My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Enfermería Global
On-line version ISSN 1695-6141
Enferm. glob. vol.19 n.58 Murcia Apr. 2020 Epub May 18, 2020
https://dx.doi.org/eglobal.362191
Originals
Quality of life of patients who have undergone bariatric surgery: a cross-sectional study
1PhD student at Universidade Federal de Minas Gerais. Brazil.
2Nurse, Universidade Federal de Minas Gerais. Brazil.
3Professor, Universidade Federal de Minas Gerais. Brazil.
4Hospital Santa Rita, Contagem, Minas Gerais, Brazil. nandapenido@hotmail.com
Purpose
Analyze factors that influenced the quality of life (QoL) of patients after bariatric surgery.
Methods
A cross-sectional study was carried out, involving 307 adult bariatric surgery patients between 2012 and 2014. Data was obtained from the electronic patient records and telephone interviews. To assess the QoL, the World Health Organization Quality of Life-Bref (WHOQOL-bref) was used. A simple linear regression model was constructed, adjusted by sociodemographic variables, with p<0.05.
Results
The domains with the worst scores were the physical (mean=58.45; SD±10.42) and environmental (mean=65.19; SD±11.36). The best domains were the social (mean=76.51; SD±15.71) and psychological (mean=68.70; SD±15.71). In the linear regression model, it was observed that time since the surgery was inversely associated with the physical health domain. For each month post-bariatric surgery, the patient's average score dropped by 2.66 points, adjusted by sex and age.
Conclusions
Time since the surgery could be an important determinant of the physical domain score of quality of life. Identifying the quality of life after bariatric surgery and influential factors is fundamental to prepare these patients for the changes deriving from the weight loss.
Keywords: Bariatric Surgery; Epidemiology; Obesity; Quality of Life; Surgery
INTRODUCTION
Obesity is a risk factor for many chronic conditions1. In its report, WHO estimated that 12% of the world population was obese. The region of the Americas showed the highest percentage, with 62% of overweight and 26% of obesity in both sexes2. In Brazil, the prevalence of obese adults corresponded to 18.9% in 20173.
It is known that obesity is a multifactorial problem and its treatment involves several types of approaches, such as clinical treatment and surgical treatment, when indicated4 5.
In Decree 424 from March 19th2013, the Ministry of Health highlights that the following criteria should be observed for the practice of bariatric surgery: individuals who did not respond to clinical treatment; dietary re-education; psychological care; prescription of physical exercise and, if necessary, drug therapy. It is emphasized in the decree that the surgical treatment is but part of the comprehensive treatment of obesity, which should be primarily based on health promotion and clinical care6.
The surgery should be indicated to individuals with: BMI of 50 kg/m2; BMI of 40 Kg/m², with or without comorbidities, and without successful clinical treatment, and individuals with BMI> 35 kg/m2and comorbidities6 7.
In the first bariatric surgeries performed in the world, the analysis of the results was based on data related to weight reduction and possible complications8. Over time, it was observed that, although the patients lost weight and presented few complications in the intra and postoperative phases, they did not consider the result satisfactory. In view of this situation, the need to quantify the postoperative patients' quality of life (QoL) was perceived. In 1982, Linner was the first to adopt patient satisfaction as a subjective criterion to assess bariatric surgery results8.
Therefore, a broader approach to the assessment of bariatric surgery outcomes is fundamental. The bariatric surgery is intended not only to reduce the weight, but also to eliminate or mitigate the diseases associated with obesity and, consequently, to promote the return to social activities9.
In that context, QoL stands out, which is considered to be the subject's perceived position in life. The concept of QoL is subjective and multidimensional, including positive and negative assessment elements in the course of life10.
Although the prevalence of obesity is increasing in Brazil3and, along with this increase, the number of bariatric surgeries has also increased11, in the Brazilian scientific literature, no studies were found in which the QoL of patients who underwent this surgical procedure was evaluated. It is known that the Brazilian scientific production about obesity and QoL in bariatric surgery patients is relatively recent11 12.
Improvement in QoL is also an important factor, but measuring this factor is difficult13.Understanding the QoL of individuals submitted to this surgical procedure favors the multidisciplinary care and treatment process, as it facilitates the planning of actions for the patient, implementing objective interventions and the assessment of their results14 15 16 17.
