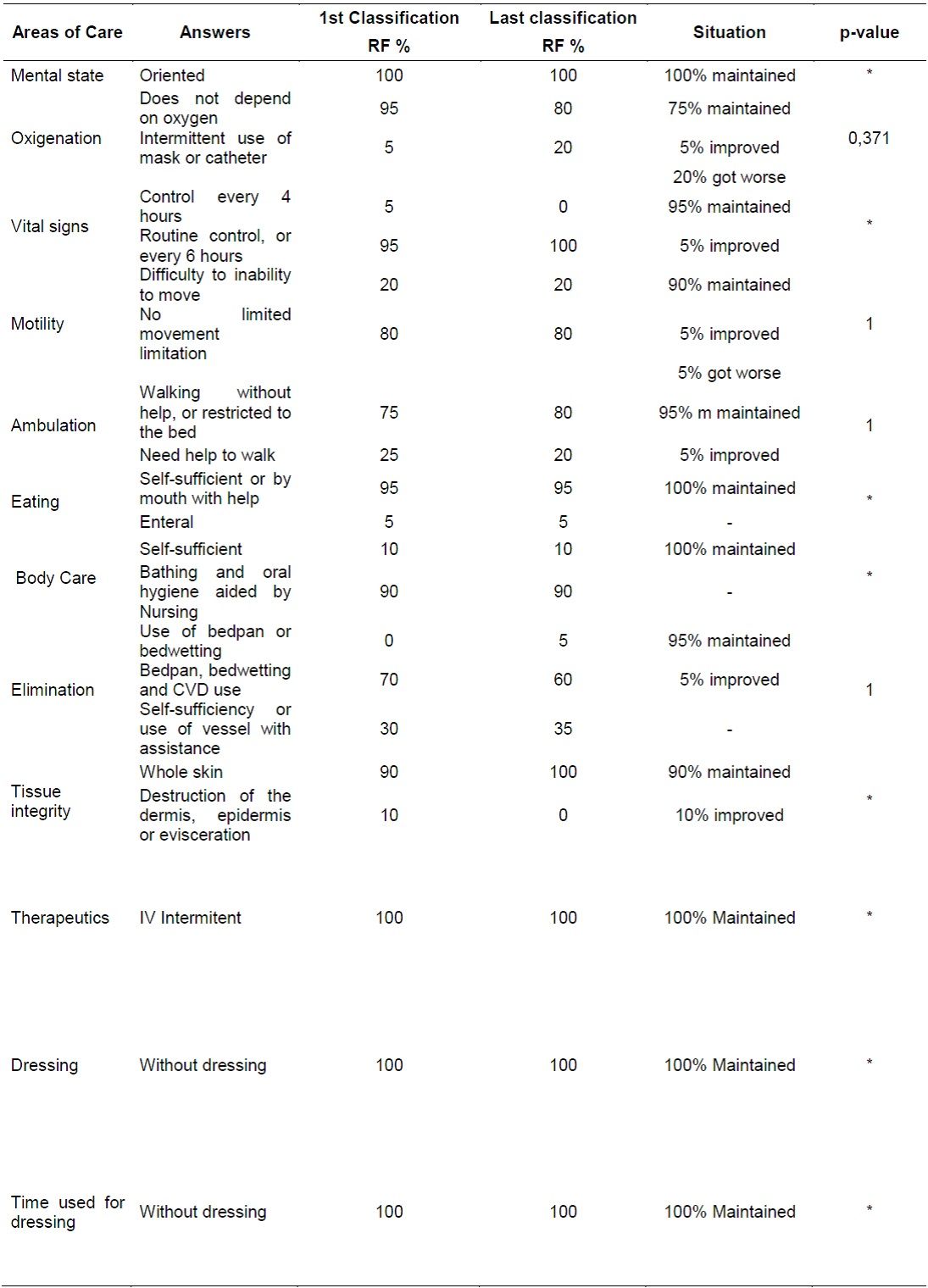
Source: Data research, 2018.
