Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Enfermería Global
versión On-line ISSN 1695-6141
Enferm. glob. vol.19 no.60 Murcia oct. 2020 Epub 21-Dic-2020
https://dx.doi.org/10.6018/eglobal.406401
Originals
Quality of chest compressions in cardiopulmonary resuscitation performed in extreme ambient temperature conditions
1Universidad Católica San Antonio de Murcia. España. marisa.fernandez.gon@gmail.com
2Hospital Comarcal de Vinaroz. Castellón. España.
Under the care of a team of health professionals in an out-of-hospital cardiorespiratory arrest (PCREH), they can be found in conditions in extreme conditions of ambient temperature, depending on the area where they are located, the time of the year, and even the time of day.
Objective:
The objective of this study was to verify whether the efficacy of Cardiopulmonary Resuscitation (CPR) was affected by extreme heat (40ºC) and cold (0ºC) temperature environments, compared to a CPR in ambient temperature (22ºC).
Method:
2 minutes of uninterrupted external chest compressions (ECC) were performed under ambient temperature conditions of 40ºC, 0ºC and 22ºC, in a realistic mannequin Resusci Anne QCPR with SIMPAD.
Results:
30 participants, both people with prior training in CPR (86.7%) and without it (13.3%), were part of the sample, 26 women (86.7%) and 4 men (13.3%), with a mean age of 27.37 ± 8.88 years. No statistically significant differences were found in the efficacy of CPR; but there were differences between the total number of CT (p = 0.042), the average depth of the ECC (p = 0.015) and the average frequency (p = 0.034). The Borg scale of perceived exertion (RPE) showed an average of 4.4 ± 1.303 at 22° C, 4.97 ± 1.402 at 40° C and 4.87 ± 2.08 at 0° C (p> 0.05). There were no significant differences in hair lactate.
Conclusions:
It is concluded that there are no significant differences between the three conditions, although it seems that the cold and room temperatures resemble results and that the heat temperature offers a slight disadvantage of the others.
Key words: cardiopulmonary resuscitation; resuscitator; fatigue; chest compressions; ambient temperature; simulation
INTRODUCTION
Basic cardiopulmonary resuscitation (CPR) is comprised of quality chest or cardiac compressions and assisted ventilations, including the use of the defibrillator. There are 5 components of high-quality CPR such as chest compression fraction (CCF), ECC frequency, ECC depth, chest expansion, or residual compression and ventilation 1. Specifically, the depth will be approximately 5-6 cm in the adult and the frequency> 100 cpm, as well as allowing the chest to re-expand after each compression 2.
If we understand chest compressions as a physical activity for the rescuer, we can define it as intense and of a short duration because, from 1½ to 2 minutes, the rescuer's fatigue increases, and the quality of the compressions begins to decrease significantly 3 4 5 6 7.
The systems that participate in the production of energy in the body are determined by intensity, so, being an intense and short-lived activity, the predominance of the ATP replacement pathway would be the anaerobic glycolytic pathway 8.
In out-of-hospital PCR, healthcare professionals are exposed to any climatic context. In reference to ambient temperature, extreme hot and cold conditions affect the body in different ways. Metabolically, in a hot context, muscular glycogenolysis, glycolysis and the degradation of high energy phosphate during exercise are increased 9. In repeated and intense activities, when the hyperthermic state is reached, the physical performance is diminished; it is suggested that this reduction is related to an increase in core temperature and not to known fatigue metabolic agents 10 11, as well as to the availability of carbohydrates. In contrast, in cold environments an increase in resistance has been observed, probably related to a reduction in glycogenolytic velocity 12.
Physical performance in cold environments is impaired by decreased mechanical, biochemical, and neural functions of the muscle due to a decrease in muscle temperature. On the other hand, it has been observed that in hot environments the performance increases when carrying out an intense activity of short duration. If this activity is repeated, the positive relationship decreases and performance deteriorates13.
The objective of our study was to determine if there are differences in the quality of chest compressions in cardiopulmonary resuscitation depending on the ambient temperature where the CPR is perforMed
METHOD
Analytical comparative study of the quality of chest compressions in simulated cardiopulmonary resuscitation performed on a specific mannequin for CPR under different conditions of ambient temperature performed in the laboratory at the facilities of the Universidad Católica San Antonio de Murcia (UCAM).
