Meu SciELO
Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Enfermería Global
versão On-line ISSN 1695-6141
Enferm. glob. vol.19 no.59 Murcia Jul. 2020 Epub 10-Ago-2020
https://dx.doi.org/10.6018/eglobal.387451
Originals
Variables associated with adverse events in neonates with peripherally inserted central catheters
1 Enfermera. Alumna de Maestría en Enfermería, Universidad Federal de Rio Grande del Norte /PPGENF/UFRN. Especialista en Cuidados Intensivos Neonatal, Maternidad Escola Januário Cicco. Natal, RN, Brasil. caroline_k16@hotmail.com
2 Enfermeira por la Universidad del Estado de Rio Grande del Norte . Especialista en Centro Quirúrgico por la Facultad Metropolitana de Ciencias y Tecnología. Natal, RN, Brasil.
3a Enfermera. Doctoranda en Enfermería, Universidad del Estado de Rio Grande del Norte /PPGENF/UFRN. Enfermera del Trabajo en el Instituto Federal de Rio Grande del Norte. Natal, RN, Brasil.
3b Enfermera . Doctoranda en Enfermería, Universidad del Estado de Rio Grande del Norte /PPGENF/UFRN. Enfermera del Trabajo en la Maternidad Escola Januário Cicco. Natal, RN, Brasil.
4 Enfermera . Alumna de Maestría en Enfermería, Universidad del Estado de Rio Grande del Norte/PPGENF/UFRN. Enfermera del Trabajo, UNOPAR, Natal, RN, Brasil.
5 Enfermera . Alumna de Maestría en Enfermería, Universidad del Estado de Rio Grande del Norte/PPGENF/UFRN. Natal, RN, Brasil.
6 Profesor Asociado . Universidad del Estado de Rio Grande del Norte, Departamento de Enfermería, Natal, RN, Brasil.
Objective:
To identify the factors associated with the occurrence of adverse events by a peripherally inserted central catheter in newborns.
Methods
A quantitative, cross-sectional study carried out in the Neonatal Intensive Care Unit of a reference maternity hospital in high-risk maternal and child care in Northeast Brazil. The sample of 108 neonates was collected from February to November 2016.
Results:
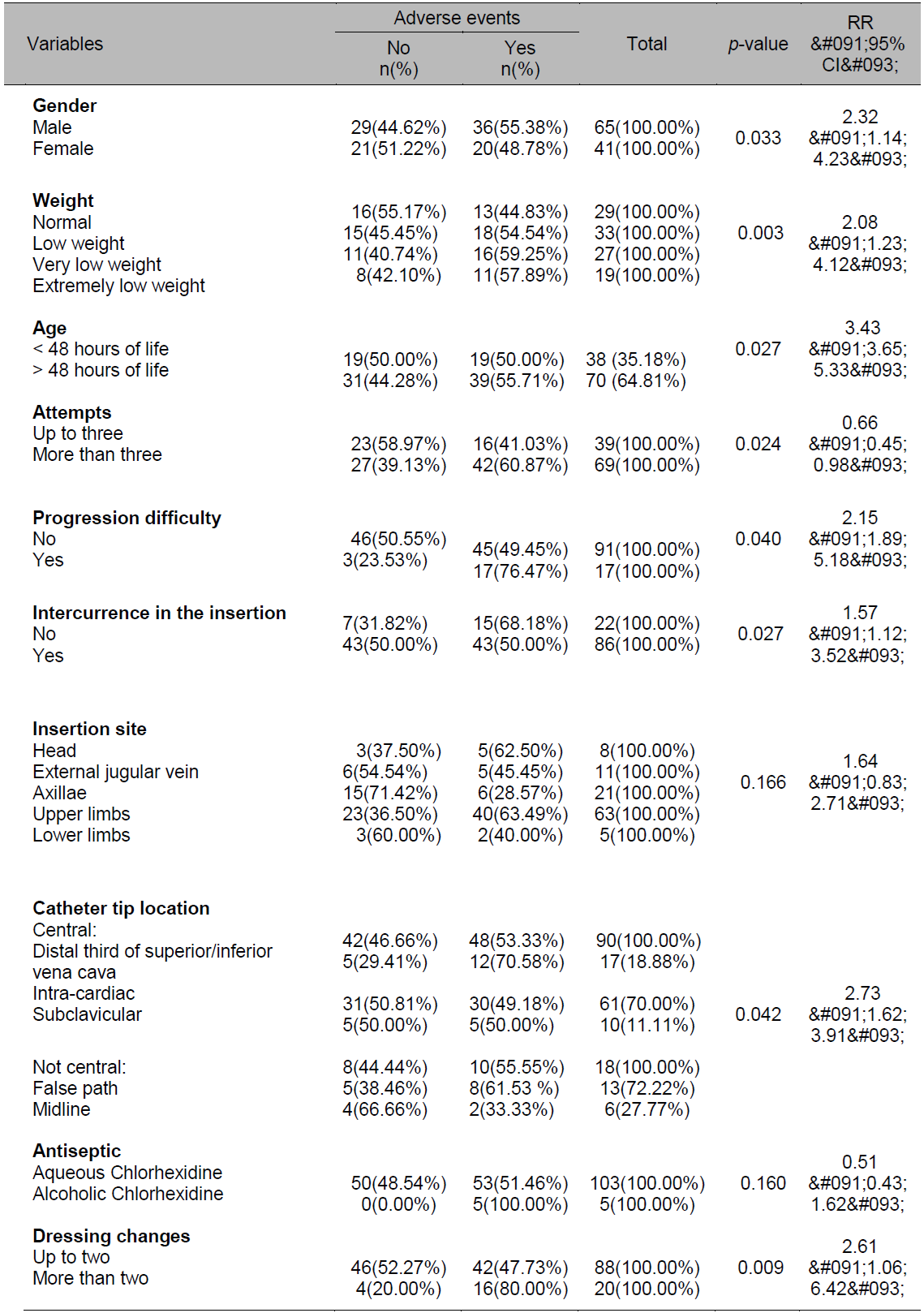
