Meu SciELO
Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Enfermería Global
versão On-line ISSN 1695-6141
Enferm. glob. vol.19 no.59 Murcia Jul. 2020 Epub 10-Ago-2020
https://dx.doi.org/10.6018/eglobal.406691
Originals
Colonization by ESKAPES and clinical characteristics of critically ill patients
1 Profesora, Maestra y orientadora del curso de graduación en Enfermería de la Universidad Paranaense - Unipar. Francisco Beltrão, Paraná, Brasil. franciele.ns@prof.unipar.br
2 Enfermera, egresada Curso de Enfermería de la Universidad Paranaense - Unipar. Francisco Beltrão, Paraná, Brasil.
3 Enfermero, Graduado por la Universidad Paranaense - Unipar. Francisco Beltrão, Paraná, Brasil.
4 Discente del Curso de Enfermería de la Universidad Paranaense - Unipar. Francisco Beltrão, Paraná, Brasil.
5 Farmacéutica, Egresada del curso de Graduación en Farmacia de la Universidad Paranaense - Unipar. Francisco Beltrão, Paraná, Brasil.
Objective:
To identify colonization by ESKAPES and clinical characteristics of patients admitted in Adult Intensive Care Unit of a mixed hospital in Paraná.
Method:
Field research, descriptive, documentary and experimental quantitative approach, developed in adult Intensive Care Unit of a mixed hospital in Southwest Paraná, Brazil. The study population consisted of patients with admission from 48 hours in the Intensive Care Unit, from April to August 2018 and April to August 2019. The sample has 102 individuals. For the collection of clinical data, a checklist was used and for microbiological analysis the sample was collected from nasal and oral cavities and tracheal secretion. The analysis of clinical data occurred through the Statistical Package for the Social Sciences software. Descriptive frequency and chi-square test, considering significant p <0,05.
Results:
A total of 102 patients admitted to the Intensive Care Unit during the period studied were evaluated. On these ones, 57 (55,8%) were colonized by pathogenic microorganisms. Regarding the colonization of microorganisms, there was predominance of Staphylococcus aureus (61,4%), followed by Klebsiella pneumoniae (40,4%), Pseudomonas aeruginosa (26,3%) and Staphylococcus epidermidis (21,1%). It is noteworthy that Klebsiella pneumoniae and Staphylococcus aureus were present in the three regions evaluated.
Conclusion:
The study identified the presence of colonization in critically ill patients studied, being this colonization, mostly, resistant bacteria belonging to the ESKAPE group.
Key words: Intensive Care Units; Bacteria; Drug Resistance Microbial; Infection
INTRODUCTION
The Intensive Care Unit (ICU) in a hospital is the environment for critically ill patients. Generally, these individuals are more likely to acquire nosocomial infections, due to their fragile state, the use of invasive procedures, high doses of medication and longer hospital stay in a contaminated and colonized place by several microorganisms, many of which are multi-resistant 1)(2)(3.
Multidrug-resistant microorganisms are considered a serious public health problem, since they often create mechanisms to minimize or to interrupt the antimicrobial action, thus causing a challenge for health professionals when choosing the appropriate treatment. Among these microorganisms, the group called ESKAPE stands out, an acronym for the following bacteria: Enterococcus faecium, Staphylococcus aureus, Klebsiella pneumoniae, Acinetobacter baumannii, Pseudomonas aeruginosa and Enterobacter spp4.
In 2017 the World Health Organization (WHO) published a global list of antibiotic-resistant bacteria that should be given priority in the investigation of new drugs. In this list, ESKAPE bacteria occupy the top positions, classified as critically priority (A. baumannii, P. aeruginosa, K. pneumoniae and Enterobacter spp.) and highly priority (E. faecium and S. aureus) for research and discoveries that minimize morbidity and mortality from these infectious agents 5.
Microbial resistance was listed as one of the ten threats to global health in 2019. About 700,000 people die each year from infections caused by resistant pathogens, and it is believed that by 2050 that number will reach 10 million deaths, generating an expense around $ 100 trillion 6)(7. In a retrospective study, carried out in Rome, 9720 cases of bloodstream infection were identified in the nine-year period, of which 61.7% were caused by bacteria in the ESKAPE group 8.