Three different tests were performed consisting of performing quality chest compressions uninterruptedly for 2 minutes on a dummy in the ground in each of the tests. The room / laboratory ambient temperature conditions for each of the three tests were 22°, 40° and 0° C respectively. In each of the conditions, an acclimatization of the participant to the ambient temperature of 5 minutes was carried out. During the test, the subjects had no information about the quality of the test or the time elapsed. At the end of the two minutes, they were asked about the degree of perceived effort of the test, according to the Borg scale, and were then measured the lactate in capillary blood by puncturing the index finger. If the two temperature tests were performed in the same session, the participants remained at rest outside the laboratory rooms for fifteen minutes between tests in order to achieve their baseline status again.
The three tests of the study were carried out during the months of April, May, June and July 2019.
The sample size was 30 participants with convenience sampling, who appeared in the absence of acute phase disease and/or not controlled, of legal age who had expressed their willingness to participate in the study. Exclusion criteria were people with acute phase disease, with musculoskeletal injuries of the upper extremities, people who had not reached the age of majority and people who had not signed the informed consent. Participants who were absent one or more days of the tests and those who voluntarily withdrew their consent to participate in the study were withdrawn.
Chest compressions were performed on a Resusci Anne QCPR® Simulation Mannequin with SimPad® control operating device from Laerdal Medical AS; The Roche Diagnostics Accutrend Plus device with BM-Lactate test strips was used to measure blood lactate; and for the subjective assessment of test hardness, the validated modified Borg CR-10 perceived effort scale (RPE) was used.
The data obtained in the SimPad® together with the rest of the data from the tests and from the participants were tabulated and exported to the statistical treatment program for analysis.
Statistical analysis was performed with the Statistical Package for the Social Sciences (SPSS) program. The description of the variables was made by counting the frequencies and their percentages and by their means and standard deviations (SD); as well as its median and interquatillic amplitude, depending on its normality. The Shapiro-Wilk test was performed to determine normality in the quantitative variables. The differences between the variables were established by the "chi-square" or by the "F" of Fisher, as well as "t" of Student or "U" of Mann Whitney; if more than two groups were compared, the ANOVA or Kruskal-Wallis test was used. In the search for association within related samples, the Student's t-test or the Wilcoxon test were used; if there were more than two, the statistic used was the Friedman test.
Pearson or Spearman was used for bivariate correlations. The level of significance was that of p <0.05.
RESULTS
The sample consisted of 30 participants, of which 26 were women (86.7%) and 4 men (13.3%). Tables 1 and 2define the characteristics of the individuals in the sample.
Table 1. Characteristics of the individuals in the sample - Categorical variables.

BMI = Body Mass Index
Table 2. Characteristics of the individuals in the sample - Quantitative variables.

SD = Standard derivation; IA = interquatillic amplitude.
Significant differences were found in the total number of external chest compressions performed during the test (p = 0.042), in the mean depth (p = 0.015), and in their mean frequency (p = 0.034) (Table 3). In all conditions, the variables behaved normally, except for the % of CPR in room temperature and cold temperature.
Table 3. Test results from the SIMPAD dummy - Quantitative variables.

% CPR = Correct Cardiopulmonary Resuscitation Percentage; Nº ECC = Total number of external chest compressions performed; Depth. med ECC = Average depth of external chest compressions; Frec. med ECC = Average frequency of external chest compressions; SD= Standard derivation; IA = interquatillic amplitude; Min. = Minimum; Max. = Minimum.
The mean scores obtained from the RPE by the participants in each of the three temperature tests were as follows: 4.4 ± 1.303 at room temperature, 4.97 ± 1.402 in heat and 4.87 ± 2.08 in cold ( p> 0.05). In hot and cold temperature, it was treated as a normal variable and in an environment as nonparametric.
Statistically significant differences (p<0.05) were found, regarding the variables obtained from the SIMPAD dummy, between the "average depth of chest compressions" in room temperature and heat temperature (50.53 mm vs 48.13 mm; p = 0.046), as well as at room temperature and cold temperature (50.53 mm vs 47.17 mm; p = 0.030) (Figure 1).
