My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Enfermería Global
On-line version ISSN 1695-6141
Enferm. glob. vol.19 n.60 Murcia Oct. 2020 Epub Dec 21, 2020
https://dx.doi.org/10.6018/eglobal.411831
Reviews
Checklist for a safe intra-hospital transport of critically ill patients: a scoping review
1MSc student in Medical-Surgical Nursing: Critical Patients, at the Institute of Health Sciences of Universidade Católica Portuguesa; Nurse at the Western Hospital Centre, Torres Vedras. Portugal. madalenacanellas@gmail.com
2MSc student in Medical-Surgical Nursing: Critical Patients, at the Institute of Health Sciences of Universidade Católica Portuguesa; Nurse at the Algarve University Hospital Centre, Faro Unit. Portugal.
3Ph.D., Assistant professor at the Institute of Health Sciences and integrated member of the Center for interdisciplinary health research of Universidade Católica Portuguesa. Portugal.
4Ph.D., Assistant professor at the Institute of Health Sciences of Universidade Católica Portuguesa. Portugal.
Transporting critically ill patients is has a set of risks that may jeopardize their safety. Knowing the risks associated with intrahospitalar transport of critically ill patients is essential to improving patient safety. For the sake of improving patient safety, was chosen to approach it as an intrahospitalar transport checklist, as the literature describes it as a practical and simple way to increase safety.
Objective:
Map available scientific evidence regarding aspects of a checklist that ensure the safety of critically ill patients in intrahospitalar transport.
Material and Method:
A scoping review was performed following the methodology proposed by The Joanna Briggs Institute in databases using the EBSCOhost and B-on search engines. Conducted research in Portuguese, English, and Spanish. Selected free full text articles, with no time limit. Inclusion criteria: adult/elderly critically ill patient, intrahospital transport, a checklist and patient safety.
Results:
Included 7 articles for analysis. Most verification requests that ensure the safety of critical patients on intrahospitalar transport concern the transport preparation phase, in which patient is monitored was the most mentioned aspect. From the post-transportation phase, checklist aspects are only available in 3 of 7 articles
Conclusion:
All studies address aspects that improve the safety of critically ill patients in intrahospitalar transport and are likely to be included in the checklist. There is no unanimity as to which aspects to include in the checklist.
Key words: intrahospital transport; checklist; critically ill; safety; adverse event; scoping review
INTRODUCTION
The intra-hospital transport (IHT) of critically ill patients is a common procedure. However, since it takes place within the hospital's facilities and under the supervision of healthcare professionals, it is often overlooked1. Despite being an ineviTable reality, it entails several risks that may jeopardize patient safety, not only because it is a transport, but also because critically ill patients are more susceptible to adverse events2. Such risks can create instability, with the consequent aggravation of the patients' clinical status. They may also lead to further complications, and the possibility of inadequate action during potential emergency situations3. The transport of critically ill patients produces a physiological impact which derives from movement, more specifically from acceleration, deceleration, and vibration. The simple act of moving a patient through the hospital's corridors and elevators may cause discomfort. But complications can also be caused by other aspects related to transport, including: patient repositioning; thermal variations of the surrounding environment, which may result in hypothermia; and noise, which may disturb, or generate anxiety in, the patient4. It is also important to note that a reduction in surveillance can occur during the execution of complementary diagnostic tests, since the patient may be less visible in such circumstances.
With respect to IHT, several authors have described high incidences of adverse events. In this regard, Farnoosh, Hossein-Nejad, Beigmohammadi, & Seyed-Hosseini-Davarani6 discovered that 33.3% of the patients were affected by adverse events during transport. Nevertheless, the occurrence of adverse events decreased to 10.8% after the implementation of transport protocols. Moreover, Jia & Gao7 reported that 79.8% of the analyzed critically ill patients experienced adverse events. In addition, Brunsveld-Reinders et al 8. observed, in their study, that the most frequent physiological adverse events (hypotension and hypoxia) were associated with malfunctioning equipment and deficient transport preparation. Concerning Portugal, the Portuguese Medical Association and the Portuguese Society of Intensive Care3 have identified the following most frequent incidents: endotracheal extubation, exteriorization of venous accesses, inadequate oxygen supply, failure of transport ventilators, accidental exteriorization or clamping of thoracic drains, and lack of battery in the necessary equipments. It is also important to note that, many times, these adverse events are only detected at the destination service, and not when they actually occur (during transportation)9.