The purposes in this study were to assess the QoL of individuals submitted to bariatric surgery and to identify the potential factors associated with the QoL of patients submitted to this procedure.
METHODS
Patient and Public Involvement
A cross-sectional study was undertaken, involving 387 adults submitted to bariatric surgery at a general and private hospital in Contagem - Minas Gerais, Brazil, between 2012 and 2014. All measures were taken at one point of time, but at individually different time points in the course of the postoperative treatment.
The final sample consisted of 307 patients. Figure 1displays the flowchart of the sample losses.
Trained professionals collected the data in two phases. As expressed in Figure 1, the first phase involved the completion of a structured questionnaire, elaborated by the researchers, using the electronic medical records of bariatric surgery patients between 2012 and 2014 as a source. In the second phase, the data were collected by telephone interviews (in the first, second and third postoperative year), when another structured questionnaire with validated questions was completed, which contained the World Health Organization Quality of Life-bref(WHOQOL-bref). Patient consent was obtained by telephone.
The WHOQOL-brefis a QoL assessment tool deriving from the short version of the WHOQOL-100. The WHOQOL-brefconsiders the interviewee's experience in the previous two weeks and consists of 26 questions or facets, 24 of which are distributed in four domains: psychological health, physical health, social relationships and environment. In addition, the questionnaire contains two general questions: one refers to the perceived QoL and the other to satisfaction with health10 18.
Each domain includes questions with scores ranging between 1 and 5, 1 indicating the worst assessment and 5 the best. To analyze the answers, the domain scores are assessed separately and transformed into a scale from 0 to 100. The score follows a positive scale. The questions were recoded in accordance with WHO's steps19.
In this study, the sociodemographic (sex, age, self-referred skin color, education, marital situation and mean income per household), clinical (mean pre-surgical weight and BMI) and lifestyle variables were taken into account, as well as variables related to the comorbidities, hospitalization and surgical procedure, present in the questionnaires to collect data from the patient histories and by telephone.
Statistical analysis
The frequencies and proportions were calculated for the categorical variables. For the numerical variables, the mean and standard deviation (SD) were used, due to the symmetry of the variables. To compare the variables and the WHOQOL-brefdomains, the t-test was applied to analyze the two-category variables with normal distribution and ANOVA for variables with three or more categories. For variables with statistical differences on the ANOVA test, the post-hoc test was applied with Bonferroni correction. Finally, to assess the association between the time since the surgery and the WHOQOL-brefdomains, a simple linear regression model was constructed and fully adjusted by all relevant analyses. The authors strongly considered using all fully adjusted relevant analyses in order to study variables that are associated with QOL. Residue analysis and the heteroscedasticity test were used. The results were presented in Tables and Figures. It should be reminded that the total numbers for the variables can vary due to missing data.
All statistical analyses were developed using Stata, version 14.0. Significance was set at 5% (p<0.05) in all analytic procedures.
The researchers funded the project with their own resources.
RESULTS
The research sample mostly consisted of women (87.62%). The mean age of all patients was 37.10 years (SD± 9.32). The majority defined themselves as mulatto (49.84%), finished secondary school (58.96%), lived with a partner (69.06%) and gained a mean income per household of 1 to 3 minimum wages (54.79%) (Table 1).
Table 1. Sociodemographic profile of patients submitted to Bariatric Surgery - Contagem, 2016.