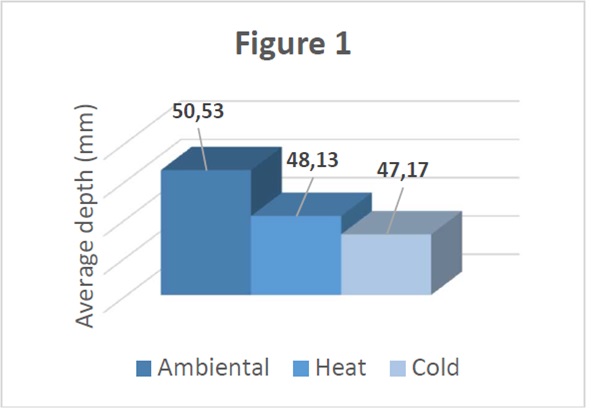
Figure 1. Average depth of chest compressions at different temperatures (22º, 40º and 0º) (p <0.05).
Also in relation to the “average frequency of external chest compressions” in ambient temperature and heat (110 cpm vs. 115 cpm; p = 0.025) and ambient temperature and cold (110 cpm vs. 116 cpm; p = 0.028) (Figure 2).

Figure 2. Average frequency of external chest compressions at different temperatures (22º, 40º and 0º) (p <0.05).
Differences in the “number of total compressions” between ambient temperature and heat (221 ecc vs. 229 ecc; p = 0.032); and ambient temperature and cold (221 ecc vs 231ecc; p = 0.046), was statistically significant (Figure 3).
DISCUSSION
For the discussion of the results, studies in the field of Physical Activity Sciences have been used, due to the difficulties in comparing it with other studies of the same approach. Thus, the authors want to highlight the difficulty of the discussion, so more studies would be necessary in this regard.
As a resolution of the main objective, in Table 3, it can be seen that in the variable "% CPR" there were no significant differences between the different conditions; however, if we look at the variables on which the CPR is based, frequency, depth and number of compressions, these significant differences did exist. In fact, among the parameters that include CPR, it is observed that, with respect to room temperature, the number of compressions increased both in hot and cold temperatures at the same time that the average depth decreased and these differences were significantly reflected. This can be explained by cardiac output, in which the increase in the former would compensate for the decrease in the latter, thus not being affected and maintaining the effectiveness of CPR 14.
In the same way, the sample in the conditions of ambient temperature and cold, performed advanced CPR, while the rest decreased the quality in the heat temperature. It could be explained by thermoregulating the body; in the hot condition, the body would need more time than the duration of the test to carry out the sweating and thus cool the body and maintain performance; while, in the cold condition, continuous muscle contraction would favor an increase in body temperature, and as observed in the results section, there is a direct correlation between the effectiveness of CPR and the increase in body temperature during test 15.
The perceived effort scale (RPE) offers us a subjective assessment of the rescuer on physical effort. In this study16, in which 2 minutes of CPR were performed, the mean value of the RPE was 3±2; therefore, it was lower than our results, however, the participants were a heterogeneous sample of health professionals trained in CPR. Likewise, significant differences were found regarding the increase of the intensity of the effort in heat temperature. As expressed in the article, in a fixed intensity activity performance is impaired, as exercise-induced hyperthermia is associated with central fatigue17. It is possible that under the recommendations of the European Resuscitation Council (ERC) to exchange the resuscitator every 2 minutes, in heat temperature this change could be carried out earlier, to guarantee the effectiveness of CPR18.
We consider that it would be necessary to carry out a comparative study that included a greater number of "n" and with a longer duration design, in which the resuscitators approached extreme fatigue and monitored the relevant variables over time, in order to obtain a more detailed evolutionary information.
Study limitations
Despite efforts to recreate the design of study, there were different technical limitations that could influence the research and have some impact on the results.
First, the tests were performed in a laboratory, not in a real setting, so it is not known if all aspects of a real resuscitation could be reproduced; there are variables in which the context can affect the rescuer; Motivation, environment, team, decision making can inherently affect the quality of a process. A second limitation could be found in the location of the test in cold temperature, since the space for performing the test was very limited, so the body dimensions of some participants might have affected the performance of external chest compressions.
CONCLUSIONS
In conclusion, the overall quality of external chest compressions has not shown statistically significant differences when performed in extreme heat or cold ambient temperatures Similarly, the median representing the percentage of chest compressions performed correctly in extreme heat was lower than that found in cold and ambient temperature. This shows a trend of worsening quality in that temperature condition compared to the other two despite not having found statistical significance. As for the RPE, it was similar in the three tests carried out; however, the extreme heat temperature seems to be the worst condition for performing chest compressions, qualitatively speaking, taking the ambient temperature at 22ºC as a reference.
Finally, statistically significant differences have been found in the parameters involved in chest compressions, the mean depth, the number of total compressions, and the mean frequency of chest compressions among the three temperature tests; however, they do not appear to have affected the overall quality result.