Understanding the risks associated with the IHT of critically ill patients is essential to improve the safety of the latter. By training and perfecting the performance of all the professionals involved in the IHT, as well as by standardizing the monitoring equipment and the conducted actions, it is possible to avoid and/or minimize the occurrence of adverse events, to achieve excellence in care provision, and to increase patient safety.10 Furthermore, Hales & Pronovost11 report that error reduction is directly linked to improvements, not only in the patients clinical outcome, but also in the effectiveness of resource utilization.
With the purpose of enhancing patient safety, the Ministry of Health - through “Plano Nacional para a Segurança dos Doentes 2015-2020” (“National Plan for Patient Safety 2015-2020”, in free translation) - established several strategic objectives, which included “increasing the safety culture of the internal environment” and “increasing the safety of communication”. Moreover, it stressed that “improving patient safety is a team responsibility, which mobilizes the individual skills of each team member and implies the systemic management of all activities”.12 The Nurse is, thus, responsible for developing strategies to improve the patients' safety within the hospital environment. This justifies the study of the IHT checklist, since the available literature describes it as a practical and simple way of promoting patient safety during that critical procedure11.
According to the guidelines provided by the Intensive Care Society and the Faculty of Intensive Care Medicine13, checklists should be used during transfers, to ensure that, for each stage of the process, all the necessary preparations are executed. This is applicable to the transfer of any critically ill patient, regardless of it being intra-hospital or inter-hospital, since the level of preparation, supervision, and care, is always the same. Although the Australian and New Zealand College of Anaesthetists14, as well as the Intensive Care Society and the Faculty of Intensive Care Medicine13, mention identical principles for intra- and inter-hospital transport, a decision was made to direct this review towards checklists specifically developed for the intra-hospital transport of critically ill patients.
A critically ill patient is a person who has “his/her life threatened by the failure, or theimminent failure, of one or more vital functions, and whose survival depends on advanced means of surveillance, monitoring and treatment”15. Usually, the IHT of critically ill patients is carried out between emergency rooms, intensive care units (ICUs), imaging units, and operating rooms. It is conducted for diagnostic, therapeutic, or relocating, purposes, involving different sections of the same institution. Besides being frequent, the IHT is also ineviTable, particularly when the patients are in emergency services.9,16 Considering the inherent peril of moving critically ill patients, it is crucial to reflect carefully about the possible execution of auxiliary diagnostic tests, so as to ponder the risks and benefits of such procedures3,8. For the duration of the IHT, the levels of care, surveillance, and intervention, should be equal to, or higher than, those observed in the service of origin3. However, in order to increase the patients' safety during transport, it is important to assure their previous assessment and stabilization14. In this regard, the first 5 minutes of transport, the patients' transfer, and a prolonged transport (more than 30 minutes long), have been identified as the most dangerous situations, with respect to the occurrence of accidents3.
The IHT team must include, at least, one nurse and one doctor, with the specific skills and training required to perform this type of transport8,14. In his study, Papson17 discovered that the incidence of adverse events was inversely proportional to the professionals' experience level, when junior and senior doctors were compared.
Patient safety is defined as the reduction, to an accepTable minimum, of the risk of avoidable harm, during care provision18. The concept of “accepTable minimum” refers to a collective notion, taking into account the current level of knowledge, the available resources, and the context in which the care was provided. The aforesaid aspects are balanced with the risk of not being treated at all, or being subjected to an alternative treatment18,19. These patients' vulnerability makes them prone to safety incidents, which can result in harmless events, or harmful (adverse) events18.
All human actions are prone to error. The main difficulties faced by healthcare professionals are associated with the unreliability of their memory and attention. In addition, there is the possibility of failure when dealing with stress, fatigue, interruptions, new situations, and the pressure to comply, especially with regard to routine issues. While under pressure, due to more urgent matters, a healthcare professional can easily overlook routine issues, and may end up skipping a few steps of the process, which leads to errors20. The checklists' structure and predictability can help to circumvent such limitations, by facilitating and systematizing the provision of care. In its turn, this reduces variability and enhances performance, thus allowing an improvement of the provided care (in terms of quality), as well as a decrease in health-related costs21. The use of checklists also permits to standardize actions, to provide evidence-based care, to improve communication, to use the available equipment in an appropriate way, to minimize errors, and to mitigate the human memory's fallibility(10,21. Williams et al.22 demonstrated that the employment of a transport checklist increased the compliance with the existing guidelines. Hence, checklists enable the creation of a more efficient and effective knowledge, by incorporating empirical and tacit evidence, continuously updated by healthcare professionals, and by converting that evidence into explicit behaviors21
Since IHT is unavoidable, while providing care to critically ill patients, checklists become a particularly helpful tool for healthcare professionals, by allowing an increase of the IHT's safety, in a practical manner11.