It is worth noting that not all patients colonized by resistant microorganisms show signs of infection, however, they present themselves as a reservoir, potential disseminators, in addition to being more vulnerable to infectious conditions 9.
Thus, the importance of screening these patients and timely implementation of preventive measures is emphasized, in view of the identification of multi-resistant colonizations in the community, that is, the patient can either be colonized in the hospital environment, or have already been colonized at the community level 10)(11)(12.
On the other hand, the hospital environment remains one of the main sources of pathogens, especially those resistant to antibiotics 13. Given the above, the question arises: is there colonization in critically ill patients and what are the microorganisms of clinical and epidemiological importance that colonize patients admitted to an ICU? Furthermore, are any clinical features related to colonization?
Therefore, this research aimed to identify colonization by ESKAPES and clinical characteristics of patients admitted to an Adult ICU of a mixed hospital in Paraná.
MATERIAL AND METHOD
This is a field research, which is descriptive, prospective, documentary and experimental with a quantitative approach, developed in an adult ICU of a mixed hospital in Southwest Paraná, Brazil. This hospital serves by private means, agreements and the Unified Health System (SUS); it has 10 ICU beds, providing specialized assistance with constant monitoring.
The study population consisted of patients admitted to the ICU after 48 hours, with the signing of the Free and Informed Consent Term, from April to August 2018 and from April to August 2019. The sample excluded patients with a stay of less than 48 hours. It totaled 102 individuals hospitalized in the mentioned period.
For the collection of clinical data, a checklist was used, developed by the researchers, based on the relevant literature. The form contained the following variables: age, sex, origin (clinical, surgical, trauma), etiology of ICU admission, chronic diseases, source of infection, use of vasoactive drugs, instituted antibiotic therapy, initial blood cultures, isolated microorganism in blood culture, need renal replacement therapy, use of mechanical ventilation (MV) and clinical outcome.
For microbiological analysis, samples were collected from the following body regions: nasal, oral and tracheal cavities. To collect the sample, a sterile swab was rolled over the established site, and then the swab was immersed in a tube (eppendorf, 2ml) with 1ml of sterile buffered saline solution, which was shaken for better release of microorganisms. After collection, the sample was sent for microbiological analysis at the Microbiology laboratory of Universidade Paranaense.
The samples were identified by macroscopic and microscopic examination. The macroscopic examination of the culture allows an analysis of the morphological characteristics, size and color of the colony in selective and simple media. One can also verify the purity of the culture, essential for the identification of the species. The microscopic examination was done using Gram stain, observing the morphological and tinting aspects of the microorganisms. In addition, catalase-coagulase tests, standardized Enterokit tests for Gram-negative bacilli and antibiograms for testing microbial resistance to antibiotics were performed.
The analysis of the clinical data of the respondents was carried out with the support of the statistical program Statistical Package for the Social Sciences (SPSS 25.0). Descriptive frequency and chi-square test were performed, considering significant p <0.05.
As it is a research that involves human beings, the referred study was previously submitted to the evaluation of the Ethics Committee in Research with Human Beings of Universidade Paranaense - Unipar, and the opinion was released as approved under protocol 2.135.782/2017, as well as was requested the declaration of permission to use data from the institution chosen as the study environment, before its inclusion in it. Therefore, all ethical and legal principles were preserved, in accordance with resolution 466/2012 of the National Health Council.
RESULTS
102 patients admitted to the ICU during the research period were evaluated. On these ones, 57 (55.8%) were colonized by pathogenic microorganisms.
Table 1 presents the sample's sociodemographic and clinical profile. Among those studied (n=102), 60 (58.8%) were male and 42 (41.2%) female, the predominant age group was elderly people with 63 (61.7%), 18 (17, 6%) smokers and 14 (13.7%) alcohol users.
The length of stay of patients was up to 15 days for 66 (64.7%) of the cases and more than 15 days for 36 (35.3%). Of these, 77 were hospitalized (75.5%). As the etiology of admission, heart disease prevailed 25 (24.5%), followed by septic shock with 19 (18.7%).
