Meu SciELO
Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Enfermería Global
versão On-line ISSN 1695-6141
Enferm. glob. vol.20 no.62 Murcia Abr. 2021 Epub 18-Maio-2021
https://dx.doi.org/10.6018/eglobal.437711
Originals
Factors affecting adherence to antiretroviral treatment in women with HIV: A sequential mixed model research design
1Murcian Health Service. Murcia. Spain
2Department of Nursing. University of Murcia. Research group Nursing, women and care. IMIBArrixaca. Murcia. Spain
Department of Nursing. University of Murcia. Research group Nursing, women and care.Murcia. Spain
3Departamento de Enfermería. Universidad de Murcia. Grupo de investigación Enfermería, mujer y cuidados. Murcia. España.
Background:
HIV/AIDS is affecting more and more women. Adherence to antiretroviral treatment (ART) is decisive for those infected to achieve quality of life.
Purpose:
The aim of the present study is to determine the degree of adherence displayed by a group of women with HIV/AIDS and to identify those factors and circumstances which might influence their adherence to ART.
Method:
A sequential mixed model research design was applied. The subjects studied consisted of 86 women diagnosed with HIV/AIDS and treated with ART.
Findings and discussion:
Qualitative data were collected from 18 of these women. 59.3% of participants were non-adherents. The determining factors for non-adherence were level of education, age, income, as well as personal and/or interpersonal factors such as socio-familial support, perceived stigma, self-stigma and factors related to disease and treatment. Nursing care should take a gender-focused approach towards those psychological and personal factors inherent in the adherence process.
Key words: HIV Infections; HIV; Anti-Retroviral Agents; Treatment Adherence and Compliance; Women’s Health; mixed methods
INTRODUCTION
HIV/AIDS infection has become a pandemic, with severe consequences for humanity, affecting the lives of 36.9 million people1. Initially, the epidemic affected mainly men, yet current data shows that 57% of all those with HIV are women2.
Since the onset of the epidemic a total of 85,720 cases have been notified in Spain, where HIV is mainly transmitted sexually. Incidence in the region of Murcia is lower than the overall nationwide mean for the entire 2009-2015 period, yet higher than for European Union member states / Western Europe3,4. Regarding those women diagnosed with HIV, 89% of cases in the Region of Murcia are attribuTable to heterosexual transmission and 5% to injecTable-drug use3.
Adherence (ADH) to antiretroviral therapy (ART) acquires immense importance due to its impact on the immune system, since a sub-optimal adherence leads to therapeutic failure and an increase in morbidity and mortality in those with HIV5. There are, therefore, numerous studies which raise the need to explore and consider the social contexts of those undergoing ART in order to identify any required adaptations and favour effective adherence6,7. In this sense, interventions must be designed and planned such that they might be adapted to the needs of specific subgroups, taking into account sociocultural aspects and available support and applying solutions to specific gender-based vulnerabilities in terms of the transmission and development of the disease8,9.
Women with HIV experience multiple forms of discrimination, both due to their socio-economic status as well as their gender, and are stigmatized by the means of transmission 10, such stigma being associated with the perpetuation of isolation and lonelines11.
Emphasis should be placed on family as one of the most important supportive elements as well as on eliminating conflicts generated by discriminatory processes such as social exclusion and the marginalization of people living with HIV/AIDS in the workplace, school and social environments12 or the increase in violence towards women, all of which highlights the need for research to approach this phenomenon in a holistic and exhaustive manner. The fact improvements in adherence have not been achieved is due to most adherence-to-ART guidelines being based on quantitative research focused on the individual, when many of the barriers described require interventions on a community level, precisely that in which affected people live6. Therefore, the main objective proposed by the present study was to determine the degree of adherence to ART by a group of women with HIV/AIDS, as well as to identify and analyse those factors and circumstances which might influence adherence in such women.
METHODS
Study Design
A mixed, sequential, explanatory research design was utilized. This methodology begins with the collection and analysis of quantitative data, to continue on an equal standing with the collection and analysis of qualitative data and ending with an interpretation of the results in which associations are established between the quantitative and qualitative data.
Study Sample
The present study is based on a multifocal approach and was carried out in six public hospitals from six healthcare districts in the Region of Murcia, Spain. The sample was construed according to the following inclusion criteria: women from 18 to 65 years of age, diagnosed with HIV/AIDS, time elapsed to onset of ART of at least 6 months, periodical clinical follow up at reference hospitals. Exclusion criteria were: existence of language barriers, advanced cognitive deterioration, being hospitalized or pregnant at the time of the study.
