Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Enfermería Global
versión On-line ISSN 1695-6141
Enferm. glob. vol.20 no.61 Murcia ene. 2021 Epub 01-Feb-2021
https://dx.doi.org/10.6018/eglobal.417281
Originals
Obstetric factors associated with birth of moderate and late premature babies
1 Nurse. Federal University of Santa Maria, Adjunct Professor of Health Sciences Department. Palmeira das Missões/RS, Brazil. leo_jantsch@hotmail.com
2Physician. Graduated from Federal University of Santa Maria, Medicine Course. Santa Maria, RS, Brazil.
3Physician. Federal University of Santa Maria, Graduated Student in Medical Clinic at Universitary Hospital of Santa Maria. Santa Maria, RS, Brazil.
4Undergraduated student at Medicine Course at Federal University of Santa Maria. Santa Maria, RS, Brazil.
5Nurse. Federal University of Santa Maria, Associated Professor of Nursing Department. Santa Maria, RS, Brazil.
Objective:
To analyze obstetric variables associated with the birth of moderate and late premature babies in a city in the southern region of Brazil.
Method:
Cross-sectional study that analyzed the obstetric variables of 151 moderate and late preterm infants from May 2016 to May 2017 resident in Santa Maria/RS. Data were collected by means of their own instrument daily, and subsequently analyzed descriptively and by comparison of frequency and correlation.
Results:
Twinning (14.6%) was the most frequent feature among late twins when compared to the moderate group (p = 0.019). The other factors showed no significant difference. The higher number of previous premature births has a significant correlation with the lower gestational age at birth (CI = -0.522, p = 0.008).
Conclusion:
For the two groups of premature infants studied, the reasons did not present significant difference, which suggests homogeneity regarding the obstetric reasons for early birth.
Key words: Obstetric Labor, Premature; Infant, Premature; Risk Factors; Gestational Age; Neonatal Nursing
INTRODUCTION
It is estimated that, annually, 15 million premature babies are born1, and Brazil occupies 9th place in absolute number of premature births, which configures a public health problem2. The World Health Organization (WHO) defines as premature neonates those born before completing 37 weeks of pregnancy. Based in gestational age, these newborns can be further subcategorized in extremely preterm infants (<28 weeks), very preterm (28-<32 weeks) and moderate to late premature babies (32-<37 completed weeks of gestation)1.
In respect to the techno scientific development of the last decades, mainly in reference to the utilization of protocols for the inhibition premature labor and the tocolytic agents use, prematurity is still the main cause of morbidity and mortality in the neonatal period. A recent study reaffirms that complications related to preterm birth lead the global ranking of death in children under 5 years old, making a total of 1.055 million deaths in 20153.
The newborn (NB) gestational age (GA) is considered a physiological determinant for extrauterine adaptation and for this is an important marking for the neonate's prognosis, mainly in the early neonatal period. Considering fetal maturity complete at 34 weeks of gestational age, puts the NB in a situation of imposition to extrauterine adaptation that presents risks to health and possibility of death4.
The maintenance of the high premature birth rates over the last few years instigates the necessary discussion about the survival characteristics of these children, besides recognizing the immediate and late health demands that elapse from a premature birth. Regarding clinical/somatic morbidities, study highlights they exist in an isolated form being the prevalence of morbidities that affect with higher risk moderate and late premature babies, the hyperbilirubinemia and the complications such as low weight gain. According to this author, there is high incidence of late premature baby readmissions in the first month of life, considering that they are discharged from the service early and with full-term NB routines, as they are considered “almost” at term4.
Several maternal-based diseases were related to preterm labor, such as maternal hypertension, utero-placental alterations, infectious diseases and heart diseases5. The main obstetric complications associated to an increased risk of these labors involve the premature rupture of the membranes, pregnancy-specific hypertensive disease, oligohydramnio and urinary tract infections6,7.