(*):p-value could not be calculated due to the presence of lines with only zero or equal values between different times.
DISCUSSION
This study aims to characterize patients hospitalized in a school hospital affected by GBS. It is noteworthy that in a review of the literature on the subject, there was a low national scientific production, which made it difficult to discuss the results. To do this, available references that were closer to the studied reality were sought.
The findings of this study presented a sociodemographic characterization of 23 patients, who showed a predominance of males (n: 14; 60.87%) followed by females (n: 9; 39.13%), ranging from 51 to 60 years (n = 9, 31,12%), followed by 41 to 50 years (n: 3; 13,04%) and under 15 years (n: 3; 13,04%).
A study conducted in Germany with a total of 73 GBS patients showed a predominance of 42 men versus 31 women, ranging from 22 to 80 years.11
In a study carried out in the same school hospital of this research in the period from 2009 to 2012, there was variation in the age distribution, of which a total of 8 patients, 3 (37.5%) presented ages between 20 and 30 years, 2 (25 %) between 50 and 60 years of age, 1 (12.5%) younger than 20 years, 1 (12.5%) younger than 5 years old, and 1 (12.5%) between 40 and 49 years old. Regarding the sex, they identified that the patients investigated in the period did not present difference for the gender variable, being 50% for the male and female, respectively.12)
Over the years there has been a change in the socio-demographic profile of GBS patients hospitalized in the study institution, pointing to an increase in the number of GBS cases in men and adults over 41 years.
Results showed that the majority of the patients presented: myalgia (73.91%), headache (56.52%), fever (39.13%), diarrhea and dysphagia, respectively (17.39 %). At this time, the duration of symptoms until admission / hospitalization was four to six days (34.78%), followed by seven to nine days (21.74%). Recent studies show that symptoms of GBS manifest between one and four weeks after viral or bacterial infection.13
It is noteworthy that microorganisms frequently correlated with GBS are Campylobacter jejuni,Mycoplasma pneumoniae,Haemophilus influenzae, cytomegalovirus, Epstein-Barr virus and influenza picture, whose clinical manifestations include symptoms such as myalgia, headache, fever and diarrhea.14
When analyzing the results related to the clinic of the patients, the presence of motor deficiency was observed in 86.96% of the cases, mainly in ascending and symmetrical form (69.57%), with decreased muscle strength (95.65%), (47.83%) and in LL and UL (43.48%), and in most of the patients there was no decrease in muscle tone, involvement of the respiratory, cervical and face musculature. This study corroborates the findings that the predominant symptoms in the acute phase of the disease are: muscle weakness, paralysis, lack of sensation, numbness, pain and decreased reflexes that normally reach the feet, legs, trunk, arms and hands.13)
The classic clinical pattern of GBS is ascending paralysis that evolves over hours to days with tingling, weakness, decreased tenderness in the extremities, and lower limbs are more affected than the upper limbs. In disagreement with the findings in the present study, the literature indicates that facial diparesis occurs in 50% of the affected individuals. In general, the prognosis of the disease is good, with an estimated 90% of patients having complete functional recovery or remaining with minimal deficits up to one year after the onset of GBS.14
Among the most performed procedures in the patient are the bladder catheter of delay (69.57%) and peripheral venous catheter puncture (100%), and other procedures such as: oral-tracheal intubation, nasogastric probing, chest drainage and central venous catheter were performed in less than 13% of cases. These procedures are due to the clinical picture and the long period of recovery of the GBS patient, as well as the complications that the disease can cause, among them: urinary retention, tachycardia, hypertension, communication difficulties, nutritional deficiency, immobility, venous thrombosis, lung fluids, respiratory failure.13
Regarding the laboratory tests, it was observed that the main tests performed in the patients were blood test, glucose, potassium, sodium, partially activated thromboplastin time (KPTT), C-reactive protein (CRP), glutamic-pyruvic transaminase (GPT), glutamic-oxalacetic transaminase (GOT), prothrombin time (PT), urea, total bilirubin and fractions, chlorine, creatinine and cerebrospinal fluid, Hemosiderimentation Rate (HR), Venereal Disease Research Laboratory (VDRL) in liquor, pro-calcitonin. The laboratory tests help in the diagnosis, treatment and proper management of the disease and the patients.