The sample selection method was probabilistic for the quantitative stage and the sample size was established according to number of patients who collected their medication personally from the hospital pharmacies over the years 2014-2015. Thereby, the total study population was composed of 86 women who met the aforementioned criteria.
During the qualitative stage the study population was composed of 15 women from 18 to 65 years of age, who participated in the quantitative stage and collected their medication from the hospital pharmacies in 2015. Participants were recruited via intentional sampling until reaching data saturation.
Quantitative Stage
This stage involved a retrospective, cross-sectional descriptive design. It is cross-sectional for the following variables: Influential factors towards non-adherence in women undergoing ART and the Degree of adherence shown by women undergoing ART. It is retrospective for the variable Degree of adherence according to the hospital pharmacies’ (HP) dispensing records. In order to obtain data during the qualitative stage the following instruments were utilized:
Questionnaire on Adherence to Treatment in Women with HIV/AIDS CAT-M VIH)13 : this is a questionnaire on adherence, comprised of closed-ended questions with a Likert-style ordinal response scale, constructed and validated previously in women with HIV/AIDS, the latter consisting of closed, dichotomous and/or multiple responses organized into three sections: Socio-Demographic Data, Clinical History and Treatment Adherence Records.
SMAQ adherence questionnaire: A brief questionnaire containing 6 questions to be asked directly to the patient regarding their medication-taking habits that considers patients with a therapeutic compliance of 95% or greater, to be adherent14,15. This instrument has been validated for the Spanish population16.
Blood tests: results for viral load were collected from medical records as an indirect measure of adherence to ART and reinforcement thereof17, and of confirmation of suspected insufficient therapeutic compliance18, CD4/CD8 blood cell counts were utilized for HIV-infection staging, establishing the need for prophylaxis and eventual discontinuation19.
Hospital pharmacy ART dispensing records: providing information on the withdrawal of patients’ medication from the hospital pharmacies and on the continuity of treatments, as well as on changes to new combinations of ART14.
Qualitative Stage
The qualitative design involved an interpretative phenomenological approach in order to comprehend women living with HIV/AIDS, thus building a group perspective based on particular experiences of their unique yet collective realities. In this stage participatory and selective observation were utilized during in-depth interviews. The results were recorded in a field diary to relate and interpret their meanings. A conversational method via semi-structured interviews was applied using topics of interest to be explored. The questions were verified previously by key informants and experts in the field. The interviews were conversational, non-directive, non-judgmental and flexible in order to adapt to each participant’s discourse such that the interviewee might discover, via phenomenology, the motivation behind their behaviour. The interviews were held in a private, amicable and relaxed environment, for which a multipurpose room was arranged in the participant recruitment services department. The mean duration of the interviews was 45 minutes.
Data analysis
The quantitative data was analysed via basic descriptive methods. The comparison of qualitative variables between groups was performed via the Chi-squared method. The degree of concordance between the methods utilized for classifying patients according to adherence was calculated via Cohen’s Kappa index. The statistical analyses were performed using the SPSS V23.0 software for Windows. Statistical significance was established at p<0.05. The qualitative data analysis was based on a latent content approach. The four stages of the analysis were as follows: textual transcription of interviews, organizing and processing of data by identifying the arising coding and context units in order to grasp the exact meaning of each coding unit the reduction of data via the regrouping of codes that provided meaning plus identifying categories and subcategories and the interpretation of data via the search for intragroup relationships as well as relationships between groups of meanings. Subsequently, the data arising from both methods were compared and integrated as is recommended in mixed methods, such that during the interpretation, the qualitative data helped explain and complemented the quantitative data.
Ethical considerations
During the data collection process, all the related information required was provided to participants in a socio-culturally appropriate format. Furthermore, participants were informed of their right to decline to respond to any given topic, as well as the option to withdraw from the interview at any time without penalty. All data obtained underwent strict confidential handling and signed “Informed Consent” forms were procured from all participants. Likewise, their permission was requested to record the interviews in audio format. Following transcription, all recordings were destroyed.
This study has been approved by the Ethical Clinical Research Committee of the University of Murcia and each Hospital in which data collection took place.