Studies indicate that gestational complications, especially in the third trimester, are related to late and moderate premature delivery as well as prenatal care, regarding the number and quality of consultations, are directly related to the reduction in the number of premature births. Late prenatal care indicates greater predisposition, not only to premature delivery but also to low birth weight and to the development of neonatal vulnerabilities 8,9.
Thus, it is understood that moderate and late preterms have clinical vulnerability. Therefore the recognition of obstetric factors, associated with premature birth, should be used in the development of preventive practices during prenatal care. This study aimed to analyze obstetric variables associated with the birth of moderate and late premature babies in a city in the southern region of Brazil.
METHOD
This is a cross-sectional study carried out in the obstetric ward of a university hospital in Southern Brazil. This hospital is reference for high risk pregnancy for the midwest region of Rio Grande do Sul. The sector has 15 beds and reaches maximum capacity daily. Participated in the study all newborns with a gestational age between 32 and 36 weeks and 6 days of pregnancy, defined be the Capurro of evaluation in the first hours of life, that were born in these hospital and that resided in the county of Santa Maria/RS in the moment of hospital discharge. Gestational age was analyzed under categorization: Moderate - 32 weeks to 33 and 6 days - and late 34 to 36 plus 6 days10.
The period of data collection was from May 2016 to May 2017, making a total of one year of data collection and the inclusion of 151 participants in the study. Thus, daily visits were made to the field of study, by research assistants previously trained for such, to the end of minimizing selection losses.
To collect the data a proper instrument was used, built for this end, which contained the obstetric variables collected in the medical record of the parturient and the baby (pregnancies [numeric variable]; previous abortion [numeric variable]; maternal age[numeric variable]; risk pregnancy [defined in the medical record] or not [categorical variable]; reason for risk pregnancy (when applicable) [categorical variable]; Prenatal [variable category]; reason premature birth) [variable category]).
The instrument was established having as basis the definition from the Brazilian State Health Departments11. It is highlighted that for the variables: reason for risk pregnancy and reason for premature birth, the information was collected according to what is established in the medical record of the parturient.
As for the prenatal variable, it was considered adequate/not adequate, by means of the number of consultation realized and registered in the patient's medical record. The evaluation happened as recommended by the Brazilian State Health Departments [minimum six consultations until end of pregnancy, monthly consultation until 28th week of gestational age and biweekly until the 36th week, considering the proportion of consultations that should be made until the moment in which the birth happened11.
After being collected, the data was organized in the program EpiInfo, version 7.0. Independent double typing was performed to check for errors and inconsistencies and a database was created. The data were analyzed statistically using the SPSS version 20.0 program. The dependent variable, gestational age, was analyzed under categorization: moderate - 32 weeks to 33 and 6 days - and late 34 to 36 plus 6 days10 and also as a discrete numerical variable. The independent variables were categorized utilizing scientific literature11 or under numerical form.
Normality tests were realized (Kolmogorov-Smirnov) of the variables for statistical analysis as well as an association between obstetric determinants (independent variables) and the Gestational Age (Numeric (Discrete) categorized (Moderate / Late-Dichotomous). Besides that, were realized Chi-square frequency tests and Fischer's exact test. For the correlations, was utilized Pearson's correlation index, considering the characteristics of the variables after normality test. The significance level utilized was of 5%.
Considering the ethical aspects, this study was approved by the Research Ethical Committee of the Federal University of Santa Maria, under protocol number 1.511.201 of 2016 and registry number: 53898916.9.0000.5346. Norms and guidelines for human research resolution number 466/12 from the Brazilian National Health Council were respected.
RESULTS
In the study scenery, during the data collection period, 1371 children were born, of which 281 (20.5%) were born moderate and late premature (MLPMT). It is worth highlighting there is a prevalence of late of 247 (18.0%) of the total of births. As the hospital is reference for the central region of the Rio Grande do Sul state, selection criteria were applied [residing in the county of Santa Maria/RS] and with this, participated in the study 28 (18.5%) moderate preterms and 123 (81.5%) late preterms.