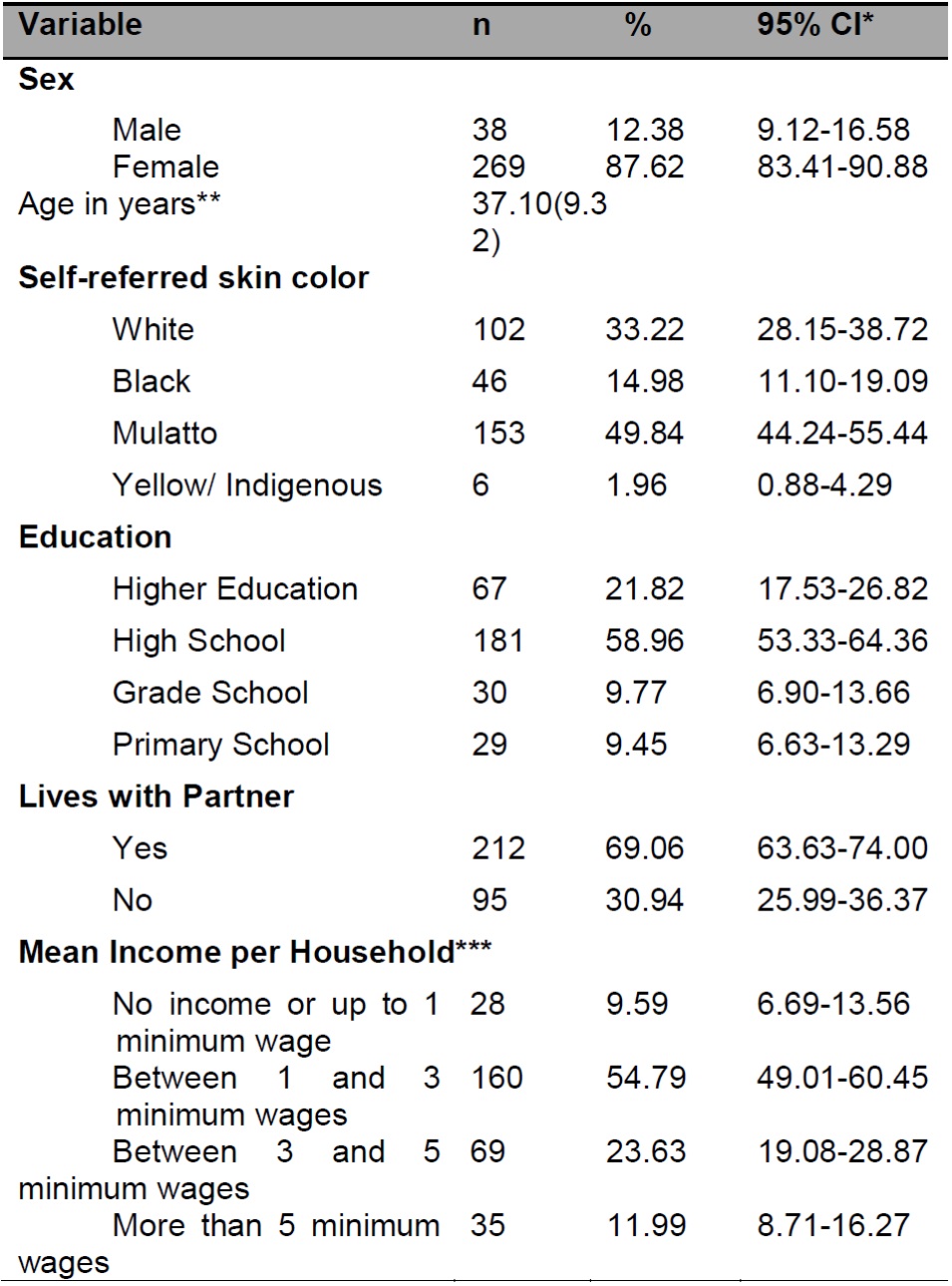
Source: Elaborated for the purpose of this study.
*95% confidence interval.
**Mean and Standard Deviation.
***Mean income per household calculated based on the minimum wage: R$788.00.
What the pre-surgical comorbidities were concerned, most of the sample presents systemic arterial hypertension (42.35%), diabetes mellitus (25.49%), respiratory disease (21.82%) or neurological disease (2.28%). The majority suffered from a gastrointestinal disease though (56.35%).
With regard to the variables related to the surgical intervention, the mean pre-surgical weight was 117.72 Kg (SD = ±20.52) and the mean BMI 43.60 Kg/m2(SD = ±5.59). Most surgeries used laparoscopic (51.47%) and open bariatric surgery (48.53%). Regarding the surgical technique, Roux-en-Y gastric bypass was applied in 94.14% and sleeve in 5.86%.