Given all this, the authors considered pertinent to conduct a scoping review on the topic, since none was found in the literature, and because the available scientific evidence with regard to the various aspects of a checklist that are capable of ensuring the safety of critically ill patients during IHT is quite scattered. Furthermore, in order to fulfill the objective of the present work, the following research question was defined: “Which aspects of a checklist ensure the safety of critically ill patients during intra-hospital transport?”
MATERIAL AND METHOD
This work is a scoping review, which follows the methodology proposed in “The Joanna Briggs Institute Reviewers' Manual 2015: Methodology for JBI Scoping Review”23, and aims to explore the available scientific evidence with regard to the aspects of a checklist that ensure the critically ill patients' safety during IHT.
Several inclusion criteria were defined, resorting to the “Population, Context and Concept” strategy:
the “Population” comprised critically ill adult/elderly patients; the pediatric population was excluded, because it has very specific characteristics that imply special care during transport;
the “Concept” was patient safety achieved through the use of a checklist;
the “Context” was intra-hospital transport; the articles referring to inter-hospital transport were not considered.
The bibliographical search was conducted in Portuguese, English and Spanish, and only full-text articles available without charge were selected. The search was not limited to a specific time span, in order to encompass as much works as possible. The search strategy was carried out in two stages: firstly, a comprehensive search was employed to address the topic and define the research question; secondly, another search was conducted, using Boolean operators and the descriptors/keywords chosen in the included databases.
The search was performed in July, 2019, using the search engines available at the EBSCOhost and B-on platforms. The following “MeSH” (Medical Subject Headings) descriptors were applied: “Critical Care”, “Checklist”, “Protocol”, “Critical Patient” and “Safety”. The following keywords were employed to direct the search: “Transport”, “Intra-Hospital Transport” and “Emergency Department”. The following combinations of terms and Boolean operators were used during the search:
- Transport OR Intra-hospital Transport (Title) AND Protocol OR Checklist (Title) AND Critical Patient OR Critical Care OR Emergency Department (Text) NOT Pediatric;
- Checklist (Abstract) AND Intra-hospital Transport OR Intra-hospital Transport (Abstract);
- Checklist (Abstract) AND Intra-hospital Transport OR Transport (Title) AND Safety (Text).
Taking into account the inclusion criteria, the articles were initially selected based on their title. Afterward, the selection was made through the abstract and, finally, through the article's full reading. This process is shown in Image 1.

Image 1: PRISMA flowchart adapted from the one presented in “The Joanna Briggs Institute Reviewers' Manual 2015: Methodology for JBI Scoping Review”23
Initially, a total of 133 articles were found through the database search. Of these, 12 were duplicates and were, therefore, removed. The remaining 121 works were subjected to title analysis, which resulted in the selection of 18 articles for abstract analysis. The later step allowed identifying a total of 12 articles eligible for full text reading, of which 7 ended up being included in this scoping review.
In this procedure, the authors considered primary studies of quantitative and/or qualitative nature, as well as literature reviews. The search, selection and analysis process was performed by two independent evaluators. A third evaluator was consulted whenever divergences occurred. The obtained data was organized using the Table presented in the next section.
RESULTS
The following Table (Table 1) summarizes the obtained results for each included study.
Table 1: Summary of the obtained results.