As for the obstetric variables associated to the birth of late and moderate premature babies is presented the Table 1. It is highlighted that each reason for premature birth and or risk pregnancy was analyzed individually in the studied groups [gestational strata (moderate and late)], sought that they could present more than one reason for premature birth or risk pregnancy.
Table 1: Comparison between the groups of moderate and late preterms and the obstetric factors - Santa Maria, RS, Brazil, 2018
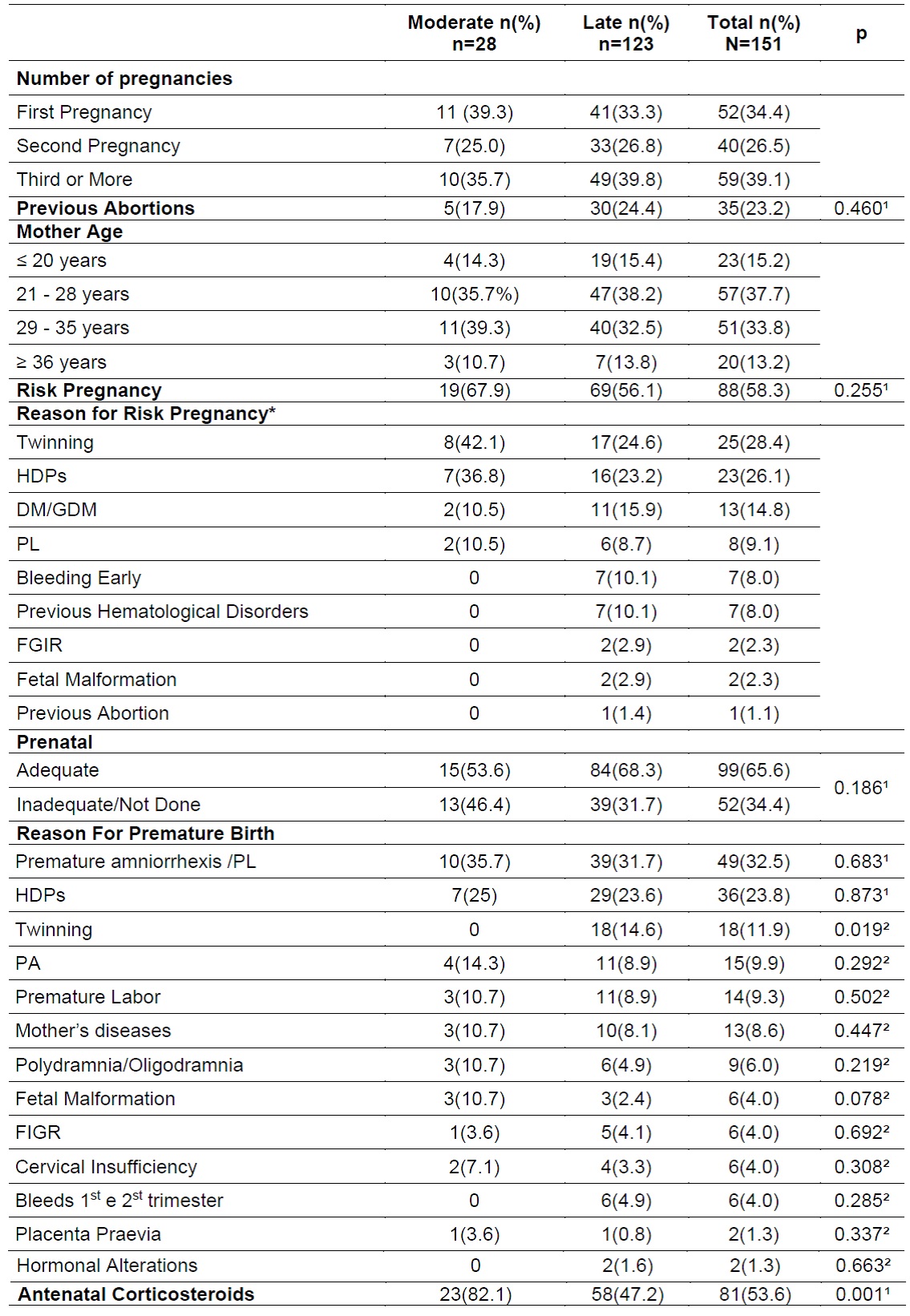
1Chi-square.nd;
2Fischer's exact test; DM/DMG- Diabetes Mellitus/Gestational Diabetes Mellitus; PL: premature labor; PA: placental abruption; HDPs - hypertensive disorders of pregnancy; FIGR - fetal intrauterine growth restriction.