Quality criteria
Credibility, transferability and traceability were applied as quality criteria to ensure scientific rigour. Thereby, veracity and credibility of the data were confirmed via the corroboration of experts and participants, transferability via transparency and protocolization of the entire process and traceability via the detailed description of sociodemographic traits of the informants, as well as inclusion and exclusion criteria and the selection process. Furthermore, a methodical data triangulation was performed by gathering information sourced from women from a range of geographical and healthcare areas, comparing and contrasting the results obtained using both quantitative and qualitative tools.
RESULTS
Sociodemographic Characteristics
The sample of the quantitative study is 86 women with HIV/AIDS undergoing ART and that of the qualitative study is a subsample of the quantitative of 15 women with adherence problems to such treatment. The participants are between 20 and 65 years old and have a mean age of 45.5 years for the quantitative sample and a mean of 42.2 for the qualitative sample.
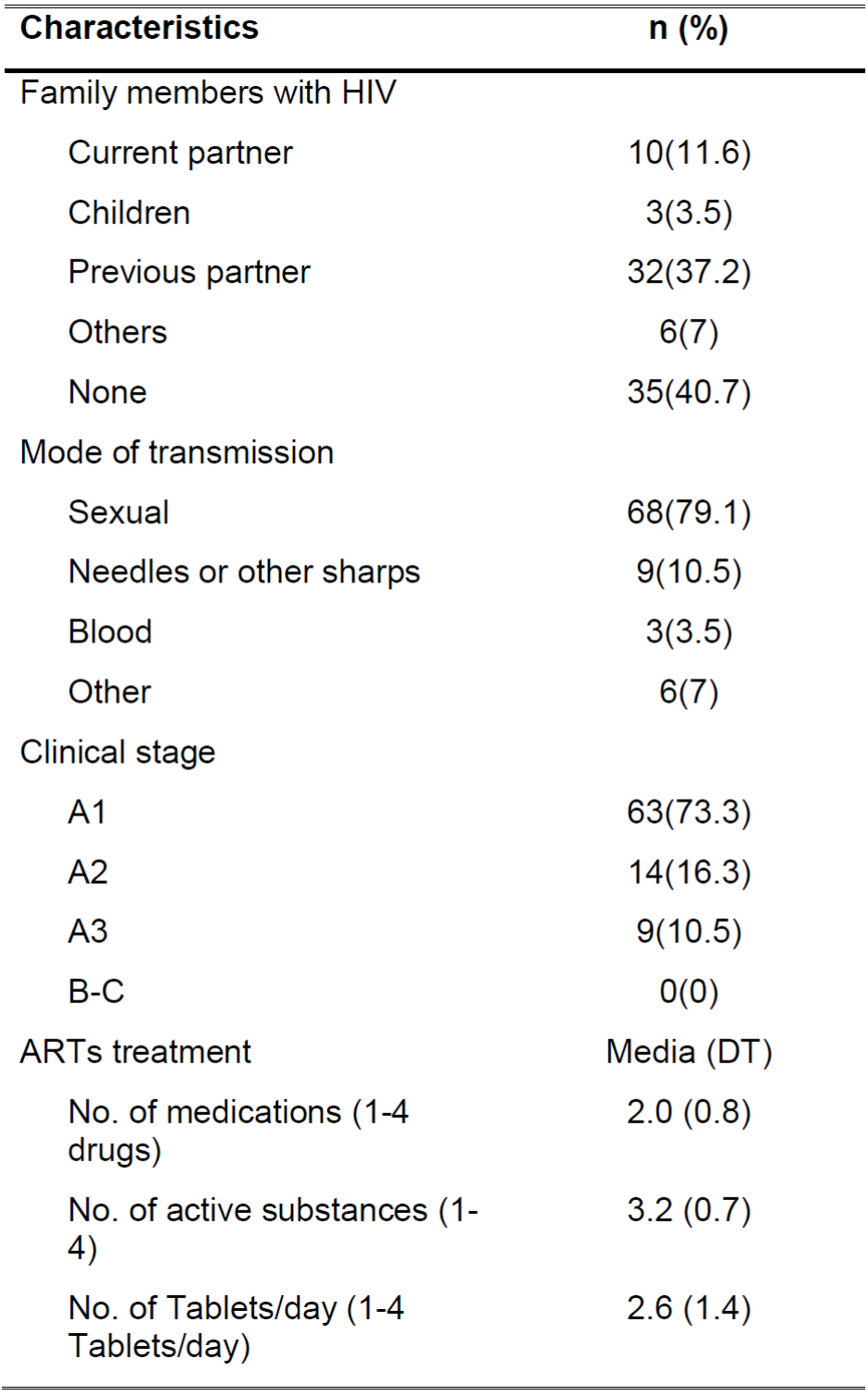
As can be seen in Table 1, the participants in the quantitative sample have a majority level of primary education followed by secondary / high school, 45% are active, 35 have dependent children and 77 are in charge of housework. On the other hand, the profile of the participants with adherence problems (qualitative phase) consists of a woman with basic level studies, with low economic resources (€ 500-700 / month) and with paid jobs (10 participants with work activity recognized) who reconcile with household chores (14).