Laboratory interpretation in the routine of care is extremely important in order to assist in the detection of alterations of the organism to the pathology. Therefore, the exams identified in this study, such as creatinine and urea, are indicated for the evaluation of renal function; potassium and sodium to detect hydro-electrolytic changes; CRP as a marker of infection / inflammation; PT and KPTT for evaluation of hemostasis; GOT and GPT for evaluation of liver function; and glucose for glucose changes. The hemogram, an examination requested for all patients in the study, allows the evaluation of the patient in a systemic way.15 Already the liquor test to verify the protein-cell dissociation present in the GBS.16
The diagnosis and follow-up of GBS are based on a set of clinical, laboratory and imaging and diagnostic exams. It was verified that the only examination performed in the majority of patients was electromyography (90.48%), followed by cranial tomography (45.45%) and chest X-ray (31.82%). The electromyography examination may show demyelinating or axonal forms present in the GBS.16 Computed tomography of the skull, due to the use of contrast enhances the ability of differentiation between tissues, facilitating the visualization of lesions when compared to previously unrecognized images, and with that monitor the evolution of the patient and intervene with greater effectiveness. On the other hand, the monitoring of the pulmonary condition of the GBS patient can be performed by means of the chest X-ray, allowing the detection of early changes such as pneumonias resulting from respiratory paralysis and bed restriction.17
In the analysis of the drugs it was verified that the class of immunoglobulins (91.30%) was the most used in the patients. In Brazil, including in other countries, immunoglobulin is the first-choice treatment for GBS because it is considered safer, easier to administer, efficient, with fewer adverse events, more affordable, and the only drug available in the National List of Essential Medicines (RENAME) to patients through the Unified Health System (UHS).13 Another therapeutic option not commonly used in Brazil is plasmapheresis, due to the fact that it presents adverse events such as hypotension, thrombophilia and others.5) Both treatments present similar efficacy, promoting a faster recovery of the patient, when compared to the conservative treatment (not using any of the two), mainly in the acceleration of the motor recovery. It is emphasized that the combination of the two therapeutic modalities is not indicated, since this does not impart additional improvement to the patient.18
The other drugs used were of the class of antispasmodic, anticholinergic and propellant agents and antithrombotic, analgesic and anti-inflammatory agents. Pain in GBS is neuropathic of nociceptive origin resulting from a dysfunction of the nerve impulse transmission pathways of pain, in which the painful stimulus occurs in a chronic way. This category justifies the use of analgesics and anti-inflammatories, but this class of drugs when in continuous use, affects the gastrointestinal system, which triggers the use of agents of the class of antispasmodic, anticholinergic and propulsive. The fact that patients commonly present with paralysis mainly of lower limbs, justifies the use of antithrombotic drugs, since they remain bedridden.19
This study also gave rise to results that imply in several aspects regarding the process of assistance to the GBS patient, who needs to be assisted by a multi-professional team, but especially by the nursing team, as it remains at the bedside daily, having as its core work the provision of direct and indirect care to the patient.
For this, it is essential the planning of actions and management of care, recording of the executed planning and, finally, evaluation of the process, allowing to generate knowledge from the practice, and mainly to offer integral assistance and to the patient with GBS. From this point of view, it is extremely relevant to use the available instruments to consolidate care planning, knowing the degree of complexity of care that a particular clientele needs.20
When the comparison between the first and last classification of Fugulin was performed, considering that patients who maintained, improved or worsened in this classification, it was verified that only 20% showed improvement and 80% maintained the classification of high dependence. This expresses that the patient needs assistance in several areas of care performed by the nursing team as: bed movement, body hygiene, skin care, among others, both during hospitalization and after discharge at home.