| Study's identification (title and date) | Study type and number of participants | Objective | Safety ensuring aspects of the checklist regarding IHT |
| S1: A before- and after-intervention trial for reducing unexpected events during the intrahospital transport of emergency patients9 2011 | Experimental, non-randomized study. In the pre-intervention period, 597 patients were included and 680 transport events were observed. During the post-intervention period, 539 patients were included and 605 transport events were observed. | To explore the intervention's effect - i.e., the outcome of implementing a checklist protocol for a safe intra-hospital transport - on the incidence of adverse events during the transport of emergency patients. | Based on previous studies, conducted in ICUs and trauma centers, the authors considered 28 items to be included in safe transport checklists: - 2 general items (a bracelet with an identification number, and an informed consent); - 8 equipment-related items (oxygen supply, 3-lead electrocardiographic monitor, non-invasive blood pressure monitor, patient monitor, and infusion pump); - 7 items related to the patient's clinical status (blood pressure, oxygen saturation, respiratory rate, and mental state); - 8 items related to tubes and lines (endotracheal tube, peripheral/central venous catheters, and drainage tubes); - 3 stretcher-related items (rail position and the presence of attached equipment). The authors also recommend: filling out checklists on the elements that the transport team should include; contacting the responsible physician, before transferring the patient. |
| S2: Transporte intra-hospitalar dos clientes críticos: revisão sistematizada da literatura para um protocolo clínico24 2016 | Systematic literature review, with 20 included articles. | To investigate the scientific research efforts which analyze the in-hospital care provided to critically ill clients. | The authors highlight the following aspects: - to anticipate, and minimize, possible adverse events associated with transport; - to continuously monitor the patient (electrocardiogram, peripheral oxygen saturation and non-invasive blood pressure). In certain patients, it may be necessary to monitor the invasive blood pressure and the central venous pressure. In patients under mechanical ventilation, the monitoring of ventilation parameters and patient position is recommended. |
| S3: Checklist para o transporte intra-hospitalar de pacientes Internados na unidade de terapia intensiva 25 2015 | Work divided into: i) Descriptive, quantitative study. A total of 103 transports were followed, resulting in the inclusion of 70 patients and 100 professionals. ii) Integrative literature review, comprising 5 articles. | To elaborate a patient assessment checklist for the intra-hospital transport of ICU patients, at a hospital located in the region of Triângulo Mineiro. | The authors emphasize the following aspects: - to verify the patient's identification; - to conduct a pre-IHT evaluation (encompassing the respiratory, circulatory, neurological, metabolic, digestive, and genito-urinary systems, as well as the equipment, and the vasoactive and sedative therapeutics); - to perform an assessment during the IHT (covering the patient's clinical conditions, in addition to the therapeutics and devices/equipment); - to carry out a post-IHT evaluation (including the patient's clinical conditions, in addition to the therapeutics, devices/equipment, and transport record). |
| S4: A comprehensive method to develop a checklist to increase safety of intra-hospital transport of critically ill patients8 2015 | Three complementary methods were applied in a sequential manner: i) a literature review on IHT guidelines and checklists (11 guidelines and 5 checklists were included); ii) the analysis of IHT-related incidents, at the Leiden University Medical Center (118 IHT-related incidents were examined); iii) the performance of structured interviews with 10 doctors and 15 nurses, who worked at an ICU, in order to list possible issues associated with IHT and identify methods to avoid their accumulation. | To elaborate a checklist covering the preparation (pre-IHT) stage, the transport stage, and the re-installation (post-IHT) stage, to improve the safety of critically ill adult patients during IHT, in an ICU context. | The literature review draws attention to the following aspects: - the existence of a clear communication with the destination service, involving the confirmation of its