In the sample studied, on average, 29.92 months (SD = ±10.67) had passed since the surgery, with more than 2 ½ years having passed after the surgery for 159 patients (51.79%). As regards the comorbidities after the procedure, according to self-referred data, the majority did not suffer from systemic arterial hypertension and diabetes mellitus (91.53% and 95.77%, respectively). Among the patients and according to self-referred data, 26.06% classified their health condition as “very bad” before the surgical procedure. After the surgery, 60.59% classified it as “very good” and 30.62% as “good”. In addition, 94.46% demonstrated satisfaction with the surgery, affirming that they would do it again.
The QoL assessment evidenced that the worst scores were found in the physical (mean = 58.45; SD±10.42) and environmental domains (mean = 65.19; SD±11.36). The highest scores were found in the psychological health (mean = 68.70; SD±10.49) and social relationships (mean = 76.51; SD±15.71) domains. The mean general QoL score was 67.24 (SD±9.42). The domain scores and the general QoL score for the WHOQOL-brefhave been summarized in Figure 2.
In Figure 3, the mean domain scores of the WHOQOL-brefare displayed.The physical health domain demonstrates that the interviewees mention good mobility, disposition in the face of pain and little dependence on medical treatment to lead their life. The lowest mean scores were observed for the facets: energy and fatigue (3.77) and satisfaction with sleep and rest (3.84).
In the psychological health domain, the interviewees attributed higher scores to beliefs (mean = 4.44) and satisfaction with self-esteem (mean = 4.28) and with their bodily appearance (mean = 4.00) (Figure 3).
Also in Figure 3, in the social relationships domain, the interviewees indicated getting support from friends (mean= 4.09), satisfaction with personal relationships (mean = 4.09) and satisfaction with sexual life (mean= 3.99).
Finally, in the environmental domain (Figure 3), the main problems are related to lack of financial resources (mean = 2.70), opportunities for leisure activities (mean = 3.39) and how healthy their physical environment is (mean = 3.56).

Figure 3. Mean assessment of facets in four domains of WHOQOL-bref according to interviewees - Contagem, 2016
In Table 2, the lowest mean scores are found in the physical health domain for patients at 30 months or more after the surgical intervention (p=0.02). In the psychological health domain, the lowest mean scores were for individuals without a monthly income and who received up to one minimum wage. In the environment domain, the female gender was associated with lower mean scores (p<0.001) when compared to the male gender. The variables education and mean income were also associated with this domain, with lower mean scores for people who finished secondary education and gained an average income of one to three minimum wages (p<0.001 in both). In the general QoL assessment, the female gender was associated with lower means (p=0.01). It seems that patients without an income or who gained up to one minimum wage per household assessed their general QoL as worse than the other categories (p<0.001).
The association between the mean scores in the psychological health domain and the mean income variable showed a statistically significant difference between patients with an income of one to three minimum wages and patients with a mean income of more than five minimum wages per household (p=0.03). In the environment domain, when considering the education variable, a statistically significant difference was observed when higher education was compared with grade school and higher education with primary school (p=0.03 and p=0.04, respectively). Concerning the comparative analysis of the mean general QoL, the female gender was associated with lower means and, in the analyses of the mean income per household, a significant difference was observed between people without an income or gaining up to one minimum wage and people with an income of more than five minimum wages; and people with a mean income of one to three minimum wages when compared to people with a mean income of more than five minimum wages (p=0.003, in both) (Table 2).