Most pregnant women 99 (65.6%) were not primigravida and 108 (71.5%) had age between 21 and 35 years. 88 (58.6%) of the pregnancies were considered of risk, this prevalence was larger among moderate preterms, 19 (67.9%), although with a non-significant proportion for the variable (p=0.255).
Around 65% of pregnant women had realized an adequate number of prenatal consultations for their gestational period. The reasons for the premature births in both groups was Premature amniorrhexis /PL in 49 (32.5%) cases, followed by hypertensive disorders of pregnancy with 36 (23.8%). There was no significant difference between the groups, with the exception of twinning which presented most frequently proportion in late prematures (p=00.19).
In what refers to gestational age analysis, as a continuous numerical variable, stands out average of participants of 34.8 weeks (SD ±1.2). When the correlations of obstetric factors associated to gestational age were analyzed presented the Table 2.
Table 2: Correlation of the obstetric factors associated with gestational age at birth- Santa Maria, RS, Brazil, 2018
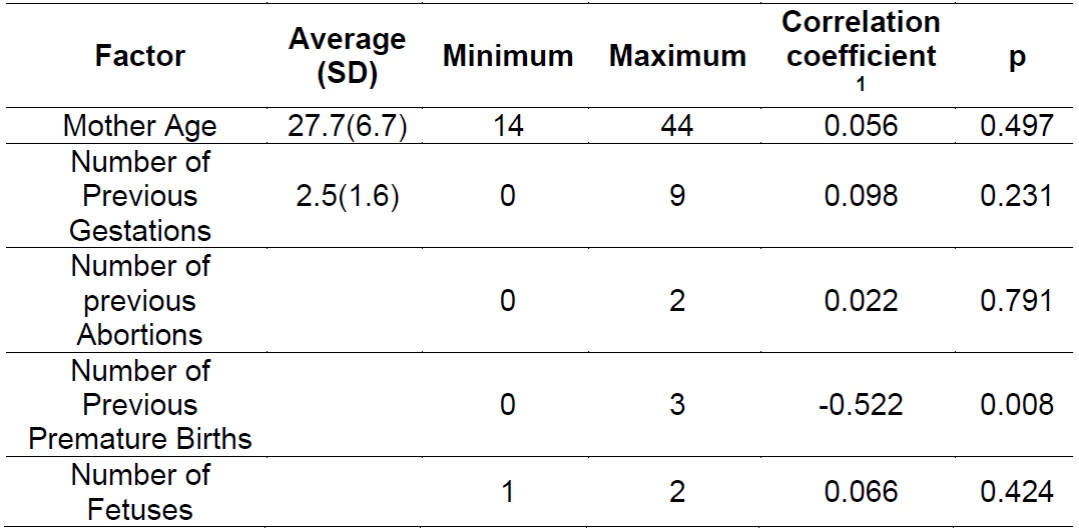
1Pearson's correlation coeficiente
There is no significant correlation between number of previous gestations and gestational age (p=0.231). It is worth highlighting that the only variable inversely correlated to gestational age was the number of previous births, highlighting that the higher the number of earlier births, lower the gestational age at birth (p=0.008). It is emphasized that the rest of the correlations were positive, but not significant.