In the variable chronic diseases, 68 (66.7%) patients had some previous pathology, the most cited being systemic arterial hypertension (SAH) in 53 (52.4%), chronic obstructive pulmonary disease (COPD) in 10 (9, 9%) and diabetes mellitus (DM) in 9 (8.9%).
MV was used in 75 patients (73.5%), vasoactive drugs in 46 (45.1%) and hemodialysis in 3 (2.9%).
Table 1: Sociodemographic and clinical profile of patients admitted to the Intensive Care Unit, Francisco Beltrão, Paraná, Brazil, 2019. (n= 102)
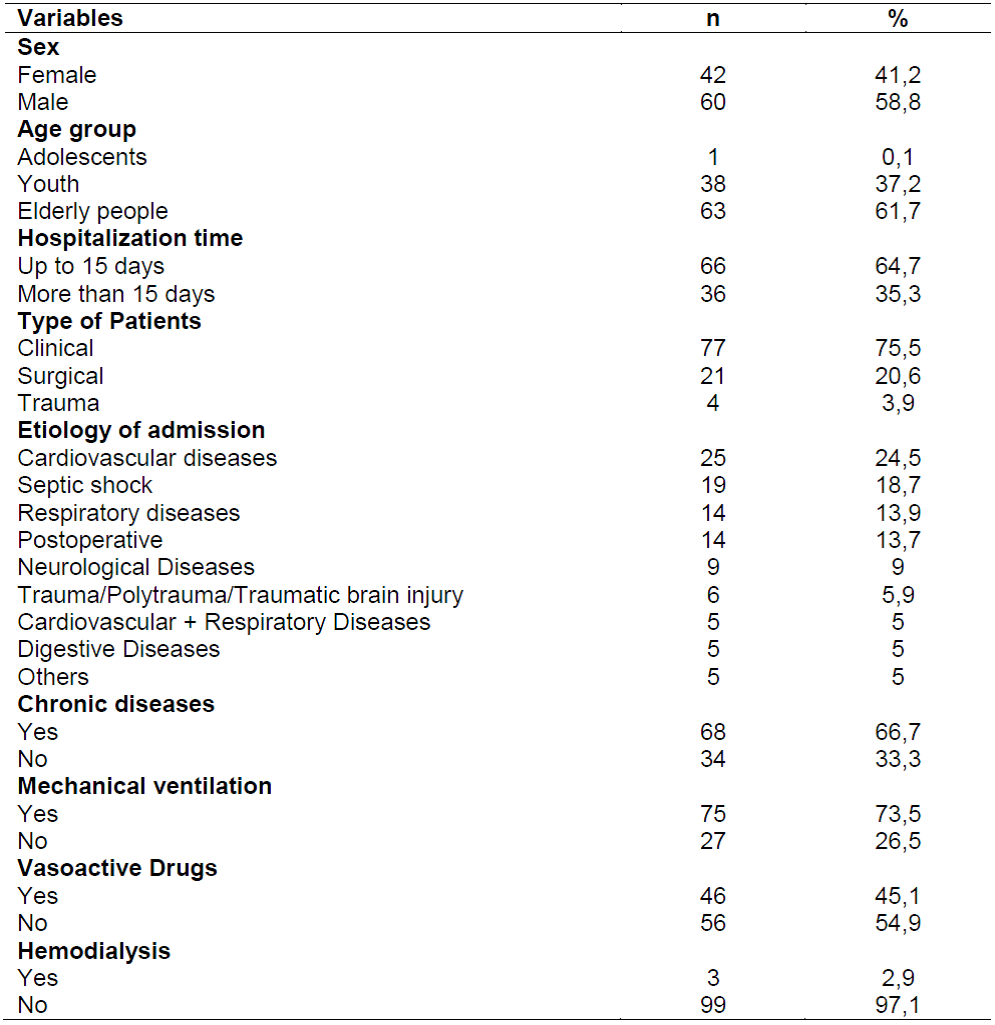
Source: Research data, authors (2019).