The prevalence of adverse events in newborns was 53.70%, associated with the following variables: male gender (p=0.033), weight below 2500 grams (p=0.003), insertion performed after 48 hours of life (p=0.027), more than three puncture attempts (p=0.024), difficulty in inserting the catheter (p=0.040), intercurrence during catheter insertion (p=0.027), over two dressing changes (p=0.009), and non-central position of the device (p=0.042).
Conclusion:
The results indicate the need for strategies to prevent adverse events, with emphasis on continuing education and on the improvement of skills regarding the use of this device.
Key words: Central Venous Catheterization; Neonatal Nursing; Neonatal Intensive Care Unit; Risk Factors; Patient Safety
INTRODUCTION
In view of the complexity of the health care provided to critically ill neonates, intravenous therapy, through safe venous access, is a primary resource in the care of this population. Currently, the Peripherally Inserted Central Catheter (PICC) is a widely used alternative for this purpose as it offers a sTable, safe and effective access1)(2.
The PICC is a device introduced through a percutaneous procedure and is inserted up to the distal third of the superior vena cava or proximal to the inferior vena cava. The main benefits of the catheter include the reduction of pain, it avoids too many venous punctures and preserves the newborn’s venous network; its benefits also include the possibility of being inserted at the bedside, for longer periods and with a lower risk of contamination compared to other devices. Its main indications are represented by the administration of antibiotics, Parenteral Nutrition (PN) and chemotherapy3.
Although the complications resulting from the use of the PICC are lower when compared to other catheters, it is necessary to discuss them, as well as to consider the possibility of reformulating conducts and recommendations peculiar to their insertion, maintenance and removal focused on the neonatal and pediatric segment, in order to ensure patient safety4.