Quantitative Findings
Clinical characteristics and HIV/AIDS treatment
Table 2 shows the clinical characteristics and HIV/AIDS treatment details. Within the clinical traits it is noteworthy that 79.1% contracted HIV via sexual transmission, 73.3% were in stage A1 of the disease and the viral load of 76.7% of participants was undetecTable.
Regarding treatment, the mean number of medications administered was 2.0 (SD=0.8) with a mean consumption of 2.6 (SD=1.4) Tablets per day and a mean number of active ingredients of 3.2 (SD=0.7). In terms of viral load, there was a significant difference (p=0.008) between adherent and non-adherent patients, with detecTable viral loads being significantly more prevalent in non-adherent than adherent patients (33% and 8.6% respectively).
Adherence to antiretroviral treatment
The analysis of adherence to ARTs treatment via the SMAQ questionnaire showed that 41.9% of participants infected with HIV were non-adherent while the analysis of the hospital pharmacy registries concluded that 40.7% of participants were non-adherent. This produced a degree of concordance between both instruments of 63.95% with a Kappa coefficient of 0.257 (p=0.017). If a participant is non-adherent by at least one of the two methods, she was classified as non-adherent. Thus, 59.3% of the HIV-infected women who participated in the study were non-adherent.
Factors influencing non-adherence to antiretroviral treatment
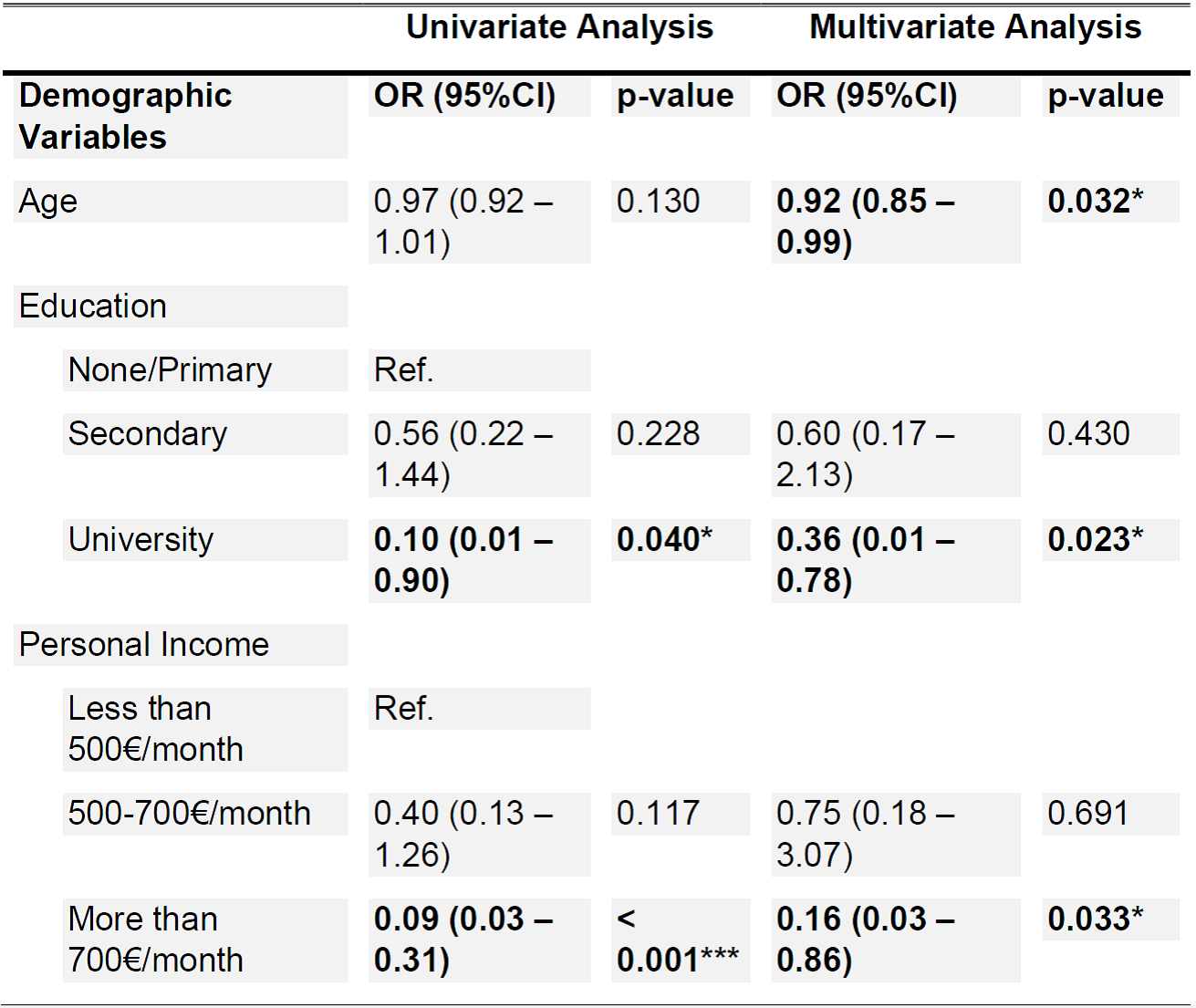
Table 3 displays demographic and clinical variables in terms of non-adherence prediction, thus determining univariantly that participants with university studies are less likely to be non-adherent than those with no education or primary school education at most (OR=0.10, p=0.040). Income also proved to have a significant effect in that women earning more than 700€ per month were less likely to be non-adherent than those with an income of less than 500€/month (OR=0.09, p<0.001). The remaining variables showed no statistically significant effects. On a multivariant level, the variables which proved to have a significant effect were: age, education and income. The older the age the lesser the likelihood of being non-adherent among the sample subjects (OR=0.92, p=0.032).