readiness; - the patient's monitoring during IHT, as well as during the diagnostic/therapeutic procedures The incidents' analysis stresses the following aspects: - regularly checking and recording the patient's vital signs (at least every 15 minutes); - managing medication and fluids, in order to maintain the patient's physiological stability; - when returning to the home service, after the patient's reinstallation and stabilization, the monitoring procedures and the medication should be evaluated, and the transport route should be recorded; - cleaning all transport equipment and reconnecting it to the main power supply, in order to recharge its batteries. The interviews' results highlight the following aspects, to be considered before transport: - ensuring larger extensions of intravenous lines, when performing diagnostic procedures such as magnetic resonance imaging; - checking and calculating the amount of oxygen available in the cylinder; - checking the presence of a defibrillator; - checking all transport equipment; - checking if the batteries are fully charged; - confirming the appointment with the destination service; - checking and preparing the intravenous medication; - checking the availability of extra medication and additional intravenous fluids. |
| S5: Safety First! Using a Checklist for Intrafacility Transport of Adult Intensive Care Patients26 2015 | Mixed study, including 2506 transports. | To develop a transport checklist that is easy to use and effective in preparing patients for transport. | The authors emphasize the following aspects: - obtaining a manual inflator with face mask and PEEP valve; - confirming that the oxygen cylinder is full; - obtaining a disposable capnography device; - configuring and testing the transport ventilator, to assess the patient's tolerance and stability; - ensuring that the transport monitor is connected and charged; - assessing the patient's vital signs; - evaluating the need for medical follow-up, using another checklist. |
| S6: Transporte intra-hospitalar de pacientes adultos em estado crítico: complicações relacionadas à equipe, equipamentos e fatores fisiológicos10 2012 | Integrative literature review, which included 20 articles. | To identify, in the available literature, the complications associated with the patient's physiological alterations, the equipment, the members of the multi-disciplinary team, and the communication between teams, during the transport of critically ill patients in an intra-hospital environment. | The authors draw attention to the following aspects: - using safety identification criteria, such as the resources needed for each patient during transport; - checking the patient's identification; - ensuring a standardized data transmission between the original location, the transport team and the destination; - ensuring care provision during the entire transport and also while the patient is out of his/her original location; - checking the technical conditions of the equipment to be used in the transport. - checking the equipment's batteries. |
| S7: A checklist for intrahospital transport of critically ill patients improves compliance with transportation safety guidelines22 2019 | Prospective pre- and post-intervention study, with a total sample of 76 transports (38 before the intervention, and 38 after). | To compare the compliance with the interdisciplinary guidelines, before and after the introduction of a transport checklist, in a tertiary metropolitan ICU. | The authors stress the following aspects: - checking the patient's identification; - notifying the destination service; - ensuring that the porter is present; - knowing the patient's Cormack-Lehane grade before the departure; - ensuring the presence of the following equipment, devices and materials: . defibrillator; . emergency equipment bag; . two oxygen cylinders, both 3 quarters full; . manual inflator with a reservoir; . secretion aspirator; . extra medication as needed; . monitor with battery at least 3 quarters charged; . extra-venous access; - transferring data to the team, after returning to the service of origin; - registering the transport after its completion. |
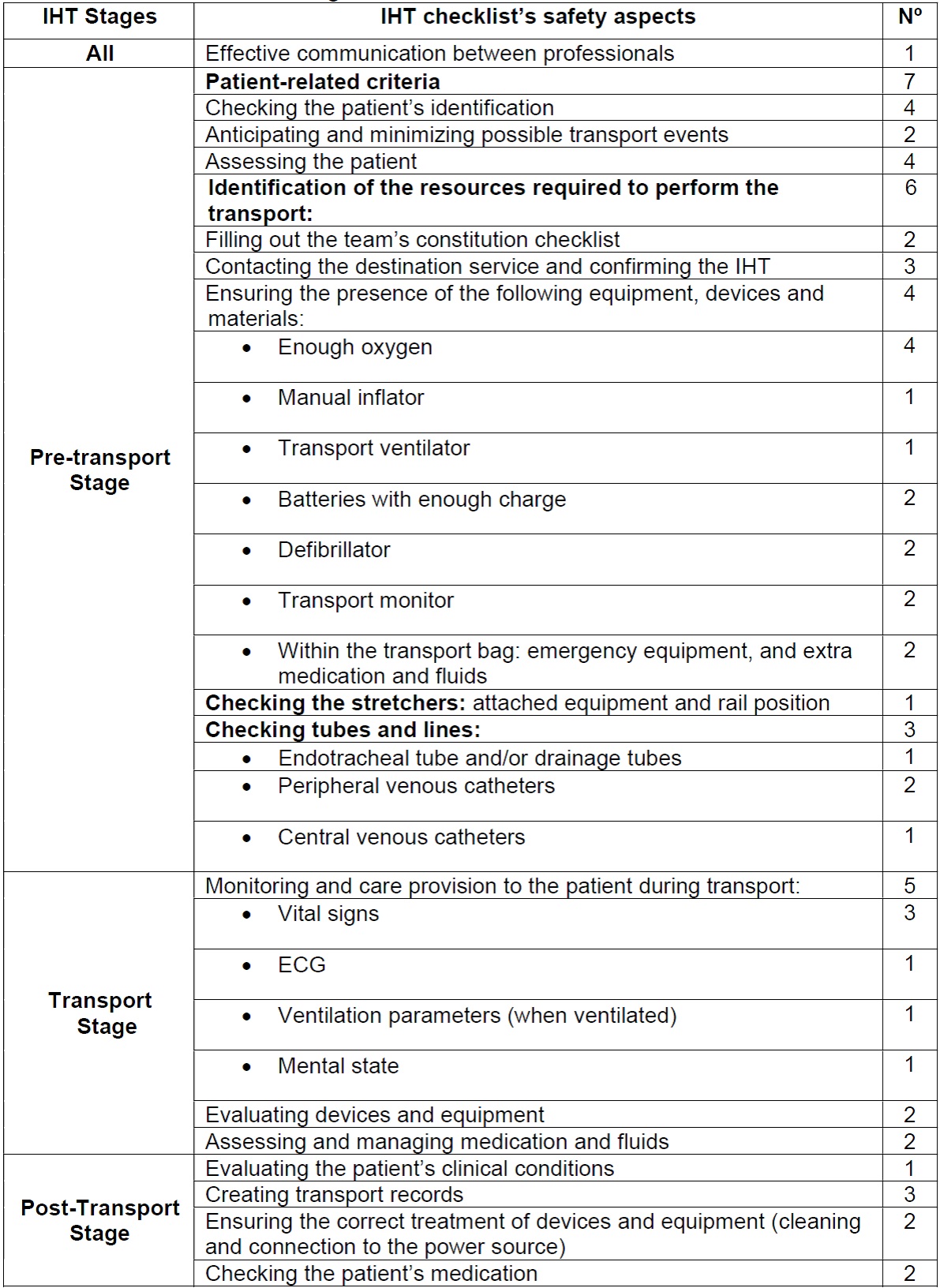
The most relevant findings, with regard to the IHT checklist's safety aspects, were organized according to the different IHT stages mentioned by Brunsveld-Reinders et al.8, resulting in the elaboration of Table 2. The number of references concerning each aspect is shown in the right column of the aforesaid Table.