DISCUSSION
The main obstetric and maternal characteristics of moderate and late premature births revolve around mothers within the age range of 21 to 35 years old, not in the first pregnancy anymore and that had risk pregnancy. The correlation between mother age and gestational age, in this study, did not prove significant, although, according to author, among risk factors for premature birth, mother age is considered notable risk factor since mothers over 35 years of age have 1,3 times higher chances of developing risk pregnancy and result premature birth12.
A study realized in the United States highlights that both younger (adolescent) and older pregnant women had higher chances of premature birth. Thus, the chances of complications increased as maternal age changed in both directions away from the reference group from 25 to 29 years old13.
Beyond maternal age, the etiology of the premature birth must be considered multifactorial and, in a way, is still incipient to literature, even in those extreme prematures. There are several maternal factors involved such as previous diseases and/or acquired in gestation, as well as difficulty of access to support from health services2.
Corroborating with this study, it is implied that underlying diseases or those acquired in the gestational period that characterize risk pregnancy, are also frequent reasons in late and moderate premature births, since almost 60% of babies were born from risk pregnancies. It is emphasized that the frequency was not significantly different between the two analyzed groups (p=0.255), although studies highlight that this characteristic is more prevalent in extreme premature births when compared to the other groups of prematures9,13.
Several underlying diseases have already been related to preterm labor, such as maternal hypertension, utero-placental changes, infectious diseases and heart diseases. The main obstetric complications associated to increased risk of premature births, regardless of gestational age at birth, involve the premature rupture of membranes, hypertensive disorders of pregnancy, oligodramnia and urinary tract infections7,14.
Such data are consistent with the findings of this study, as HDP and premature aminorrhexis/PL together represented more than 55% of reasons for premature births in the population of the moderate and late, which corroborates with the population of born, independent of them being moderate or late. When compared with the same population of prematures - moderate and late- other studies corroborate these findings, highlighting premature amniorrhexis15, HDP16) and the Premature Labor (PL)17 as the main causes that led to early birth.
The premature amniorrhexis was the main reason for prematurity in this research and was prevalent in 32.5% of births. A Brazilian study highlights that premature amniorrhexis is a frequent factor of premature births, mainly in gestations with more than 30 weeks of GA. This corroborates premature birth as the main cause of non-extreme premature births18.
Another frequent cause in relation with premature birth was HDP. Research points out that one of the main complications of HDP is premature birth, which is in line with what was evident with the moderate and late population of this study. The rates of prevalence in premature births for mothers with HDP, according to international study, revolves around 15 and 67% of gestations15, which matches with the about 25% of premature births which had this etiology as the cause founded in this analysis.
Preeclampsia, as an isolated factor, is a great cause of morbimortality in premature births, with maternal risks and to the newborn. Pregnant women with this diagnosis of up to 34 weeks pregnancy have great association with restricted intrauterine growth, low weight at birth, beyond higher rates of preterm births, increasing the risk of perinatal mortality. These factors, beyond representing risk to the NB, are sometimes reasons that add to the maternal-fetal complications of preeclampsia17.
The reasons for the premature birth had little difference between the two groups of prematures, however it is worth mentioning that the twinning was more frequent in the group of late prematures. The twinning was the cause for the premature birth in almost 12% of participants and it was the only reason for premature birth that showed a difference between the studied groups, being more frequent in the late group. In Brazil, twinning corresponds to 2-3% of all the births in the range of the population in general, however it is present between 10 to 17% of births before the 37th week11,13,19.
In this research, it was more frequent in the population of late prematures. It is worth mentioning that this characteristic in the population of late prematures can be justified, since in its majority the early identification of the risk to premature birth due to twinning raises early efforts of tocolysis and the pregnancies tend to last for more time, however justifications in the literature for this relation were not found.