In this context, this complex process requires knowledge and technical-scientific training of the team, as well as knowledge of the stages of indication, insertion, maintenance and removal of the catheter to employ safe procedures and technologies to minimize Adverse Events (AEs) that may arise due to improper use5)(6.
A study carried out at the Neonatal Intensive Care Unit (NICU) of the Intermountain Medical Center in the state of Utah, USA, showed that, although the PICC requires nurses potentially trained for the insertion, as well as for ratifying the position through a radiographic evaluation, the history of the procedure is still not very positive7. In order to corroborate the basic premise regarding the possibility of successfully using the catheter, a number of research studies revealed that there are significantly fewer incidents when the training of the professionals is carried out in an appropriate, effective and continuous manner8)(9.
With regard to the PICC, it is necessary to consider its complications represented by events such as obstruction, leakage, rupture, infection, thrombosis and migration of the catheter tip. These correspond to 13% to 60% of the complications related to that population. These obstacles result in the reduction of the period using the catheter and, consequently, in failure in the drug therapy and even in the neonates’ survival10. Thus, it is essential that the professionals identify these factors early to provide quality care based on scientific knowledge, which justifies this study.
The relevance of the study is that outcome indicators such as the AEs are fundamental tools of quality, as they signal aspects of care that can be improved, making care safer.
Therefore, this study aimed to identify the factors associated with the occurrence of adverse events by a peripherally inserted central catheter in newborns.
MATERIAL AND METHOD
This is a quantitative, cross-sectional, and descriptive study carried out in a university hospital that is a reference in high-risk maternal and child care, located in a capital city in northeastern Brazil.
To calculate the sample, the population of neonates admitted to the NICU in 2014 using PICCs was used to calculate the sample, corresponding to 297. Thus, the calculation for finite populations was used11. The parameters for the sample calculation were the following: confidence level of 95%, sample error of 5%, and population of 297, resulting in a sample of 108 patients.
The inclusion criteria adopted included the following: neonates without any type of congenital anomaly with loss of skin integrity and with no diagnosis of blood coagulation disorders. The exclusion criteria included the following: neonates who had their catheter inserted in an institution other than the one in the study, in view of possible divergences in the procedure routine. It should be noted that only the first catheter inserted in the newborn was included in the sample. The participants were part of a convenience sample and the data were collected by the researcher herself.
Information was collected from February 1st to November 31st, 2016. The unit has a protocol for insertion, maintenance and removal of the PICC and nurses qualified for the insertion and use of the catheter.
The researcher analyzed the associations of adverse events with the following variables: gender, weight, length of hospital stay, number of attempts, difficulty in the insertion, complications in the insertion, insertion site, location of the catheter tip, antiseptic used and number of dressing changes.
The data were tabulated and analyzed using descriptive and inferential statistics. The Chi-square test, Fisher’s exact test and logistic regression were used, using the Wald test for a significance level of 5%. The Statistical Package for the Social Sciences (SPSS), version 20.0, was used.
The research was approved by the Research Ethics Committee of the Federal University of Rio Grande do Norte (Universidade Federal do Rio Grande do Norte, UFRN), under CAAE No. 48990515.0.0000.5292.
RESULTS
There was a predominance of males (60.19%) and those born by cesarean section (74.07%). Regarding the insertion of the catheter, 30.56% of the newborns (NBs) were underweight and had a gestational age over 32 weeks (56.48%). It was observed that 64.81% of the catheters were inserted after 48 hours of life, with the following as main indications: antibiotic therapy (47.94%) and parenteral nutrition (19.86%).
The upper limbs were preferentially chosen for insertion (58.33%). Of all the complications observed at the insertion of the PICC, it was observed that 15.74% of the catheters were hard to move during their introduction and that 4.63% of the NBs presented bleeding, whether moderate or abundant, or changes in their vital signs (bradycardia/tachycardia or drop in oxygen saturation).
46% of the records in the medical chart, for pain management during the procedure, the use of non-nutritive suction with 20% glucose, facilitated tucking and, in specific cases, sedation.