DISCUSSION
Although small in number, the works included in this review produced a set of findings which is consistent with the proposed framework. Furthermore, its interdisciplinary character and transversality regarding the various contexts makes it representative of the theme under study.
Patient safety during IHT has been optimized by the development of adequate equipment, trained teams and specific protocols10 The transport's success depends directly on the planning, on the equipment's adequacy and on the multidisciplinary team's organized performance27. Brunsveld-Reinders et al8 reported an incidence of 38% for pre-transport incidents, 47% for transport incidents and 15% for post-transport incidents. Nonetheless, they mention that the pre-transport stage is the most extensively addressed in the literature. They also refer that the pre-transport stage, in which the transport's planning takes place, is the most studied by the different authors, listing several aspects that should be verified to ensure safety.
The effective communication between professionals is a crucial and transversal aspect that influences all transport stages, since professionals from multiple services are involved in the process. The “Plano Nacional para a Segurança dos Doentes 2015-2020”12 (“National Plan for Patient Safety 2015-2020”, in free translation) establishes the need to “increase the communication's effectiveness” as its second strategic objective. With respect to communication, the most frequently mentioned aspect in the articles under review was the prior contact with the destination service8,22,26, since it allows the preparation of the necessary resources, the verification of the destination's availability and the reduction of the receivers' anxiety27. By ensuring the communication with the destination service, the checklist is, on its own, a vector for communication improvement22. The Joint Commission National Patient Safety Goals19 recommends that hospitals should develop protocols to improve data flow between the various sites involved in the patients' transport, as a means of improving the patients' safety and satisfaction, an aspect highlighted by De Almeida et al.10. The presence of communication barriers is one of the major obstacles identified by nursing teams8,29. In this context, Brunsveld-Reinders et al 8 suggest the creation of a debriefing moment, gathering the ICU doctors and nurses, after the transport.
In the study by Choi et al.9, approximately one quarter of the adverse events detected during IHT were associated with equipment-related incidents, which explains the importance attributed, in all the included studies, to the equipment's acquirement/verification.9,22,25 The aforesaid studies list several specific aspects to be taken into account. From these, the most frequently mentioned is the verification of the amount of oxygen available for transport8,9,22,26 Therefore, it is extremely important to check the technical conditions of the equipment to be used. In this regard, Ribeiro et al.2 propose the equipment's daily verification by nurses. Another frequently mentioned aspect is the need to check the batteries' charge8,10.
Notwithstanding, not all authors mention equipment-related problems as the most frequent ones29. Ong & Coiera29 point to an equipment failure incidence of only 0.2%, attributing a greater relevance to other aspects, such as team composition (43.1%) and patient identification (41.9%). Patient identification is mentioned in 4 of the 7 included articles9,10,22,25, corresponding to the fifth strategic objective of the “Plano Nacional para a Segurança dos Doentes 2015-2020”12. The application of a checklist to determine the team's constitution is referred to in some studies9,26. De Almeida et al.10 defend that the nurse's presence during transport is fundamental, since it reduces the incidence of adverse events. This happens because those events are less triggered and detected earlier, when compared to the medical team's exclusive intervention. The presence of more experienced physicians is also associated with a lower incidence of adverse events17.
In the transport stage, the objective is to maintain the patient's physiological stability, through continuous monitoring, to avoid iatrogenic occurrences30, which is why patient monitoring was the most mentioned aspect.8,9,10,24,25 During transport, the levels of care, surveillance and intervention should be equal to, or greater than, the ones verified at the service of origin.3 However, to increase the transport's safety, it is important to previously evaluate and optimize the patient's clinical status14.
After the instability manifested by the critically ill patient during transport, the stabilization process may be slow. Even when the patient presents hemodynamic stability during the transport stage, he/she may undergo hemodynamic changes in the destination service, after the conclusion of the transport procedure30. This determines the need for additional stabilization after IHT. Nevertheless, only 3 of the 7 included articles8,22,25 mentioned aspects to be verified in this stage.