Table 2. Mean domain scores of WHOQOL-brefaccording to exposure variables - Contagem, 2016
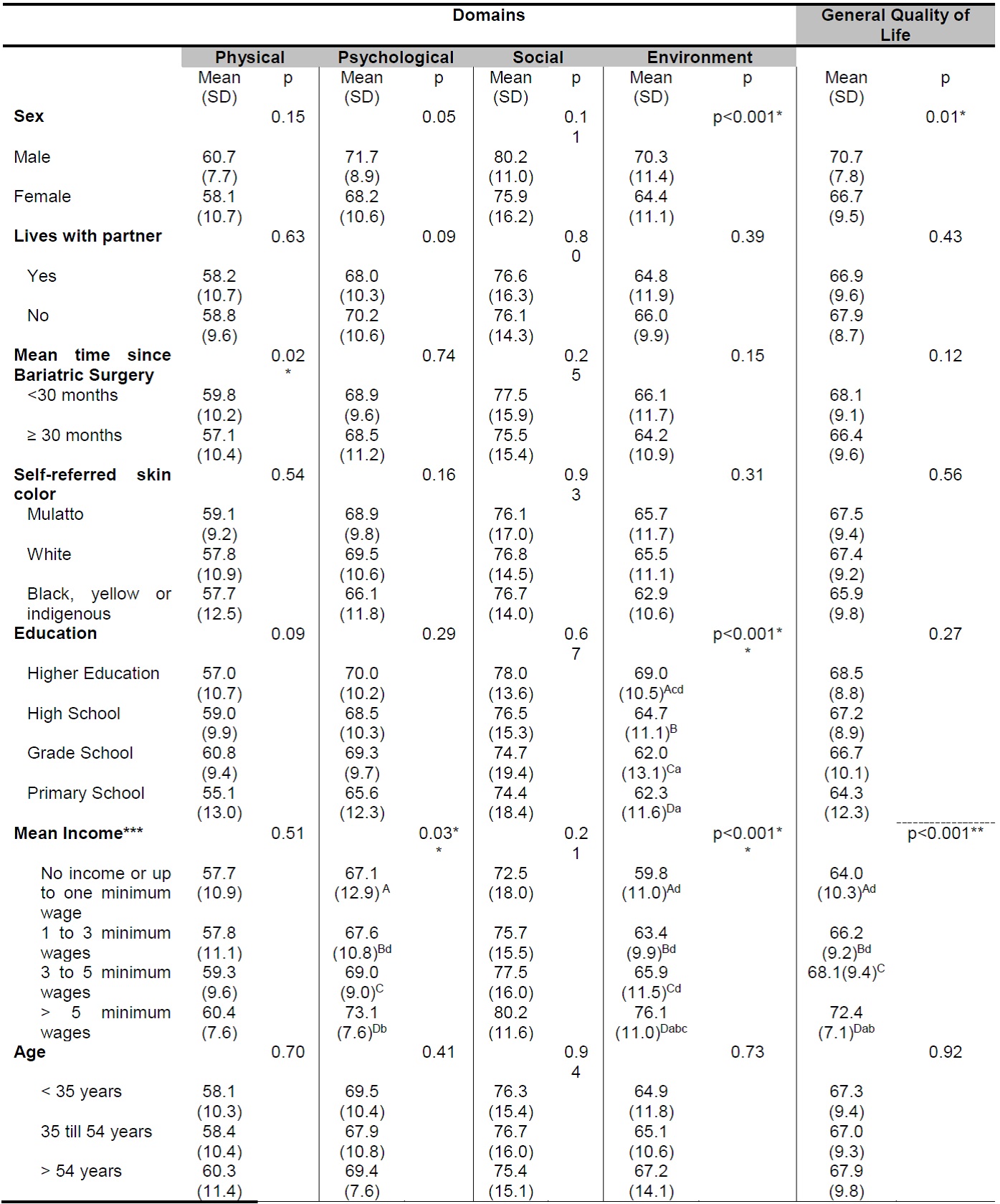
Source: Elaborated for the purpose of this study.
*p-value ≤ 0.05 (t-test).
**p-value ≤ 0.05 (ANOVA and post hoc with Bonferroni correction). A priori, each mean receives a capital letter. The small letters indicate a statistically significant difference between the means.
***Mean income per household calculated based on minimum wage: R$788.00.
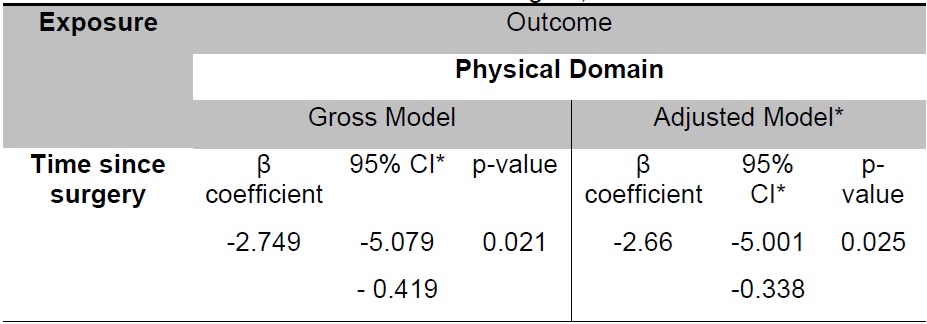
Table 3displays the linear regression model of the relation between the time since the surgery and the physical health domain of the WHOQOL-bref.As observed, the time since the surgery was inversely associated with the physical health domain, that is, for every month post-bariatric surgery, the patient's mean score in this domain dropped by 2.66 points when adjusted by sex and age.