Among the areas of care analyzed in the first and last classification of the patients, 10% improvement in tissue integrity was achieved, and for the others less than 5% improvement. Oxygenation was the area that showed the most worsening (20%). This finding is due to the fact that the recovery of GBS patients is generally slow and progressive and may extend for days, months and even years.
Although the results showed all the time and space oriented, non-oxygen dependent patients with sTable vital signs at regular routine intervals, these had important limitations such as: no limited movement limitation, bed restriction, dependence on the nursing team for bathing and oral hygiene, use of midwife, bedwetting and use of late bladder catheter. This requires greater attention on the part of the nursing team, considering that they needed to be submitted to various procedures such as medication administration, airway aspiration, bladder catheterization, change of position, hygiene and comfort, among other care. All this requires adequate planning and design of the team to meet the care needs of these patients since the complexity of care is higher.21
CONCLUSION
The development of studies that provide the knowledge of the characterization of a specific group of patients affected by a disease considered rare, in which its exact etiology is still unknown, becomes extremely relevant since they constitute instruments for the planning in as well as subsidizing health professionals in order to provide quality care to this clientele.
The study made it possible to verify that the majority of the cases were concentrated in men over 40 years of age, with signs and symptoms prior to hospitalization such as myalgia, headache, fever, diarrhea and dysphagia related to previous infection. The classic signs of GBS as ascending, symmetrical and decreased muscle strength appeared from four to nine days before admission until hospital discharge.
Still, according to Fugulin's classification, most of these patients presented highly dependent care complexity. The characterization obtained in the study allows inferring the need for assistance by a multi-professional team, as well as the nursing team for integral care. In addition, knowing the socio demographic characteristics, epidemiological clinics and care of patients with GBS allows a more adequate planning of nursing care.
It is worth noting the difficulty in obtaining scientific studies on GBS and nursing care, in view of the low production on this subject, which made it difficult to discuss the results obtained in the present study. Thus, it is necessary to expand research on the subject, as well as wide dissemination and application of the state protocol, in order to optimize the diagnosis early, seeking rapid onset of therapy and decrease of sequelae in the patients affected by the disease.
REFERENCIAS
1. Matos, AMB. Perfil clínico, epidemiológico, laboratorial e letroneuromiográfico de pacientes com síndrome de guillain barré assistidos no hospital geral de fortaleza. Hospital geral de Fortaleza, Fortaleza 2017. [ Links ]
2. Maranho LS; Ribas GW; Bandeira M. Síndrome de guillain-barré em paciente pediátrico: relato de caso e revisão da literatura. Rev Med UFPR 3(1): 41-44. 2016. [ Links ]
3. Paraná. Protocolo de vigilância da síndrome de guillain-barré e outras doenças neurológicas agudas graves pós-infecciosas. Secretaria De Estado da Saúde Superintendência de Vigilância em Saúde, versão 4.0, 2016. [ Links ]
4. Beneti, GM; Silva DLD. Síndrome de Guillain-Barré. Semina: Ciências Biológicas e Saúde, Londrina, 27(1): 57-69, jan/jun. 2006. [ Links ]
5. Brasil. Portaria SAS/MS nº 1171. Protocolo Clínico e Diretrizes Terapêuticas Síndrome de Guillain-Barré, 2015. [ Links ]