Immediately after the insertion of the PICC, a radiography confirming the location of the catheter tip is performed, and then the intravenous infusion is initiated through the device. It is noteworthy that 15.74% of the catheters were located in the distal third of the superior or inferior vena cava. It should be noted that 56.48% of the PICCs were located at the intra-cardiac level, making it necessary to reposition the catheter in order to avoid cardiac complications.
At the study institution, nurses used aqueous chlorhexidine (95.37%) for the antisepsis of dressing changes. Regarding the number of dressing changes, 81.48% of the catheters had less than two changes during the entire use of the PICC. According to the NICU routine, the first dressing is performed 48 hours after the procedure and the remaining only in the presence of dirt or displacement. The mean length of use was 12.6 days, ranging from 1 to 89 days.
It is noteworthy that 53.70% of the catheters had AEs (53.70%), namely: occlusion (31.81%), infiltration (19.31%), phlebitis (17.04%), resistance (9.09%), rupture (9.09%), externalization (9.09%), suspected infection (2.27%), and skin maceration (2.27%).
Regarding the relative risk, it is observed that the risk of incidence of AEs in male NBs, with a weight below 2500 grams, procedure performed after 48 hours of life, difficulty in moving the catheter, presence of complications (bleeding or change in vital signs) during insertion, non-central position and number of dressing changes higher than two, exceeds 2.32; 2.08; 3.43; 1.57; 2.15; 2.58 and 2.31 times, respectively, that of a female patient, of normal weight, with less than 48 hours of life, when the catheter was not difficult to move, and who did not have major bleeding or show changes in the vital signs in the insertion, or with a centrally located catheter and with a number of dressing changes up to two times (Table 1).
In addition, the risk of AEs in patients with more than two attempts increases by 80% with respect to that of a patient with up to one attempt.
Logistic regression analysis was applied, using the Wald test for a significance level of 5%, as shown in Table 2.
Table 2 - Logistic regression analysis for the adverse events in newborns with PICCs in Natal, RN), 2016.
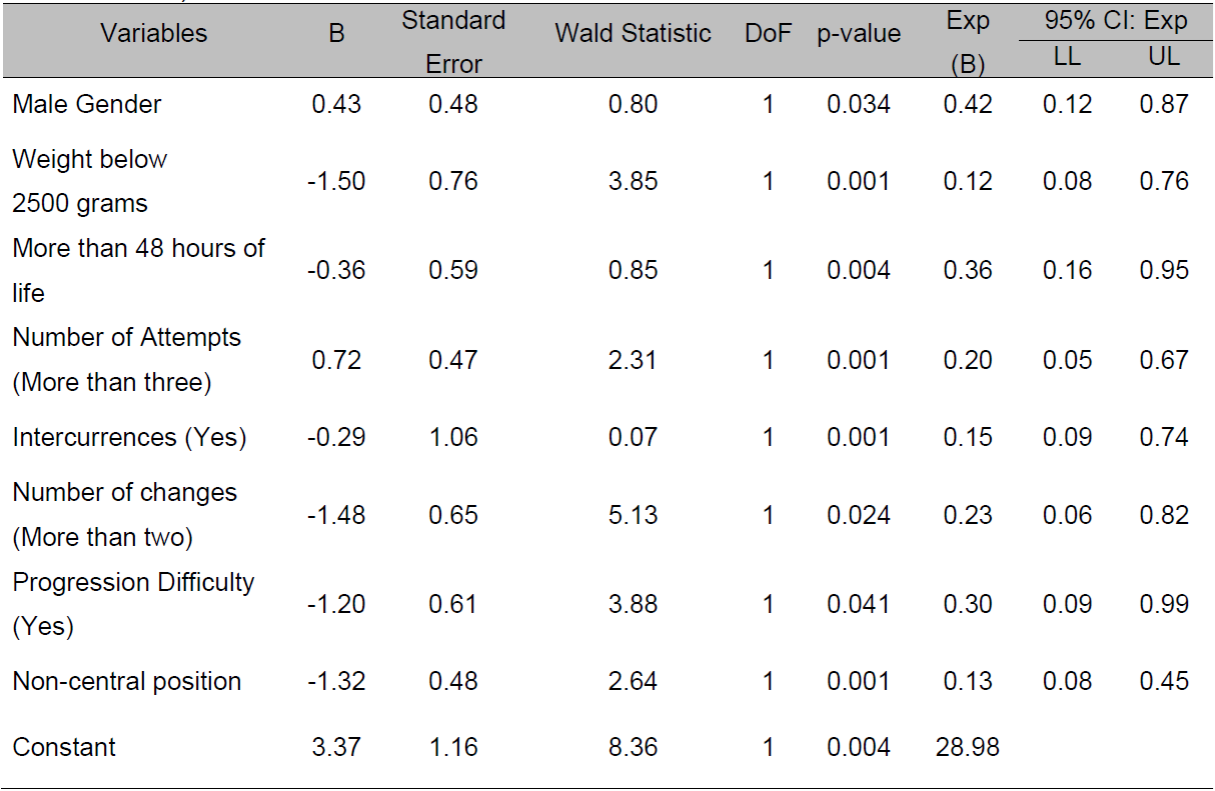
It was identified that the probability of AEs in female NBs, with normal weight, less than 48 hours of life, up to three insertion attempts, no intercurrences, up to two dressing changes, with no difficulty in moving the catheter and position at central level, reduced by 58%, 88%, 64%, 80%, 85%, 77%, 70%, 87%, respectively, compared to male patients, with weight below 2500 grams, procedure performed after 48 hours of life, over three insertion attempts, presence of intercurrences, more than two dressing changes, difficulty in moving the catheter and central location of the catheter.