DISCUSSION
In this study, the QoL of individuals submitted to bariatric surgery was assessed. The principal finding of this research was that time since the surgery could be an important determinant of the physical domain score of quality of life.
The profile was similar to that of bariatric surgery candidates in the state of São Paulo, Brazil: married, finished secondary education and part of class C, corresponding to a mean family income of R$ 927.0020.
In addition, studies have demonstrated that the female gender is the population group that most engages in bariatric surgery21 22 23, similar to the results of this study.
The predominance of the female gender can be related to the fact that women are exposed to a higher stress load and tend towards unsuiTable food intake and depression more strongly16 17 21 24. Another factor that makes women turn to surgeries to lose weight is related to prejudice. Due to overweight, the prejudice takes the form of inequalities on the job, in healthcare, educational facilities and institutions, often due to the negative stereotypes that stigmatize people with overweight and obesity25. The other reason refers to the bodily requirements, as the body should comply with the socially imposed beauty and esthetic standards. The sociocultural parameters can influence the perceived bodily image and, therefore, the self-image and the valuation of external appearance26.
As most of the sample lives with some kind of partner, married men and women show higher rates of abdominal obesity26. In addition, a socioeconomic factor is also related to the diet, according to which people in better socioeconomic conditions present healthier diets, due to the consumption of more varied fruits and vegeTables, as well as diet and low-fat products27.
The assessment of the mean domain scores for psychological health associated with the variable mean income per household revealed a statistically significant difference for people with a mean income of more than five minimum wages per household. In the environment domain, concerning the education variable, a statistically significant difference was observed when higher education was compared with grade school and primary school. The fact that, in Brazil, the population with lower income and education (proxy) levels faces difficulties to make change in many of the aspects of these domains can explain this iniquitous result.
As verified, the opportunities for leisure activities are very scarce and the patients studied are hardly satisfied in terms of having enough money to attend to their needs. In addition, there is the fact that, on average, they survive on a family income of 2.36 minimum wages, justifying their dissatisfaction. The obesity is inversely proportional to social class and the poorest population suffers most due to obesity and its diseases28.
In this study, an inverse association was also observed between the time since the surgery and the physical health domain. A downward trend exists in this domain, that is, the more years have passed since the surgery, the lower the patients' assessment in this domain. This drop reflects the natural aging process, entailing new comorbidities or the worsening of comorbidities that used to be under control29.
Finally, it is important to consider some limitations of the study, including the sample loss during the data collection. This may have influenced the lack of statistical significance in some of the results presented. It is highlighted, however, that the registration data of the patients who could not be contacted by telephone were amended to include new data. New calls were made but without success. Sensitivity analyses were developed between the losses and the final sample but, except with regard to color, no significant differences were found between them. In addition, some variables were self-referred, which may have entailed imprecise reports. Despite this potential limitation, this was an economically and logistically feasible option for this study. Also, self-referred weight and height, for example, have been widely used in epidemiological studies as an accepTable and valid method for Brazilian adults30,31. Besides, comorbidities were not included in the analyses. These are unanswered questions and future research can contribute to clarify these limitations.
The last strength of this study is, to our knowledge, that there is a lack of Brazilian studies on the theme with large samples like in this research. This research undoubtedly contributes for clinicians and policymakers to plan interventions that entail a better QoL for bariatric surgery patients, especially in the domains with the worst scores.
In summary, the identification of the QoL after bariatric surgery and the potential influential factors is fundamental in the multiprofessional monitoring of the patients and to prepare these patients for the changes deriving from the weight loss. Thus, care delivery to these patients can continuously improve with a view to a better QoL after the surgical procedure.