About the 102 patients evaluated, only 13 (12.7%) received initial blood cultures and surveillance cultures performed at the institution. Four patients showed positive results, one of which had two distinct pathogens. During hospitalization, S. aureus were identified in 1 (1.0%), P. aeruginosa, 1 (1.0%), K. pneumoniae, 1 (1.0%), and Staphylococcus haemolyticus and Candida albicans in 1 (1.0%).
In view of the antibiotic therapy used, 42.4% used two classes of antimicrobials concomitantly, and the others used isolated therapy; 17.6% did not use antibiotics, as shown in Graph 1.

Graph 1: Antibiotic therapy prescribed during admission to the Intensive Care Unit, Francisco Beltrão, Paraná, Brazil, 2019.
Regarding the colonization of microorganisms, there was a predominance of S. aureus (61.4%), followed by K. pneumoniae (40.4%), P. aeruginosa (26.3%) and Staphylococcus epidermidis (21.1%), as shown in Graph 2.
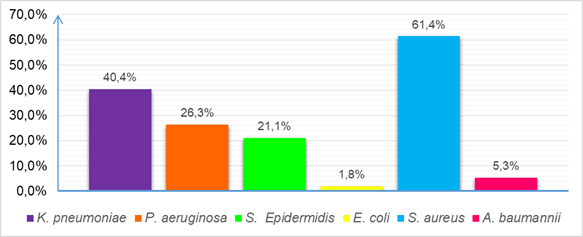
Graph 2: Colonization by microorganisms in patients admitted to the Intensive Care Unit, Francisco Beltrão, Paraná, Brazil, 2019. (n= 57)
Graph 3 shows colonization by body region. It is noticed that K. pneumoniae and S. aureus were present in the three regions evaluated, with K. pneumoniae predominating in the oral cavity (28.1%), while S. aureus prevailed in the nasal cavity (42.1%). P. aeruginosa and S. epidermidis were found only in the nasal and oral cavities, with P. aeruginosa growing more in the oral cavity (17.5%) and S. epidermidis in the nasal (21.1%). Escherichia coli and A. baumannii colonized only the nasal cavity (1.8% and 3.5%, respectively).

Graph 3: Colonization of isolated pathogenic microorganisms by evaluated body cavity, from patients admitted to the Intensive Care Unit, Francisco Beltrão, Paraná, Brazil, 2019. (n= 57)
Regarding antimicrobial resistance, of the 35 colonized by S. aureus, 9 (25.7%) had resistance to erythromycin, clindamycin, ciprofloxacin and cefoxitin. Of the 23 colonized by K. pneumoniae, 8 (34.8%) showed resistance to the antibiotics ceftriaxone, amoxicillin + clavulanate and ceftazidime. While the 15 colonized by P. aeruginosa, 4 (26.7%) showed resistance to ceftazidime, gentamicin, norfloxacin, ertapenem and imipenem.
In addition, the clinical outcome showed 52 (51.0%) patients who were discharged from the hospital, while 50 (49.0%) died.
DISCUSSION
Colonization by pathogenic microorganisms is an important condition to favor infections, especially those related to assistance9, especially when considering patients admitted to the ICU, since they are more exposed, due to their fragile state and the use of multiple drugs and invasive procedures 1.
The data collected showed a male prevalence among hospitalized patients, which is in line with other research in the area 3)(14. Regarding the age group, there was a predominance of the elderly population, which is similar to other studies that show values of 54.6% and 56.9% among those over 60 2)(12.
These findings may be justified by the fact that the male gender is not in the habit of routinely monitoring their health condition, and when they seek health services they are in a state that inspires advanced care. In addition, with advancing age and the senescence process, greater care is needed, due to the fragility of this period 2)(3)(12)(14)(15.
In relation to smoking and drinking, similar data were found in a survey conducted in a public teaching hospital, in which 15% were smokers and 13% were alcoholics. It should be noted that both alcoholism and smoking are considered risk factors, as they worsen the prognosis when associated with chronic diseases, in addition to increasing the incidence of infections 16.
In more than half of the cases, the length of stay was less than 15 days, similar to that found in research conducted in Bahia and Amazonas. In a study conducted in Minas Gerais, it was evident that patients who remained hospitalized for a period greater than or equal to nine days had 32 times more risk than those who remained less than nine days 14)(17)(18.