DISCUSSION
When male gender, low weight, length of hospital stay, number of attempts, presence of complications during insertion of the PICC, number of dressing changes (over two), difficulty in moving the catheter, and non-central position of the device were associated with the occurrence of an adverse event, a significant difference was observed.
These characteristics indicate similarities with the cohort study that investigated the association between intravenous therapy and non-elective removal of 97 peripherally inserted central catheters in newborns, which showed a mean weight below 2000 g, male (59; 60.8%), prematurity (87; 89.7%), respiratory disorder (70; 70.2%), heart disease (16; 16.5%), septicemia (15; 15.5%), gastrointestinal disorder (9; 9.7%), and hydroelectrolytic disorder (5; 5.2%)12. A descriptive cohort study design carried out in a NICU in the Netherlands verified the association between male gender and the occurrence of central line-associated bloodstream infections13.
An epidemiological study carried out in a hospital in Minas Gerais that analyzed the factors associated with infection in 291 peripherally inserted central catheters in newborns admitted to the NICU verified the association of withdrawal due to suspected infection with prematurity, birth weight up to 1500 grams, non-central position of the catheter and time of use over 30 days. It should be noted that the following remained independently associated: weight below 2500 grams at the time of insertion and time of use of the catheter14.
The literature indicate that the PICC must be inserted in the first 48 hours of life, depending on the clinical conditions of the newborn, since the venous network is intact15. The insertion of the PICC in the neonate’s first days of life makes it easier to move the catheter and reduces repeated peripheral venous punctures16.
Corroborating with this research, a study that analyzed 244 insertions of PICCs in an NICU identified that the mean of insertion attempts varied from one to five, which was associated with failure to move the catheter, obstruction, externalization, leakage, phlebitis, and infiltration17. The number of attempts should be monitored during catheter insertion, since the risk of complications also increases as the number of attempts increases18)(19.
Still regarding the non-elective removal of the PICC and the non-central position of the device, a study showed that those whose tip location is not central are three times more likely to be non-electively removed and removed due to a complication when compared to the PICCs with the tip in a central position20.