Qualitative Findings
Based on the quantitative results analysed in the first stage of the present study, a subsample of women with difficulties in adhering to treatment was selected in order to identify factors associated with poor adherence to ARTs. Four main categories arise from the analysis of these semi-structured interviews.
Personal factors
Personal factors which influence adherence to treatment are associated with socio-demographic (Table 1) and cognitive-emotional aspects. The latter are unique and differ from one subject to another, although certain common elements are to be found which will be highlighted subsequently.
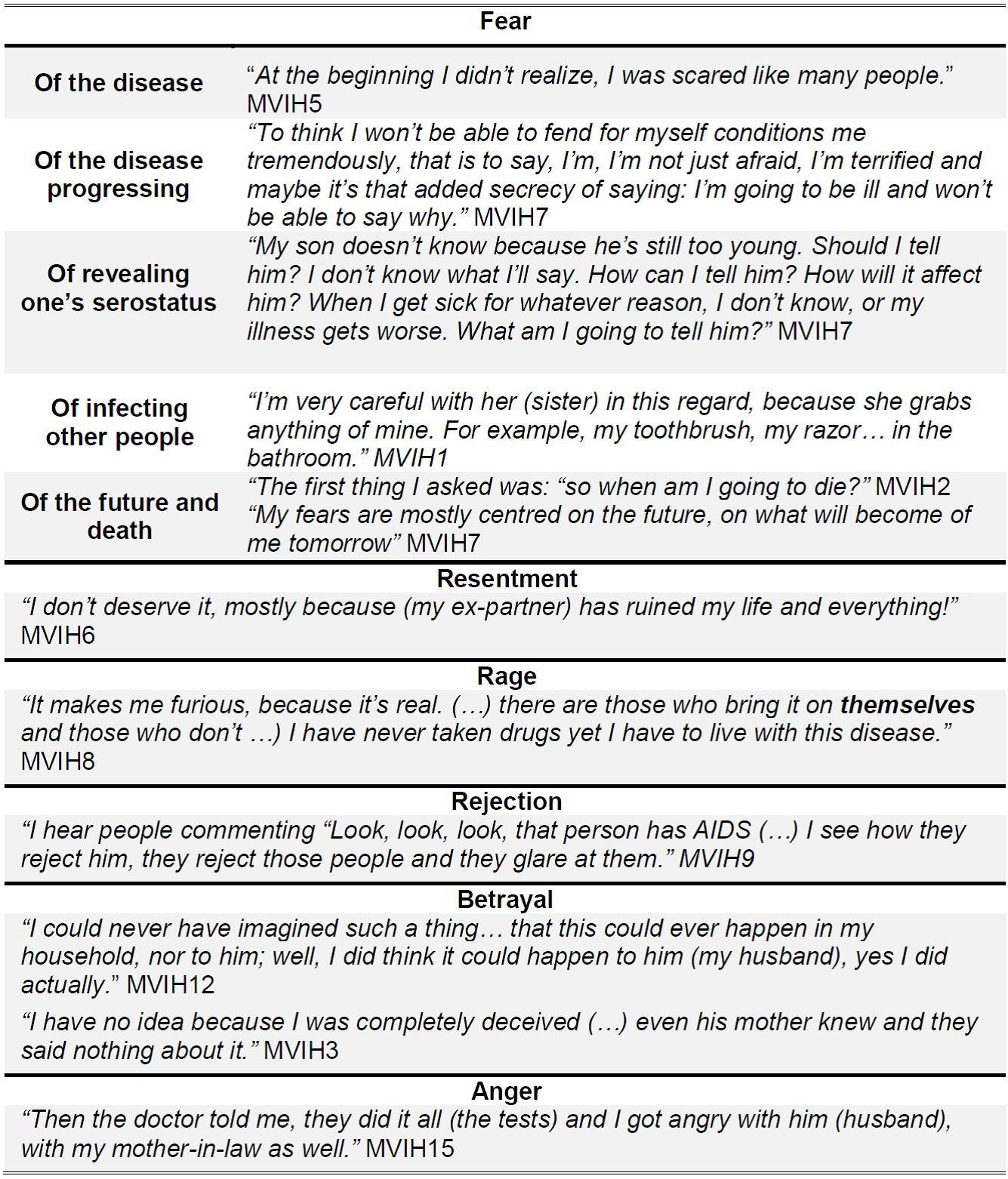
Regarding cognitive-emotional aspects, these were closely associated with interpersonal factors and the appearance of self-stigmatization factors. The feelings and emotions generated on being diagnosed as HIV-positive and associated experiences limit interpersonal relationships and alter the “everydayness” of participants. In this sense, the main feeling identified in the participants of the present study was fear, although other feelings also emerged, such as resentment, rage, rejection, betrayal or anger (Table 4).
Moreover, fear stood out as a determinant for maintaining proper adherence to ART. Fear of the progress of the disease, of infecting third parties and of others learning of their serostatus leads them to becoming incapable of collecting and taking their medication on a regular basis. This in turn produces behaviour aimed at concealing any activity that might associate them with HIV, including visits to the Hospital Pharmacies to collect ARTs.
“You have to have a little bag for medication hidden inside your handbag/suitcase so no-one can see which medication you’re taking in case they ask: “What’s that you’re taking?”” MVIH7
“I can’t hand the box (of ARTs) to just anyone because it says so on the box and you know yourself with a mobile phone number in no time… they’ll rob you of everything” MVIH13