REFERENCES
1. Christenson J, Caen AR De, Bhanji F, Abella BS, Kleinman ME, Dana P, et al. Declaración de consenso de la AHA. 2014. [ Links ]
2. Kg M, Resuscitation E, Guidelines C. Recomanacions_ERC_2015_Principals_novetats.pdf. 2015;1-8. Disponible en: http://www.cercp.org/images/stories/recursos/Documentos/Recomanacions_ERC_2015_Principals_novetats.pdf [ Links ]
3. Blas G De, Garc P, Cobo-va C. Electrophysiology of Muscle Fatigue in Cardiopulmonary Resuscitation on Manikin Model. 2015;30-7. [ Links ]
4. Kleinman, ME, Brennan, EE, Goldberger, ZD, Swor, RA, Terry, M, Bobrow, BJ, Rea, T. (2015). Part 5: Adult Basic Life Support and Cardiopulmonary Resuscitation Quality. Circulation, 132(18 suppl 2), S414 -S435. doi:10.1161/cir.0000000000000259. [ Links ]
5. Sánchez B, Algarte R, Piacentini E, Trenado J, Romay E, Cerdà M, et al. Low compliance with the 2 minutes of uninterrupted chest compressions recommended in the 2010 International Resuscitation Guidelines . J Crit Care [Internet]. 2015;30(4):711-4. Disponible en: http://dx.doi.org/10.1016/j.jcrc.2015.03.001 [ Links ]
6. Gianotto-Oliveira R, Gianotto-Oliveira G, Gonzalez MM, Quilici AP, Andrade FP, Vianna CB, et al. Quality of continuous chest compressions performed for one or two minutes. Clinics. 2015;70(3):190-195. [ Links ]
7. Kiliç D, Göksu E, Kiliç T, Buyurgan CS. Resuscitation quality of rotating chest compression providers at one-minute vs. two-minute intervals: A mannequin study. Am J Emerg Med [Internet]. 2018;36(5):829-33. Disponible en: http://dx.doi.org/10.1016/j.ajem.2017.10.035 [ Links ]
8. López J, Almudena F. Fisiología del Ejercicio - López Chicharro.pdf. 2006. p. 987. [ Links ]
9. Carey MF, Stathis CG, Snow RJ, Febbraio MA, Hargreaves M. Influence of elevated muscle temperature on metabolism during intense, dynamic exercise. Am J Physiol Integr Comp Physiol. 2017;271(5):R1251-5. [ Links ]
10. Nybo L, Rasmussen P, Sawka MN. Performance in the Heat - Physiological Factors of Importance for Hyperthermia-Induced Fatigue. 2014;4(April):657-89. [ Links ]
11. Girard O, Brocherie F, Bishop DJ. Sprint performance under heat stress: A review. 2016;25:79-89. [ Links ]
12. Parkin JM, Carey MF, Zhao S, Febbraio MA. Effect of ambient temperature on human skeletal muscle metabolism during fatiguing submaximal exercise. J Appl Physiol. 2017;86(3):902-8. [ Links ]
13. Racinais S, Oksa J. Temperature and neuromuscular function. Scand J Med Sci Sport. 2010;20(SUPPL. 3):1-18. [ Links ]
14. H Wilmore J, L.Costill D. Control cardiovascular durante el ejercicio. En: H Wilmore, J; L Costill, D. Fisiología del esfuerzo y del ejercicio. 6ª ed. Barcelona: Editorial Paidotribo, 2007. P. 221-241. [ Links ]
15. Vogt J. Enciclopedia de Salud y Seguridad en el Trabajo. 4-5 p. [ Links ]
16. Trenado J, Quintana S, Baltasar S, Fern M, Mestre J. The physiological effect on rescuers of doing 2 min of uninterrupted chest compressions. res 2007;74:108-12. [ Links ]
17. Nybo L, Rasmussen P, Sawka MN. Performance in the Heat - Physiological Factors of Importance for Hyperthermia-Induced Fatigue. 2014;4 (April):657-89. [ Links ]
18. Mcdonald CH, Heggie J, Jones CM, Thorne CJ, Hulme J. Rescuer fatigue under the 2010 ERC guidelines, and its effect on cardiopulmonary resuscitation (CPR) performance. Joirnal Emerg Med 2012. [ Links ]
Received: December 11, 2019; Accepted: April 12, 2020











 texto en
texto en 