REFERENCES
1. World Health Organization. World health statistics 2015. WHO; 2015. [ Links ]
2. World Health Organization. World health statistics: A snapshot of global health. WHO 2012. [ Links ]
3. Brasil. Ministério da Saúde. Secretaria de Vigilância de Fatores de Risco e Proteção para Doenças Crônicas por Inquérito Telefônico. Ministério da Saúde, Secretaria de Vigilância em Saúde, Departamento de Vigilância de Doenças e Agravos não Transmissíveis e Promoção da Saúde. - Brasília: Ministério da Saúde, 2018. [ Links ]
4. World Health Organization. Obesity and overweight. n. 311, Mar. 2011. [ Links ]
5. Coelho EML, Fontela PC, Winkelmann ER, Schwengber MSV. Perda de peso , estado de saúde e qualidade de vida durante 2 anos após cirurgia bariátrica. Ciência & Saúde. 2016;9(3):174-81. DOI:10.15448/1983-652X.2016.3.23377. [ Links ]
6. Brasil, Ministério da Saúde. Redefine as diretrizes para a organização da prevenção e dotratamento do sobrepeso e obesidade como linha de cuidado prioritária da RededeAtenção à Saúde das Pessoas com Doenças Crônicas. Portaria n 424, de 19 demarço de 2013. [ Links ]
7. Conselho Federal de Medicina(CFM). Estabelece normas seguras para o tratamento cirúrgico da obesidade mórbida, definindo indicações, procedimentos aceitos e equipe. Resolução nº 2.131, 12 de novembro de 2015. [ Links ]
8. Nicareta JR, Freitas ACT, Nicareta SM, Nicareta C, Campos ACL, Nassif PAN et al . Bariatric Analysis and Reporting System. ABCD arq bras cir dig. 2015; 28(Suppl 1): 73-78. DOI: http://dx.doi.org/10.1590/S0102-6720201500S100020 [ Links ]
9. Kim J, Eisenberg D, Azagury D, Rogers A, Campos GM. American Society for Metabolic and Bariatric Surgery position statement on long-term survival benefit after metabolic and bariatric surgery. Surg Obes Relat Dis.2016;12(3):453-9. DOI: http://dx.doi.org/10.1016/j.soard.2015.11.021 [ Links ]
10. World Health Organization. WHOQOL: measuring quality of life. The WHOQOL group. WHO: 1997 [ Links ]
11. Santos AA et al. Qualidade de vida de pessoas com obesidade grau III: um desafio Comportamental. Rev Bras Clin Med São Paulo. 2012; 10(5):384-9. [ Links ]
12. Tavares TB, Nunes SM, Santos MO. Obesidade e qualidade de vida: revisão daliteratura. Rev Med Minas Gerais.2010; 20(3):359-66 [ Links ]
13. Kelles SMB, Machado CJ, Barreto SM. Dez anos de cirurgia bariátrica no Brasil: mortalidade intra-hopitalar em pacientes atendidos pelo sistema único de saúde ou por operadora da saúde suplementar. ABCD, arq bras cir dig. 2014; 27(4): 261-267. DOI: http://dx.doi.org/10.1590/S0102-67202014000400008 [ Links ]
14. Mazer, LM, Azagury, DE, Morton, JM. Quality of Life After Bariatric Surgery. Current Obesity Reports. 2017; 2(6): 204-10. [ Links ]
15. Barros LM, Frota, NM, Moreira, RAN, Araújo, TM, Caetano JA. Avaliação dos resultados da cirurgia bariátrica. Rev Gaúcha Enferm.2015; 36(1):21-27. [ Links ]
16. Castanha CR, TCBC-PE AABF, Castanha AR, Belo GQMB, Lacerda RMR, Vilar L. Avaliação da qualidade de vida, perda de peso e comorbidades de pacientes submetidos à cirurgia bariátrica. Rev Col Bras Cir. 2018;45(3): e1864. DOI: http://dx.doi.org/10.1590/0100-6991e-20181864 [ Links ]
17. BarrosLM et al. Qualidade de vida entre obesos mórbidos e pacientes submetidos à cirurgia bariátrica. Revista Eletrônica de Enfermagem; 2015; 17(2):312-21. [ Links ]