Interpersonal factors
The main interpersonal factors which have a negative impact on adherence to ART are: socio-familial support, self-stigmatization and perceived socio-familial stigma.
Socio-familial support can be a factor which favours adherence to treatment when it is positive:
“My cousin came to Madrid to tell me I had HIV and had to take medication (…). “You have to take this medication and live a normal life” and I said: “Oh, well that’s that then! Take medication” (…) I was taken to an association in Murcia to get informed (…).” MVIH2
In this regard, support and comprehension within couples prevents concealment issues, reducing levels of self-stigmatization and normalizing the disease process:
“The person who really supported me in every sense was my partner: by talking with me, advising me and not leaving me for even one second, by supporting me with the treatment” MVIH1
Nonetheless, it can also act as a detrimental factor for adherence when it is negative, directly influencing the emotional stability of the participants, occasionally becoming an incentive for concealing their serostatus, even if this meant complicating the collection of medication:
“To look for support …is something you can’t do (…). You can’t talk with everyone or look for support openly, it’s better they don’t know.” MVIH7
“Regarding work, because practically I can’t … actually, I can say “I have a Doctor’s appointment”, yet the less absent I am, it would seem, less explanations I have to give (…) due to my profession, since I attend to members of the public, the less people know the better.” MVIH11
Conversely, the processes of labelling and assimilation of beliefs and prejudices related to HIV/AIDS, both by infected women and by their social, familial and working environments, directly and negatively affect ongoing optimal adherence to ART. The belief that everyone rejects, or would reject, others due to their serostatus, drives women with HIV/AIDS to seek concealment strategies for the entire range of situations they must face regarding their illness and ART.