Each ICU presents a profile of the nature of the hospitalization, according to its public of care and the reference specialty for which the hospital is qualified. This is shown when the prevalence of patients evaluated in this study was of a clinical nature, consistent with another study, while in other studies, 60.6% and 45.3% were surgical and 57.3% were traumatic 2)(3)(14)(17.
The clinical character of the visits is due to the majority profile present, which was that of the elderly people, with chronic diseases, who consequently had a deterioration of their condition, or even, as a result of comorbidities, had clinical complications. It is not necessarily possible to conFigure the probability of colonization in clinical patients as greater, as research shows colonization also in surgical and trauma patients. This characterization only demonstrates the service profile of the unit 2)(14.
In a study carried out in Switzerland, the main etiologies for admission to the ICU were sepsis/infection (26.5%), hemodynamic monitoring after surgery (16.2%) and heart disease (14.9%). Heart disease (33.3%) was also prevalent in a survey conducted in Canoas, which is similar to the data from this study 12)(19).
Cardiovascular diseases are among the main causes of death and are directly linked to the population's lifestyle (20). Likewise, sepsis is a serious problem in the ICU because it increases morbidity and mortality, especially when it progresses to septic shock. The age over 65 years-old, the presence of comorbidities, the use of invasive procedures and a longer ICU stay were described as risk factors for worsening sepsis21.
In relation to the presence of comorbidities, similar data were found in research developed in an ICU of a teaching hospital in which 59% were also carriers of chronic pathologies, and, among the most cited, DM (19.9%), SAH (16 , 3%) and COPD (8.4%). The literature addresses the presence of chronic diseases as a risk factor for microbial colonization 21.
Of the evaluated patients, a large part used MV. A similar value was found in other studies, in which 77.4% and 79.3% used MV during hospital stay. A similar value was also found for the use of vasoactive drugs (41.9%), while for the use of hemodialysis it was higher than that of the study (12.9%) (17, 15). The use of invasive procedures in conjunction with the delicate clinical condition in which the ICU patients are found increases the risks of colonization, and consequently, infection; however, they are necessary for the maintenance of the condition, taking into account the risk/benefit 1.
Surveillance blood cultures were performed in the minority of patients. From these, predominantly S. aureus, P. aeruginosa, K. pneumoniae, S. haemolyticus and C. albicans were isolated. The presence of positivity in cultures does not necessarily indicate the presence of infection, as already mentioned; however, the performance of surveillance cultures is very important in the identification of the microbial profile of the ICUs, thus helping in the correct prescription of antimicrobials, either as a way of treatment or prophylaxis when necessary, as well as to contribute to minimize microbial resistance 2.
Another factor evaluated was the use of antibiotic therapy, widely observed in this sample, as well as in the study carried out in Minas Gerais, in which the applied multivariate analysis showed statistical significance regarding the use of antimicrobials as a risk factor for colonization by resistant microorganisms 18.
In the ICU, the use of antibiotics is essential due to the delicate situation in which the patients are, being used as a prophylaxis method. However, its indiscriminate use implies a greater susceptibility of patients to contract an infection 1. Still in relation to antibiotic therapy, most inpatients made use of two classes of antimicrobials concomitantly, followed by the use of cephalosporins. A study developed in Maranhão corroborates the data found 22.
Combined antibiotic therapy is commonly used to increase the effectiveness of certain antimicrobials, or when treating resistant microorganisms. In addition, cephalosporins in particular are widely used, as they are bactericidal for most bacteria, both gram-positive and gram-negative, within the mechanisms of action of each of their generations 22.
In the microbiological analysis, colonizations of S. aureus, K. pneumoniae, P. aeruginosa, S. epidermidis, E. coli and A. baumannii were identified. These microorganisms were also isolated in other studies, but with variations in prevalence, thereby indicating the variability of the bacterial profile of each treatment unit 1)(2)(3)(14.
S. aureus is a pathogen in the group of gram-positive cocci that is present in the human microbiota and is one of the main microorganisms responsible for causing the most diverse pathologies, from mild skin diseases to serious infections. Transmission occurs through direct contact or with fomites, and the main risk factors are the use of antibiotic therapy and invasive procedures. Something that has caused the concern of health professionals is the spread of methicillin-resistant S. aureus (MRSA), which has been causing major disorders in its treatment 23)(24.