18. Fleck MPA et al . Aplicação da versão em português do instrumento abreviado de avaliação da qualidade de vida "WHOQOL-bref". Rev Saúde Pública; 2000;34(2):178-183. [ Links ]
19. World Health Organization. WHOQOL-BREF: introduction, administration, scoring and generic version of the assessment: field trial version, December 1996. 1996. [ Links ]
20. Quesada K. et al. Perfil Socioeconômico e Antropométrico de Candidatas a Cirurgia Bariátrica pelo Sistema Único de Saúde.Saúde e Pesquisa. 2015; 8(3): 431-38. [ Links ]
21. Carvalho TS, Vasconcelos FC, Carvalho MDBM. Análise do histórico de métodos de emagrecimento dos pacientes submetidos à Cirurgia Bariátrica em um hospital público de Belém-PA. RBONE-Revista Brasileira de Obesidade, Nutrição e Emagrecimento. 2016; 10(55):4-11. [ Links ]
22. Klobukoski C, Höfelmann DA. Compulsão alimentar em indivíduos com excesso de peso na Atenção Primária à Saúde: prevalência e fatores associados. Cadsaúde colet. 2017; 25( 4 ): 443-452. DOI: http://dx.doi.org/10.1590/1414-462x201700040094 [ Links ]
23. Lima AR, Brito LS, Tomiya MTO, Souza TKM, Silva RPP, Evolução pondera e qualidade de vida de indivíduos submetidos à cirurgia bariátrica. RBONE-Revista Brasileira de Obesidade, Nutrição e Emagrecimento. 2019; 12(76): 1087-94. [ Links ]
24. Silva CAF, Faro A. Significações relacionadas à cirurgia bariátrica: estudo no pré e pós-operatório. Salud & Sociedad, Antofagasta. 2015; 6(2):156-169. [ Links ]
25. Spahlholz J, Baer N, Honig HH, Riedel-Heller SG, Luck-Sikorski C. Obesity and discrimination - a systematic review and meta-analysis of observational studies. Obes Rev 2016; 17(1):43-5. DOI: 10.1111/obr.12343 [ Links ]
26. Macedo TTS, Portela PP, Palamira CS, Mussi FC. Obese people's perception of their own bodies. Esc Anna Nery. 2015; 19(3):505-510. DOI: http://dx.doi.org/10.5935/1414-8145.20150067 [ Links ]
27. Ares G, Machín L, Girona A, Curutchet MR, Giménez A. Comparison of motives underlying food choice and barriers to healthy eating among low medium income consumers in Uruguay. Cad Saúde Pública. 2017; 33(4): e00213315. DOI:. http://dx.doi.org/10.1590/0102-311x00213315 [ Links ]
28. Matozinhos FP, Meléndez GV, Pessoa MC, Mendes LL, Gomes CS, Costa MA. Distribuição espacial da obesidade em área urbana no Brasil. Ciênc saúde coletiva. 2015;20(9): 2779-2786. DOI: http://dx.doi.org/10.1590/1413-81232015209.00442015 [ Links ]
29. Herpertz S, Muller A, Burgmer R, Crosby RD, Zwaan M, Legenbauer T. Health-related quality of life and psychological functioning 9 years after restrictive surgical treatment for obesity. Surg Obes Relat Dis. 2015; 11(6):1361-70. [ Links ]
30. Carvalho AM, Piovezan LG, Selem SSC, Fisberg RM, Marchioni DML. Validação e calibração de medidas de peso e altura autorreferidas por indivíduos da cidade de São Paulo. Rev bras epidemiol. 2014;17(3): 735-746. DOI: http://dx.doi.org/10.1590/1809-4503201400030013 [ Links ]
31. Ternus DL, Canuto R, Henn RL, Macagnan JAB, Pattussi MP, Olinto MTA. Uso de medidas autorreferidas de peso e altura na determinação do estado nutricional de trabalhadores. Rev Nutr. 2016;29(3):347-356. DOI: http://dx.doi.org/10.1590/1678-98652016000300005 [ Links ]
Acknowledgements
To the Hospital Santa Rita, for support and authorization to collect the data for this study. To Sofie Tortelboom Aversari Martins, for the critical review and proofreading English of the manuscript.
Received: February 07, 2019; Accepted: June 23, 2019











 text in
text in