“I cleaned up the blood, I put on a glove, I did what I had to do to stop the bleeding and carried on working!” MVIH2
“Every time I go to have blood tests done, I have to come up with an excuse (…).
Every time I have to go and collect medication, I have to make up an excuse (…).
Each time I go to the Doctor, I have to make something up” MVIH7
Factors related with HIV/AIDS
The acceptance of and attitude towards this illness to a large extent determine adherence to ART, but it is also directly related to the acquisition of habits such as self-care and caring for one’s surroundings which complement pharmaceutical treatments.
The presence of HIV/AIDS permeates the feelings and emotions of the women who suffer from it throughout their entire their lives. All of these factors, together with their attitude towards HIV and ART will come to determine adherence. Participants are to be found with either positive or negative coping mechanisms and it is difficult to discern between feelings of acceptance, conformity or resignation towards the situation. Nonetheless, the participants have adapted to living with the illness, despite having developed defensive attitudes towards the social prejudices which drive self-stigmatization and perceived socio-familial and socio-workplace stigma. This leads them to conceal the illness, to minimize it and even attempt to forget they have HIV:
“There are worse things and by worse things I mean, there are people who can’t even move or anything.” MVIH5
“I think I have adapted to it (HIV) (…). Up until now I’m doing fine. I have assimilated it.” MVIH1
The degree of acceptance of the illness displayed by some participants and resignation by others, led them to incorporate new lifestyle habits, encouraged by professional advice, in order to keep healthy:
Nutritional self-care: “I try to eat well, I take vitamins and I always say you have to work, because by working one remains keener.” MVIH1
Mental-health self-care: “Many a time I jump on my motorcycle and head to the countryside for a spin or I go window shopping to distract myself, so as not to think, so as not to think.” MVIH9
Medical check-ups, blood tests and pharmacological reviews: I continue to have blood tests” (…) I visit the doctor on my own, I have the tests done and go alone (…) My chest x-ray is fine, bone tests are fine, it’s all fine, it’s just that “I’ve got this and I’ve got to keep an eye on it.” MVIH8
Sexual health: “Now I know that this isn’t … one has to take care when it comes to sexual relations, just like other diseases which are caught more often” MVIH5
Such routines are also associated with taking care of one’s surroundings, mainly to avoid disease transmission.
Caring for the family: “We had the (HIV) tests done on my son as well but he came up negative (…) I have a daughter who is fine, I had her tests done and she’s fine.” MVIH8
Caring for healthcare professionals: “When I go to the doctor, it (having HIV) is the first thing I tell them, the dentist even, that’s right, the very first thing, I always tell them straight up.” MVIH15
Conversely, those participants who have not accepted the fact they have the disease develop ineffective (negative) coping mechanisms. This finds them not developing the self-caring attitudes necessary for a proper and effective adherence to treatment:
“I have never accepted it” (…). “It´s difficult to accept it (…). The first year I had it, I shut myself indoors, not even a window open; everything totally shut.” MVIH1
“No, accept it (HIV)? I will never accept it, ever, because I don’t deserve it, because I didn’t do anything to bring it on myself.” MVIH6
Factors related with ART
The prognosis and quality of life of HIV patients depend on the degree of therapeutic compliance with ART. Along these lines, the importance of and adhesion to treatment were analysed as factors related with ART, as was attitude towards ART and perceived efficacy.
It was thereby found that the greater part of the participants reported having received information on ART from qualified professionals, the importance of proper adherence and the consequences in terms of disease progression associated with low or non-adherence.
“The Doctor said to me: …you will have to take medication, this medication will be your lifeline (…). If you follow the treatment properly … you have a chance at a somewhat longer life (…). I had already been informed very well about the disease, about what happens when you do certain things, if you don’t take the medication, what happens step-by-step, basically everything.” MVIH3
“Everyday (I take ART) in the morning. I was told: if you take it in the afternoon, then in the afternoon it is, if you take it in the morning, then in the morning it is, but never ever change the time.” MVIH9
Nonetheless, there was one case reported of not having received sufficient information regarding the dose and timing of the treatment, which led to self-administration errors.