A research study carried out with children to define the distance calculation formula, based on age, gender, weight, size, and body surface area, concluded that the predictive linear equation to determine the appropriate size for the insertion of the central venous catheter depends only on the body surface area and on a constant21.
The local insertion variable was not statistically significant. However, a study that retrospectively assessed the incidence of complications related to the PICC in a large pediatric tertiary center identified an association between non-infectious complications and the insertion site22.
Regarding the number of dressing changes, minimal manipulation is necessary, since it ensures less trauma to the newborn’s epidermis to protect skin integrity23. It is also necessary to analyze the frequency of these changes, since the risk of displacement of the catheter is greater than the benefits of the dressing change24)(25.
In a prospective cohort study with a sample of 524 PICC lines inserted in 436 neonates admitted to a tertiary-level NICU in a Brazilian hospital, it was found that diagnoses of transient metabolic disorder (hypoglycemia, calcium, magnesium, sodium or potassium disorders or dehydration), previous PICC insertions, use of double-lumen polyurethane catheter, location of the tip in a non-central region, and infusion of multiple intravenous solutions in mono-lumen catheter corresponded to the predictive factors of non-elective removal19.
Finally, the use of the PICC has become an integral and extremely important part of monitoring newborns, who need intensive care in most hospital units. Thus, care measures for the maintenance of the PICC must be reinforced, such as hand hygiene, the use of antiseptic, the sterile technique during dressing changes, and the periodic training of the team who handles the device.
CONCLUSIONS
This study verified the high occurrence of adverse events related to the use of PICCs in high-risk newborns. The variables associated with the complications were the following: gender of the baby (male), weight, over 48 hours of life, number of attempts (over three), intercurrence during the insertion of the PICC, number of dressing changes (over two), difficulty in moving the catheter, and non-central position of the device.
In view of the above, this study supports reflection, as well as the practice of Nursing. Although the catheter mentioned is a viable option for neonatal vascular access, nurses’ knowledge about potential and more prevalent adverse effects resulting from the technique ensure better clinical judgment, which interferes directly with the quality of care provided and preserves patient safety.
REFERENCIAS
1. Sharpe E, Kuhn L, Ratz D, Krein SL, Chopra V. Neonatal Peripherally Inserted Central Catheter Practices and Providers: Results From the Neonatal PICC 1 Survey. Adv Neonatal Care [Internet]. 2017 [acesso em: 05 jun. 2018];17(3):209-221. Disponível em: https://www.ncbi.nlm.nih.gov/pubmed/28045704. [ Links ]
2. Ling Q, Chen H, Tang M, Qu Y, Tang B. Accuracy and Safety Study of Intracavitary Electrocardiographic Guidance for Peripherally Inserted Central Catheter Placement in Neonates. J Perinat Neonatal Nurs [Internet]. 2019 [acesso em: 05 jun. 2018];33(1):89-95. Disponível em: https://www.ncbi.nlm.nih.gov/pubmed/30676468. [ Links ]