With regard to the correlation between the greater number of previous premature births and the lower gestational age at birth (CI = -0.522, p = 0.008), studies highlight and corroborate these statements11,18, however tocolysis practices are still few considered for women with this risk factor. According to a Brazilian multicenter study, efforts to delay early birth did not differentiate between mothers with previous premature births and those who had not yet experienced prematurity18, which indicates the necessary early identification of this condition in health services.
The improvement in prenatal services and professional and technological qualification favors the maintenance of pregnancy, even in those at risk of early delivery and imminent obstetric, fetal and neonatal complications. This improvement is reflected in the reduction of extreme premature births and thus, moderate and late births have been growing in recent years, when compared to extremes20.
Studies bring up the discussion about elective iatrogenic and cesarean sections, as an important cause of birth, especially of late ones 20,21.
It is recognized that, currently, there is no longer a moment of confirmation of the consistency and magnitude of these relationships from late / moderate prematurity to undesirable outcomes, however we face the discussion and construction of evidence-based protocols for premature pregnancy interruptions22.
Therefore, multi-causal factors that increase risk exist and range from biological to the social ones involved. Author, analyzing the estimates of prematurity rates for 184 countries in 2010, also states that premature birth is a syndrome with a variety of causes classified into two major groups: spontaneous causes and medical causes (induced or elective), by maternal indications, fetal and even iatrogenic2.
The reflex of obstetric aspects influences fetal development and its adaptation to extrauterine life. Many obstetric pathologies are related to immediate neonatal aspects, such as complications during delivery and the need for immediate extrauterine adaptation, assessed through Apgar and the needs for resuscitation in the delivery room. All of these adaptive conditions, related to weight, GA, mode of delivery and complications during delivery, in turn, reflect the need for assistance to the newborn in health services and immediate acute conditions.
In this perspective is that obstetric and neonatal nursing is responsible for its position and role in care. Recognize the factors of premature birth, already discussed, provide care and coordinate the care network of this pregnant woman, with a view to delaying or preventing the outcome of prematurity, as well as providing assistance to premature newborns.
Authors highlight the importance of the performance of obstetric nursing in high-risk pregnancies, with autonomy and effectiveness in the care and reduction of premature births, emphasizing the need for training and specific skills for this23,24.
CONCLUSION
The obstetric factors related to the delivery of moderate and late preterm infants were not statistically significant between the two groups studied. However, twinning was more frequent in the late when compared to moderates. It is also inferred that risky pregnancy is related to the birth of this population of premature babies and that the most frequent reasons for premature birth were amniorrhexis and premature labor followed by preeclampsia.
It is recognized that the birth of moderate and late preterm infants is a growing trend today, which requires obstetric nursing to build subsidies for clinical care in prenatal care, based on tocolysis practices, such as early recognition of factors associated with the birth and referral of pregnant women to specialized services at high risk. As for neonatal practices, it is worth recognizing this emerging and recurring demand and the specific care of this group of newborns, still considered “almost term” and, therefore, little studied.