Several authors have considered patient safety during IHT as a product of the combination of various factors, such as the implementation of continuous educational actions and the utilization of protocols. This promotes improvements in: guideline compliance; transport standardization; communication; equipment monitoring; and ability to identify and resolve possible intercurrences2,10,29 Raizer & Cruz24 suggest that, when following a protocol, the professionals who perform the transport are more capable and autonomous to make quick decisions that ensure patient safety.
Thus, the use of checklists has proven to be an effective measure2,22,25 Nurses frequently play an important role in the implementation of checklists22. Nonetheless, in healthcare, there are barriers that hinder checklist use, related to operational and cultural circumstances11.
Since the objective of minimizing IHT-related risks has not been achieved, there is a need for a better IHT planning, with a greater attention to technical and human conditions.10 In order to promote the successful implementation of checklists, it is important that they: are easy to apply, do not duplicate the nurses' work26, are adapted to local procedures and policies8, and are understood by the nurses before their use9.
The limitations of this study are related to the articles' selection process, which only considered works written in Portuguese, English and Spanish, thus running the risk of not including relevant studies published in other languages. Since this is a scoping review, the methodological evaluation of the included studies has not been carried out and it is not possible to transfer directly the contents to the professional practice.
We, therefore, suggest the development of primary research in the field of patient safety during IHT, and within the context of the Portuguese reality, particularly concerning the application of an IHT checklist.
CONCLUSIONS
Understanding the risks associated with the IHT of critically ill patients is essential to improve its safety. Hence the need to identify the checklist aspects capable of ensuring that safety, in order to attain a more accurate knowledge on the subject. All the included studies address aspects which can be integrated in a checklist, to improve the critically ill patients' safety during IHT. The authors are unanimous on the need to take measures to ensure IHT safety, but there is no consensus regarding the items to be checked. In this review, we found that none of the considered aspects was mentioned in all the included articles.
Not all authors divide the IHT into 3 stages, but they all address aspects related to those phases. Since there are published guidelines for IHT, a greater uniformity would be expected in practice. In this regard, the checklist can be a powerful tool, because it increases guideline compliance, creating, in a simple manner, a more efficient, effective and practical knowledge.
The continuous training of the professionals involved in the transport, the standardization of actions, guideline compliance, the adequacy and correct functioning of the equipment, and the critically ill patients' clinical monitoring during transport, are decisive to the prevention/minimization of adverse events. Only considering these aspects it will be possible to achieve excellence in care provision and patient safety, with the nurse taking on a crucial responsibility, as part of the transport teAm
REFERENCES
1. Morais SA, Almeida LF. Por uma rotina no transporte intra-hospitalar: elementos fundamentais para a segurança do paciente crítico. Revista Hospitalar Universidade Pedro Ernesto. 2013;12(3):138-146. [ Links ]
2. Ribeiro G da SR, Silva RC da, Ferreira M de A. Tecnologias na terapia intensiva: causas dos eventos adversos e implicações para a Enfermagem . Revista Brasileira de Enfermagem. 2016 ;69(5):972-980. [ Links ]
3. Ordem dos Médicos (Comissão da Competência em Emergência Médica) e Sociedade Portuguesa de Cuidados Intensivos. Transporte de Doentes Críticos. 2008; 1-30. [ Links ]
4. Fanara B, Manzon C, Barbot O, Desmettre T, Capellier G. Recommendations for the intra-hospital transport of critically ill patients. Critical Care. 2010;14(3), R87. [ Links ]
5. Ott LK, Hoffman LA, Hravnak M. Intrahospital transport to the radiology department: Risk for adverse events, nursing surveillance, utilization of a MET, and practice implications. Journal of Radiology Nursing. 2011;30(2):49-54. [ Links ]
6. Farnoosh L, Hossein-Nejad H, Beigmohammadi M-T, Seyed-Hosseini-Davarani S-H. Preparation and Implementation of Intrahospital Transfer Protocol for Emergency Department Patients to Decrease Unexpected Events. Advanced Journalof Emergency Medicine. 2018;2(3):e29. [ Links ]