3. Di Santo MK, Takemoto D, et al. Peripherally inserted central venous catheters: alternative or first choice vascular access?. J Vasc Bras [Internet]. 2017 [acesso em: 10 jun. 2018];16(2):104-112. Disponível em: http://dx.doi.org/10.1590/1677-5449.011516. [ Links ]
4. Chopra V, Flanders AS, Saint S, Woller SC, O'Grady NP, Safdar N, et al. The Michigan appropriateness guide for intravenous catheters (MAGIC): results from a multispecialty panel using the RAND/UCLA appropriateness method. Ann Intern Med [Internet]. 2015 [acesso em: 15 jun. 2018];15;163(6 Suppl):S1-40. Disponível em: https://doi.org/10.7326/M15-0744. [ Links ]
5. Chen IL, Ou-Yang MC, Chen FS, Chung MY, Chen CC, Liu YC, et al. The equations of the inserted length of percutaneous central venous catheters on neonates in NICU. PediatrNeonatol [Internet]. 2018 [acesso em 20 jul. 2018]; pii: S1875-9572(18)30283-3. Disponível em: https://www.ncbi.nlm.nih.gov/pubmed/30217481. [ Links ]
6. Rosche N, Stehr W. Evaluation of a Magnetic Tracking and Electrocardiogram-based Tip Confirmation System for Peripherally Inserted Central Catheters in Pediatric Patients. J Infus Nurs [Internet]. 2018 [acesso em 02 ago. 2018]; 41(5):301-8. Disponível em: https://www.ncbi.nlm.nih.gov/pubmed/30188452. [ Links ]
7. Chenoweth KB, Guo JW, Chan B. The Extended Dwell Peripheral Intravenous Catheter Is an Alternative Method of NICU Intravenous Access. Adv Neonatal Care [Internet]. 2018 [acesso em 10 ago. 2018];18(4):295-30. Disponível em: https://www.ncbi.nlm.nih.gov/pubmed/29847401. [ Links ]
8. Dongara AR, Patel DV, Nimbalkar SM, Potana N, Nimbalkar AS. Umbilical Venous Catheter Versus Peripherally Inserted Central Catheter in Neonates: A Randomized Controlled Trial. J Trop Pediatr [Internet]. 2017 [acesso em 20 ago. 2018]; 1;63(5):374-9. Disponível em: https://www.ncbi.nlm.nih.gov/pubmed/28077611. [ Links ]
9. Vachharajani AJ, Vachharajani NA, Morris H, Niesen A, Elward A, Linck DA, et al. Reducing peripherally inserted central catheters in the neonatal intensive care unit. J Perinatol [Internet]. 2017 [acesso em 05 set. 2018];37(4):409-413. Disponível em: https://www.ncbi.nlm.nih.gov/pubmed/28079867. [ Links ]
10. Ling QY, Chen H, Tang M, Qu Y, Tang BZ. Efficiency of electrocardiogram monitor for positioning the catheter tip in peripherally inserted central catheter placement in neonates. Zhongguo Dang Dai ErKeZaZhi [Internet]. 2018 [acesso em 16 set. 2018];20(5):363-7. Disponível em: https://www.ncbi.nlm.nih.gov/pubmed/29764571. [ Links ]
11. Vieira S. Introdução à Bioestatística. 5th ed. Rio de Janeiro: Elsevier; 2015. [ Links ]
12. Costa P, Silva MN, Kimura AF. Intravenous therapy and non-elective removal of epicutaneous catheters: a cohort study of neonates. Online Braz J Nurs [Internet]. 2014 [acesso em 05 out. 2018]; 13(2):129-38. Disponível em: http://www.objnursing.uff.br/index.php/nursing/article/view/4572. [ Links ]
13. Dubbink-Verheij GH, Bekker V, Pelsma ICM, van Zwet EW, Smits-Wintjens VEHJ, Steggerda SJ, te Pas AB and Lopriore E. Blood stream Infection Incidence of Different Central Venous Catheters in Neonates: A Descriptive Cohort Study. Front. Pediatr [Internet]. 2017 [acesso em 18 out. 2018];5:142. Disponível em: http://dx.doi.org/10.3389/fped.2017.00142. [ Links ]
14. Duarte ED, Pimenta AM, Silva BCN, Paula CM. Fatores associados à infecção pelo uso do cateter central de inserção periférica em Unidade de Terapia Intensiva Neonatal. Rev Esc Enferm USP [Internet]. 2013 [acesso em 15 nov. 2018]; 47(3):547-54. Disponível em: http://www.scielo.br/pdf/reeusp/v47n3/0080-6234-reeusp-47-3-00547.pdf. [ Links ]