REFERENCIAS
1. World Health Organization (WHO). Preterm birth. [Internet] Geneva: WHO; 2018 [acesso em 14 abr 2018]. Disponível em: http://www.who.int/mediacentre/factsheets/fs363/en/ [ Links ]
2. Blencowe H, Cousens S, Oestergaard MZ, Chou D, Moller AB, Narwal R, et al. National, regional, and worldwide estimates of preterm birth rates in the year 2010 with time trends since 1990 for selected countries: a systematic analysis and implications. Lancet [Internet]. 2012 [acesso em 22 out 2018]; 379(9832). Disponível em: https://doi.org/10.1016/S0140-6736(12)60820-4 [ Links ]
3. Liu L, Oza S, Hogan D, Chu Y, Perin J, Zhu J, et al. Global, regional, and national causes of under-5 mortality in 2000-15: an updated systematic analysis with implications for the Sustainable Development Goals. Lancet [Internet]. 2016 [acesso em 22 out 2018]; 388(10063). Disponível em: https://doi.org/10.1016/S0140-6736(16)31593-8 [ Links ]
4. Kuzniewicz MW, Parker SJ, Schnake-Mahl A, Escobar GJ Hospital readmissions and emergency departamentvisits in moderate preterm, late preterm, and ealry term infants. Clinical Perinatology [Internet]. 2013 [acesso em 22 out 2018]; 40(4). Disponível em: https://doi.org/10.1016/j.clp.2013.07.008 [ Links ]
5. Salge A, Vieira A, Aguiar A, Lobo S, Xavier R, Zatta, L et al. Fatores maternos e neonatais associados à prematuridade. Revista Eletrônica de Enfermagem [Internet]. 2017 [ acesso em 22 out 2018]; 11(3). Disponível em: https://www.revistas.ufg.br/fen/article/view/47198/23139 [ Links ]
6. Almeida AC, de Jesus ACP, Lima PFT, de Araújo MFMA, de Araújo TM. Fatores de risco maternos para prematuridade em uma maternidade pública de Imperatriz-MA. Rev Gaúcha Enferm [Internet]. 2012 [acesso em 22 out 2018]; 33(2). Disponível em: http://dx.doi.org/10.1590/S1983-14472012000200013 [ Links ]
7. Mally PV, Bailey S, Hendricks-Muñoz KD. Clinical issues in the management of late preterm infants. Curr Probl Pediatr Adolesc Health Care [Internet]. 2010 [acesso 22 out 2018]; 40(9). Disponível em: http://dx.doi.org/10.1016/j.cppeds.2010.07.005 [ Links ]
8. Guimarães EAA, Vieira CS, Nunes FDD, Januário GC, OVC, Tibúrcio JD. Prevalência e fatores associados à prematuridade em Divinópolis, Minas Gerais, 2008-2011: análise do Sistema de Informações sobre Nascidos Vivos. Epidemiol Serv Saúde [Internet]. 2017 [acesso em 22 abr 2018]; 26(1). Disponível em: http://dx.doi.org/10.5123/s1679-49742017000100010 [ Links ]
9. Melo EC, Oliveira RR, Mathias TAF. Factors associated with the quality of prenatal care: an approach to premature birth. Rev Esc Enferm USP [Internet]. 2015 [acesso em 07 jan 2017]; 49(4). Disponível em: http://www.scielo.br/pdf/reeusp/v49n4/0080-6234-reeusp-49-04-0540.pdf [ Links ]
10. Engle WA. A recommendation for the definition of "late preterm" (near-term) and the birth weight-gestational age classification system. Semin Perinatol. [Internet] 2006 [acesso em 20 out 2016];30(1): 2-7. Disponível em: doi:10.1053/j.semperi.2006.01.007 [ Links ]
11. Ministério da Saúde (BR). Secretaria de Atenção à Saúde. Departamento de Atenção Básica. Atenção ao pré-natal de baixo risco. Brasília: Ministério da Saúde; 2012. [ Links ]
12. Moura BLA, Alencar GP, Silva ZP, Almeida MF. Internações por complicações obstétricas na gestação e desfechos maternos e perinatais, em uma coorte de gestantes no Sistema Único de Saúde no Município de São Paulo, Brasil. Cad Saúde Pública [Internet]. 2018 [acesso em 20 out 2018]; 34(1). Disponível em: http://dx.doi.org/10.1590/0102-311x00188016 [ Links ]