K. pneumoniae is described as an agent of high morbidity and mortality worldwide. Studies show that the mortality rate for K. pneumoniae is around 23.4%. This pathogen is responsible for pneumonia and urinary tract infections. In addition, a major current concern in relation to this bacterium is its production of carbapenemase, that is, K. pneumoniae producing carbapenemase (KPC), an enzyme that hydrolyzes carbapenems 23)(25)(26.
P. aeruginosa is a gram-negative bacillus of epidemiological importance because it is an agent of nosocomial infections, present mainly in pulmonary, urinary and bacteremic infections. It colonizes the respiratory and digestive tract of patients, especially those with prolonged hospitalization, broad-spectrum antibiotic therapy and use of MV 1)(23.
S. epidermidis is a gram-positive coccus that causes bacteremia, urinary tract infections, infections of surgical wounds and catheters. E. coli, on the other hand, is associated with infections of the digestive system, urinary infections, sepsis, meningitis and bacteremia, and is a gram-negative bacillus frequently found in the digestive tract1)(23.
A. baumannii, characterized as a gram-negative cocobacillus, is known as an opportunistic pathogen with high morbidity and mortality. It is commonly found on surfaces and identified in pulmonary infections, especially in patients using MV, urinary and nosocomial infections 1)(23.
Resistant microorganisms are a major concern for critically ill patients. It is worth noting that among the six isolated microorganisms, four are from the ESKAPE group, with this group of bacteria having a great impact on global health, since its various resistance mechanisms restrict effective treatment alternatives for the control of infections 4.
It is essential that the identification of the microbiological profile of each ICU is done, as research shows variations in prevalence in different regions, and that this is related to resistant bacteria and consecutive therapeutic failure. Thus, the importance of choosing an appropriate and effective treatment is shown to treat and contain the spread of pathogenic microorganisms 1)(2.
Regarding the resistance to the tested antimicrobials, in a study conducted in the region of Porto Alegre that analyzed the profile of microbial resistance in three ICUs, S. aureus resistant to clindamycin and ciprofloxacin 1 was also identified. Still, data found in other studies corroborate the presence of K. pneumoniae resistant to ceftriaxone, amoxicillin + clavulanate and ceftazidime and P. aeruginosa resistant to ceftazidime, gentamicin, norfloxacin and imipenem, evidenced in this study 1)(8)(27)(28.
Resistance to antibiotics is growing, a worrying fact, because while multidrug resistance increases, the development of new antimicrobials does not meet the current demand, which recalls not so distant times, when most bacterial infections had unfavorable prognosis 1.
One of the most recent studies in the area reports that if antibiotic resistance is not controlled as soon as possible, infections caused by resistant microorganisms will be the main cause of death in the world in 2050, due to the lack of availability of antibiotics for effective treatment 29.
Still, regarding the clinical outcome, the percentage of discharge was slightly higher than the death. In research conducted in Rio Grande do Norte, similar data were found, in which 57.6% were discharged and 42.4% died 2. On the other hand, some conditions considered sTable worsened during hospitalization, due to the development of infections in the most varied anatomical sites, which directly contributed to the death rate.
It is worth mentioning that the use of antimicrobials associated with invasive procedures and the fragile state, due to senility, chronic diseases and severe clinical conditions, favor the expansion of resistance patterns. It is up to the health teams to be prudent and assertive in the control and prevention of bacterial colonization, thus preventing infections and increasing resistance. In this regard, it is necessary to instigate measures that can prevent and minimize exposure to risk factors for colonization by pathogenic microorganisms 1)(2.
The limitations of the study are highlighted, related to the specificity of the place where the samples were collected and the patients were evaluated, as it is understood that each health institution presents a wide variation in this profile.
CONCLUSIONS
The study identified the presence of colonization in critically ill patients, with colonization, mostly, by resistant bacteria and ESKAPE group (S. aureus, K. pneumoniae, A. baumannii and P. aeruginosa).