15. Uygun I. Peripherally inserted central catheter in neonates: A safe and easy insertion technique. J Pediatr Surg [Internet]. 2016 [acesso em 02 dez 2018];51(1):188-91. Disponível em: https://www.ncbi.nlm.nih.gov/pubmed/26364881. [ Links ]
16. Johnson KN, Thomas T, Grove J, Jarboe MD. Insertion of peripherally inserted central catheters in neonates less than 1.5 kg using ultrasound guidance. Pediatr Surg Int [Internet]. 2016 [acesso em 17 dez 2018];32(11):1053-1057. Disponível em: https://www.ncbi.nlm.nih.gov/pubmed/27590475. [ Links ]
17. Yu X, Yue S, Wang M, Cao C, Liao Z, Ding Y, et al. Risk Factors Related to Peripherally Inserted Central Venous Catheter Nonselective Removal in Neonates. Biomed Res Int [Internet]. 2018 [acesso em 12 fev 2019]; 30;2018:3769376. Disponível em: https://www.ncbi.nlm.nih.gov/pubmed/30003096. [ Links ]
18. Silva R, Lui A, Ferreira H, Franca A, Lala E, Vieira C. Analys in the use of peripherally inserted central cateter in neonatology. Journal of Nursing UFPE on line [Internet]. 2016 [acesso em 24 fev 2019];10(2):796-804. Disponível em: https://periodicos.ufpe.br/revistas/revistaenfermagem/article/view/11022. [ Links ]
19. Costa P, Kimura AF, Brandon DH, Damiani LP. Predictors of non elective removal of peripherally inserted central catheters in infants. Biol Res Nurs [Internet]. 2016 [acesso em 04 fev 2019]; 18(2):173-80. Disponível em: https://www.ncbi.nlm.nih.gov/pubmed/26134427. [ Links ]
20. Litz CN, Tropf JG, Danielson PD, Chandler NM. The idle central venous catheter in the NICU: When should it be removed? J PediatrSurg [Internet]. 2018 [acesso em 16 fev 2019];Jul;53(7):1414-1416. Disponível em: https://www.ncbi.nlm.nih.gov/pubmed/29198897. [ Links ]
21. Stroud A, Zalieckas J, Tan C, Tracy S, Zurakowski D, Mooney DP. Simple formulas to determine optimal subclavian central venous catheter tip placement in infants and children. J Pediatr Surgery [Internet]. 2014 [acesso em 10 mai 2019];49:1109-112. Disponível em: https://www.ncbi.nlm.nih.gov/pubmed/24952798. [ Links ]
22. Dasgupta N, Patel MN, Racadio JM, Johnson ND, Lungren MP. Comparison of complications between pediatric peripherally inserted central catheter placement techniques. Pediatr Radiol [Internet]. 2016 [acesso em 14 mai 2019];46(10):1439-43. Disponível em: https://www.ncbi.nlm.nih.gov/pubmed/27126700. [ Links ]
23. Lui AML, Zilly A, França AFO, Ferreira H, Toninato APC, da Silva RMM. Care and limitations in the management of the peripherally inserted central catheter in neonatology. Revista de Enfermagem do Centro-Oeste Mineiro [Internet]. 2018 [acesso em 16 mai 2019 ]; 8:e1918. Disponível em: http://www.seer.ufsj.edu.br/index.php/recom/article/view/1918/1901. [ Links ]
24. Gupta R, Drendel AL, Hoffmann RG, Quijano CV, Uhing MR. Migration of Central Venous Catheters in Neonates: A Radiographic Assessment. Am J Perinatol [Internet]. 2016 [acesso em 20 mai 2019];33(6):600-4. Disponível em: https://www.ncbi.nlm.nih.gov/pubmed/26731179. [ Links ]
25. Souza RRB, Alves VH, Rodrigues DP, Dames LJP, Medeiros FVA, Paiva ED. The knowledge of nurses in terms of the peripherally inserted central catheter: a descriptive study. Online braz j nurs [Internet]. 2016 [acesso em 20 mai 2019];15(1):21-31. Disponível em: http://www.objnursing.uff.br/index.php/nursing/article/view/5298. [ Links ]
Received: July 04, 2019; Accepted: August 14, 2019











 texto em
texto em