6. Cadastro Nacional de Estabelecimentos de Saúde - CNEAS. Disponível em: http://cnes2.datasus.gov.br/cabecalho_reduzido.asp?VCod_Unidade=4104802738368. Acesso em: 08 jan 2019. [ Links ]
7. Organização Mundial da Saúde. Classificação Estatística Internacional de Doenças e Problemas Relacionados à Saúde - CID-10. 10a rev. São Paulo: Universidade de São Paulo; 2008. [ Links ]
8. Conselho Federal de Enfermagem (BR). Resolução COFEN Nº 543/2017, de 18 de abril de 2017. Atualiza e estabelece parâmetros para o Dimensionamento do Quadro de Profissionais de Enfermagem nos serviços/locais em que são realizadas atividades de enfermagem. Brasília (DF): COFEN; 2017. [cited 2019 jan 30]. Available from: http:// www.cofen.gov.br/resolucao-cofen-5432017_51440.html [ Links ]
9. WHO Collaborating Centre for Drug Statistics Methodology, Guidelines for ATC classification and DDD assignment 2016. Oslo, 2016. [ Links ]
10. Addinsoft. Software XLSTAT Versão Anual 2017.19.02. Licença ID 43894 (Node-lock). [ Links ]
11. Derksen A, Ritter C, Athar P, Kieseier BC, Mancias P, Hartung HP, Sheikh KA, Lehmann HCL. Sural sparing pattern discriminates Guillain-Barré syndrome from its mimics. Muscle & Nerve Volume [internet] 2014, [cited 2019 Jan 25] 50:780-784. Available from: https://onlinelibrary.wiley.com/doi/full/10.1002/mus.24226 [ Links ]
12. Moraes A , Casarolli ACG, Eberhardt TD, Hofstatter LM. Caracterização dos pacientes com síndrome de guillain-barré internados em um Hospital Universitário. Revista Enfermagem Contemporânea. [internet] 2015, [cited 2019 Jan 25] Jan./Jun.;4(1):7-11 Available from: https://www5.bahiana.edu.br/index.php/enfermagem/article/view/532 [ Links ]
13. Costa ACD. Síndrome de Guillain-Barré: uma revisão integrativa de literatura e de dados do Sistema Único de Saúde. Universidade de Brasília Faculdade de Ciências de Saúde Departamento de Saúde Coletiva. Brasília, DF 2016 [ Links ]
14. Sudulagunta SR, Sodalagunta MB, Sepehrar M, Khorram H, Raja SKB, Kothandapani S, Noroozpour Z, Sham MA, Prasad N, Ensolarado SP, Mohammed MD, Gangadharappa R, Sudarshan RN. Síndrome de Guillain-Barre: Perfil clínico e controle. Ger Med Sci [Internet]. 2015; [cited 2019 Jan 25] 13(16). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4576316/ [ Links ]
15. Costa DAG. Interpretação de exames. 2. Ed. São Paulo: Medcel, 2014. [ Links ]
16. Santos SLF, Alves HHS, Prado RMS, Barros KBNT. Parâmetros terapêuticos da síndrome de guillainbarré: uma revisão sistemática de estudos de casos. RPBeCS. [internet] 2017, [cited 2019 Jan 25] 4(1):09-17. Available from: https://docplayer.com.br/57331757-Revista-brasileira-de-pesquisa-em-ciencias-da-saude.html [ Links ]
17. Souza ABG, Chaves LD, Silva MCM (org.). Enfermagem em clinica medica e cirúrgica: teoria e prática. São Paulo (SP): Martinari, 2014. [ Links ]
18. Silva RPA. Síndrome de guillain-barré: Revisão retrospetiva da casuística dos casos hospitalizados no Centro Hospitalar do Porto. Instituto de Ciências Biomédicas Abel Salazar da Universidade do Porto. Porto, Jun de 2015. [ Links ]
19. Souza LS, Comarella L. Comparação da eficácia e segurança da gabapentina no tratamento da dor na índrome de guillain-barré. Revista Saúde e Desenvolvimento 5(3), jan/jun 2014. [ Links ]
20. Casarolli ACG, Eberhardt TD, Moraes A, Hostätter LM. Assistência de enfermagem na síndrome de guillain-barré. REVISTA CONTEXTO & SAÚDE IJUÍ EDITORA UNIJUÍ v. 14 n. 27 JUL./DEZ. 2014 p. 16-22. [ Links ]
21. Nobre IEAM, Barros LM, Gomes MLS et al. Sistema de classificação de pacientes de fugulin: perfil assistencial da clínica médica. Rev enferm UFPE, Recife, 11(4):1736-42, abr., 2017. [ Links ]
Received: March 08, 2019; Accepted: June 23, 2019











 texto en
texto en 