Regarding the profile of colonized patients, there was a prevalence of male, elderly people, with associated morbidities and who remained less than 15 days hospitalized.
Finally, some pathogens from the ESKAPE group were identified that presented important resistance mechanisms, and this resistance is considered a serious global health problem.
Thus, it is considered that such inferences may contribute to the characterization of the clinical and microbiological profile of the researched unit, in order to outline a profile of the risk group, and thus, enable the development of new control measures.
REFERENCIAS
1. Basso ME, Pulcinelli, RSR, Aquino ARC, Santos KF. Prevalence of bacterial infections in patients admitted to an intensive care unit. Rev bras anal clin. 2016; 48 (4): 383-388. [ Links ]
2. Araújo PL, Mendonça AEO, Medeiros RA, Souza Neto VL, Nobre TTX, Costa IKF. Prevalence of health assistance infection in patients hospitalized in intensive therapy unit. Enferm glob. 2018; 17 (52): 291-303. [ Links ]
3. Merzoughi L, Barhoumi T, Guizani T, Barhoumi H, Hannachi H, Turki E et al. Nosocomial infections in the Intensive Care Unit: annual incidence rate and clinical aspects. Pan Afr Med J. 2018; 30 (143): 1-8. [ Links ]
4. Esposito S, Simone G. Update on the main MDR pathogens: prevalence and treatment options. Infez Med, 2017; 25 (4): 301-310. [ Links ]
5. WHO. World Health Organization. Global priority list of antibiotic-resistant bacteria to guide research, discovery, and development of new antibiotics. [Internet]. Genebra: WHO; [cited 2017 Feb 27]. Available from: https://www.who.int/medicines/publications/global-priority-list-antibiotic-resistant-bacteria/en/. [ Links ]
6. WHO. World Health Organization. United Nations meeting on antimicrobial resistance. Bull World Health Organ. 2016; 94 (9): 638-639. [ Links ]
7. WHO. World Health Organization. Ten threats to global health in 2019. [Internet]. Genebra: WHO; [cited 2019]. Available from: https://www.who.int/emergencies/ten-threats-to-global-health-in-2019. [ Links ]
8. Angelis G, Fiori B, Menchinelli G, D'Inzeo T, Liotti FM, Morandotti GA et al. Incidence and antimicrobial resistance trends in bloodstream infections caused by ESKAPE and Escherichia coli at a large teaching hospital in Rome, a 9-year analysis (2007-2015). Eur J Clin Microbiol Infect Dis. 2018; 37 (9): 1627-1636. [ Links ]
9. Sun QL, Gu D, Wang Q, Hu Y, Shu L, Hu J et al. Dynamic Colonization of Klebsiella pneumoniae Isolates in Gastrointestinal Tract of Intensive Care Patients. Front Microbiol. 2019; 10: 1-9. [ Links ]
10. Estrada-Román A, Mendo-López R, Astocondor L, Zervos M, García C. Colonization by enterococcal strains resistant to vancomycin in patients from a hospital in Lima, Perú. Rev Peru Med Exp Salud Publica. 2017; 34 (4): 666-671. [ Links ]
11. Santolin C, Sesma AC, Llansa MA, Pintado S, Masso MG, Mangiaterra SM. Rectal colonisation by multiresistant gram-negative bacilli: relevance of early detection in the course of hospitalization. Acta bioquím clín latinoam. 2017; 51 (4): 675-680. [ Links ]
12. Martinez AE, Widmer A, Frei R, Pargger H, Tuchscherer D, Marsch S et al. ESBL-colonization at ICU admission: impact on subsequent infection, carbapenem-consumption, and outcome. Infect Control Hosp Epidemiol. 2019; 40 (4): 408-413. [ Links ]
13. Costa DM, Johani K, Melo DS, Lopes LKO, Lima LKO, Tipple AFV et al. Biofilm contamination of high-touched surfaces in intensive care units: epidemiology and potential impacts. Lett Appl Microbiol. 2019; 68 (4): 269-276. [ Links ]