13. Teixeira GA, Carvalho JBL, Rocha BG, Pereira SA, Enders BC. Perfil de mães e o desfecho do nascimento prematuro ou a termo. Cogitare Enferm [Internet]. 2018 [acesso em 09 jan 2019]; 23(1). Disponível em: http://dx.doi.org/10.5380/ce.v23i1.51409 [ Links ]
14. Demitto MO, Gravena AAF, Dell'Agnolo CM, Antunes MB, Pelloso SM. High risk pregnancies and factors associated with neonatal death. Rev esc enferm USP [Internet]. 2017 [acesso em 05 nov 2018]; (51). Disponível em: http://dx.doi.org/10.1590/s1980-220x2016127103208 [ Links ]
15. Rassmussen KM, Yaktine AL. Institute of Medicine (US) and National Research Council (US). Committee to Reexamine IOM Pregnancy Weight Guidelines. Weight gain during pregnancy. Washington (DC): National Academies Press; 2009. [ Links ]
16. Silva SM, Mattos LC, Macedo LF, Araújo TS. Perinatal morbidity and mortality in pregnancies that progressed with ruptured membranes at a public hospital in Northern Brazil. Rev Bras Ginecol Obstet [Internet]. 2014 [acesso em 02 nov 2018]; 36(2). Diponível em: http://dx.doi.org/10.1590/1984-0462/;2018;36;2;00001. [ Links ]
17. Guida JPS, Surita FG, Parpinelli MA, Costa ML. Preterm Preeclampsia and Timing of Delivery: A Systematic Literature Review. Rev Bras Ginecol Obstet. [Internet]. 2017 [acesso em 05 nov 2018]; 39(11). Disponível: http://dx.doi.org/10.1055/s-0037-1604103 [ Links ]
18. Dias TZ, Fava ML, Passini JR, Cecatti JG, Tedesco RP, Lajos GJ et al . Tocolysis among Women with Preterm Birth: Associated Factors and Outcomes from a Multicenter Study in Brazil. Rev Bras Ginecol Obstet. [Internet]. 2018 [acesso em 09 jan 2019]; 40(4). Disponível em: http://dx.doi.org/10.1055/s-0038-1642025 [ Links ]
19. Tablie PM, Teixeira RM, Toso G, Matras RC, Fuhrmann IM, Pires MC, et al. Características dos partos pré-termo em hospital de ensino do interior do Sul do Brasil: análise de 6 anos. Revista da AMRIGS [Internet]. 2016 [acesso em 20 out 2018]; 60(3). Disponível em: https://pt.calameo.com/read/00075624651215d2604aa [ Links ]
20. Lisonkova S, Sabr T, Butler B, Joshep KS. International comparisons of preterm birth: higher rates of late preterm birth are associated with lower rates of stillbirth and neonatal death. BJOG [Internet]. 2012 [acesso em 22 out 2018]; 119(13). Disponível em: http://dx.doi.org/10.1111/j.1471-0528.2012.03403.x [ Links ]
21. Joseph KS, Demissie K, Kramer MS. Trends in obstetric intervention, stillbirth and preterm birth. Semin Perinatol [Internet]. 2002 [acesso em 01 nov 2018]; 26(4). Disponível em: https://www.ncbi.nlm.nih.gov/pubmed/12211615 [ Links ]
22. Machado LC, Passini Junior R, Rosa IRM. Late prematurity: a systematic review. J Pediatr. [Internet]. 2014 [acesso em 01 nov 2018]; 90(3). Disponível em: http://dx.doi.org/10.1016/j.jped.2013.08.012 [ Links ]
23. Amorim TV, Souza ÍEO, Moura MAV, Queiroz ABA, Salimena AMO. Perspectivas do cuidado de enfermagem na gestação de alto risco: revisão integrativa. Enfermeria Global. [Internet] 2017 [acesso 07 mai 2020]; 46:515-29. Disponível em: http://dx.doi.org/10.6018/eglobal.16.2.238861 [ Links ]
24. Errico LSP, Bicalho PG, Oliveira TCFL, Martins EF. O trabalho do enfermeiro no prénatal de alto risco sobaótica das necessidades humanas básicas. Rev Bras Enferm [Internet]. 2018 [acesso 07 mai 2020]; 71( Suppl 3 ):1257-64. Disponível em:https://doi.org/10.1590/0034-7167-2017-0328 [ Links ]
Received: March 04, 2020; Accepted: July 19, 2020











 texto en
texto en 