7. Jia L, Wang H, Gao Y, Liu H, Yu K. High incidence of adverse events during intra-hospital transport of critically ill patients and new related risk factors: A prospective, multicenter study in China. Critical Care. 2016;20(1):1-13. [ Links ]
8. Brunsveld-Reinders AH, Arbous MS, Kuiper SG, Jonge E. A comprehensive method to develop a checklist to increase safety of intra-hospital transport of critically ill patients. Critical Care. 2015;19(1), 214. [ Links ]
9. Choi HK, Shin S Do, Ro YS, Kim DK, Shin SH, Kwak YH. A before- and after-intervention trial for reducing unexpected events during the intrahospital transport of emergency patients. The American Journal Emergency Medicine. 2011;30(8):1433-1440. [ Links ]
10. De Almeida ACG, Neves ALD, De Souza CLB, Garcia JH, De Lima LJ, De Barros ALBL. Transporte intra-hospitalar de pacientes adultos em estado crítico: complicações relacionadas à equipe, equipamentos e fatores fisiológicos. Acta Paulista de Enfermagem. 2012;25(3):471-476. [ Links ]
11. Hales BM, Pronovost PJ The checklist-a tool for error management and performance improvement. Journal Critical Care. 2006;21(3):231-5 [ Links ]
12. Ministério da Saúde. Plano Nacional para a Segurança dos doentes 2015-2020. Diário da República. 2015;2(2). [ Links ]
13. Intensive Care Society & Faculty of Intensive Care Medicine. Guidance On: The Transfer Of The Critically Ill Adult. 2019;1-40. [ Links ]
14. College of Intensive Care Medicine of Australia and New Zealand, Emergency Medicine, A. C. F., & Anaesthetists A. Guidelines for Transport of Critically ill Patients. Emergency Medicine. 2015; 1-12. [ Links ]
15. Ordem dos Enfermeiros. Regulamento de Competências Específicas do Enfermeiro. 2018;19359-19370. [ Links ]
16. Dunn MJG, Gwinnutt CL, Gray AJ Critical care in the emergency department: Patient transfer. Emerg Med J 2007;24(1):40-44. [ Links ]
17. Papson JPN, Russell KL, Taylor DMD. Unexpected Events during the Intrahospital Transport of Critically Ill Patients. Acad Emerg Med 2007;14(6):574-577. [ Links ]
18. Direçao Geral de Saúde. Estrutura Concetual da Classificação Internacional sobre Segurança do Doente. Relatório técnico Final. 2011;142. [ Links ]
19. Joint Commission. National Patient Safety Goals 2019. 2019;1. [ Links ]
20. Gawande A. The Checklist Manifesto: How to get things right. First Edit. York New York: Metropolitan Books. 2010. ISBN: 978-0-8050-9174-8. [ Links ]
21. Winters BD, Gurses AP, Lehmann H, Sexton JB, Rampersad CJ, Pronovost PJ Clinical review: Checklists - translating evidence into practice. Crit Care. 2009;13(6):1-9. [ Links ]
22. Williams P, Karuppiah S, Greentree K, Darvall J A checklist for intrahospital transport of critically ill patients improves compliance with transportation safety guidelines. Australian Critical Care. 2019;2-6. [ Links ]
23. The Joanna Briggs Institute. Joanna Briggs Institute Reviewers' Manual: 2015 edition/Supplement. South Australia: The Joanna Briggs Institute; 2015. [ Links ]
24. Raizer CN, Cruz ICF da. Transporte intra-hospitalar dos clientes criticos: revisao sistematizada da literatura para um protocolo clinico. Journal of Specialized Nursing Care. 2016;8,No 1. [ Links ]
25. Silva R da, Amante LN. Checklist for the intrahospital transport of patients admitted to the Intensive Care Unit. Text Context Nursing 2015;24(2):539-547. [ Links ]
26. Comeau OY, Armendariz-Batiste J, Woodby SA. Safety first! using a checklist for intrafacility transport of adult intensive care patients. Critical Care Nurse. 2015;35(5):16-25. [ Links ]
27. Beckmann U, Gillies DM, Berenholtz SM, Wu AW, Pronovost P. Incidents relating to the intra-hospital transfer of critically ill patients: An analysis of the reports submitted to the Australian Incident Monitoring Study in Intensive Care. Intensive Care Medicine. 2004;30(8):1579-1585. [ Links ]
28. Bergman LM, Pettersson ME, Chaboyer WP, Carlström ED, Ringdal ML. Safety hazards during intrahospital transport: A prospective observational study. Critical Care Medicine. 2017;45(10):e1043-1049. [ Links ]
29. Ong MS, Coiera E. Safety through redundancy: A case study of in-hospital patient transfers. Qual Saf Health Care. 2010;19(5):1-8. [ Links ]
30. Júnior GAP., Carvalho JB de, Filho, Ponte AD, Malzone, DA, Pedersoli CE. Transporte Intra-Hospitalar do Paciente Crítico. Simpósio de Cirurgia de Urgência e Trauma. 2007;2a Parte C(4):500-508. [ Links ]
Received: January 28, 2020; Accepted: March 22, 2020











 text in
text in