14. Hespanhol LAB, Ramos SCS, Ribeiro Junior OC, Araújo TS, Martins AB. Infection related to Health Care in an adult Intensive Care Unit. Enferm glob. 2019; 18 (1): 229-241. [ Links ]
15. Vieira AM, Parente EA, Oliveira LS, Queiroz AL, Bezerra ISAM, Rocha HAL et al. Characteristics of deaths of hospitalized patients in Intensive Care Unit of a tertiary hospital. J. Health Biol Sci. 2019; 7 (1): 26-31. [ Links ]
16. Moura JM, Bertolli ES, Pereira RM, Frutuoso IS, Werneck AL, Contrin LM. Sepsis diagnosis in patients after intensive care unity hospitalization. Arq. Ciênc. Saúde. 2017; 24 (3): 55-60. [ Links ]
17. Santos GO, Queiroz RS, Jesus CS, Carneiro JAO, Faria LMA, Fernandes ME et al. Patients admitted to an intensive care unit who do not adopt na antigravity posture have a higher odds of death. Fisioter Pesqui. 2019; 26 (3): 235-240. [ Links ]
18. Arcanjo R, Oliveira AC. Factors connected to axillary colonization by resistant organisms of intensive care unit patients. Rev. Aten. Saúde. 2017; 15 (51): 11-17. [ Links ]
19. Santos LJ, Silveira FS, Müller FF, Araújo HD, Comerlato JB, Silva MC et al. Functional assessment of impatients in the Intensive Care Unit of the University Hospital of Canoas. Fisioter Pesqui. 2017; 24 (4): 437-443. [ Links ]
20. Souza HP, Werneck GL, Medeiros LT, Sabroza PC, Santos JPC. Spatial analysis of causes of death from cardiovascular disease and associated factors in a deployment area of a large development project. Hygeia. 2017; 13 (24): 199-214. [ Links ]
21. Barros LLS, Maia CSF, Monteiro MC. Risk factors associated to sepsis severity in patients in the Intensive Care Unit. Cad. Saúde Colet. 2016; 24 (4): 388-396. [ Links ]
22. Lima Júnior FA, Vieira SEM, Silva BS, Araújo TD, Reis TGM, Miranda JM et al. Profile of antibiotics prescription in an adult intensive care unit at a surgical reference hospital in the state of Maranhão. REAS/ EJCH. 2019; 34: 1-7. [ Links ]
23. Murray PR, Rosenthal KS, Pfaller MA. Microbiologia Médica. 7th ed. Rio de Janeiro: Guanabara Koogan; 2014. [ Links ]
24. Arias CA, Reyes J, Carvajal LP, Rincon S, Diaz L, Panesso D et al. A prospective Cohort Multicenter Study of Molecular Epidemiology and Phylogenomics of Staphylococcus aureus Bacteremia in Nine Latin American Countries. Antimicrob. Agentes chemother. 2017; 61 (10): 1-12. [ Links ]
25. Juan CH, Chuang C, Chen CH, Li L, Lin YT. Clinical characteristics, antimicrobial resistance and capsular types of community-acquired, healthcare-associated, and nosocomial Klebsiella pneumoniae bacteremia. Antimicrob Resist Infect Control. 2019; 8 (1): 1-9. [ Links ]
26. Sanctis G, Ferraris A, Ducatenzeiler L, Benso J, Fernández-Otero L, Angriman F. Risk factors for in-hospital mortality among adult patients infected with colistin-resistant carbapenemase producing Klebsiella pneumoniae: a retrospective cohort study. Rev. chil. Infecto. 2018; 35 (3): 239-45. [ Links ]
27. Merjildo DF, Apac CG, Piérola JZ, Bullon LG. Antimicrobial susceptibility among endotracheal isolates in na intensive care unit in Lima, 2016. Rev Med Hered. 2017; 28: 236-241. [ Links ]
28. Gómez-González JF, Sánchez-Duque JA. Microbiologic profile and antibiotic resistance at na intensive care unit in Pereira, Colombia, 2015. MÉD. UIS. 2018; 31 (2): 9-15. [ Links ]
29. O'neill J. Tackling drug-resistant infections globally: final report and recommendations. Rev Antimicrob Resist. 2016. [ Links ]
Received: December 13, 2019; Accepted: February 17, 2020











 texto em
texto em 