“When I started with the pills, the first time I took them they didn’t explain how I was supposed to take them properly (…) I took them all in one go, I became very unwell with high fevers!” MVIH2
As such, correct professional healthcare information and education can have a positive effect on both adherence to and proper administration of ART.
Furthermore, the information received by the study participants favours positive attitudes towards ART and the perception that treatment is effective. In this regard, most participants reported trusting in ART and perceived its effectiveness:
“I am aware that without this medication I would be as (good as) I am (…). It’s enough for me to know I’m doing fine, because the Doctor tells me so, and besides the Doctor, I see the blood tests and I know I’m doing well, because my defences are up quite a bit.” MVIH1
Notwithstanding, although the attitudes towards and the perception of the efficacy of ART was positive among the majority of the participants as well as the treatment being considered responsible for their wellbeing, despite their illness, in some cases contradictory statements were noted with regard to adherence to ART, raising some suspicion as to a possible low adherence. This is based mainly on statements revealing delays in dosing regimen, the existence of leftover Tablets and sporadic omissions in administration.
Improper dosing regimen: “(…). When I have a drink, I take my medication a little later than normal so as to not mix it with the (alcoholic) drink, but I never skip taking it, I never skip a day.” MVIH1
Surplus medication: “I’m handling the treatment well, I mean, I take it (the medication) (…). There are months I go and months I don’t because I’ve got pills to spare, I say: “Why bother going all that way? (…). One Tablet every night and that’s that, that’s my day-to-day…” MVIH13
Dosing omissions: “I keep up with my medication. My Doctor told me it was long term and I can’t stop taking it, I have to follow instructions to the letter (…). Well, I’m carrying on, although sometimes I forget and then pick it up again, and so on, but I’m still on it.” MVIH15
Further important factors related to adherence to ART are side-effects and simplifying treatments. In this regard, reducing the number of pills on a daily basis can be seen to favour adherence: “At first you have to take up to a dozen pills, I had forgotten, now, thank God, one is enough (…) I have never had any side-effects, none whatsoever, and mine’s (viral load) undetecTable” MVIH8. Likewise, the side-effects associated with treatment pose a barrier to proper adherence: “In the mornings I wake up quite poorly, I get terrible acid reflux and I told the Doctor I couldn’t go on like this, I went 2 - 3 days without taking the medication because I wasn’t tolerating it.” MVIH1
DISCUSSION
To be informed of a HIV diagnosis creates a strong emotional impact in women which in turn produces shock, denial, surprise and fear. Participants reported such an impact greatly limits interpersonal relationships and alters daily life. Among the feelings that pervade the lives of those interviewed, fear of unknown aspects of the disease, of worsening health, of the physical manifestations of HIV, of the discovery of their serostatus, of facing their future and of infecting third persons are all to be emphasized. Furthermore, an unfounded sense of guilt worsened stress levels in these female participants, which is considered a predictor for low adherence. In this regard, emotional impact, psychological anguish and depressive symptoms which develop during the illness, are associated with a drop in adherence11 Further elements highlighted by participants in the present study were stigma and self-stigmatization. Stigma is another factor associated with low adherence20 and although there is no statistically significant association between stigma and gender, there tends to be a greater presence of self-stigmatization among women20. The issue of seropositivity being related with behaviour construed as immoral finds women with HIV presenting reported perceived stigma from friends, family and healthcare professionals21. Regarding the latter statement, ignorance of the disease causes HIV to be associated with promiscuity and drug use. As such, some women see their reputation questioned and feel obliged to clarify to the contrary.
Of the participants in the present study, 79.1% contracted the disease via sexual transmission related with their partner concealing their serological status from them. These data reflect the greater biological and social vulnerability of women to becoming infected with HIV19. In addition to biological vulnerability, the present study reflects the social and workplace susceptibility of women who live with HIV/AIDS. Although legal coverage exists in Spain22, study participants detected discriminatory situations in the workplace and discriminatory situations related with the violation of their confidentiality. These situations and the stigma in the workplace perceived by the participants, generate situations of hiding the disease, fear of being fired, stressful situations linked to injuries in the workplace, hiding medication, medical appointments or fear of taking the ART in public, making ADH very difficult 23.
The aforementioned issues and the stigma in the workplace perceived by the participants, lead to the concealment of the disease, a fear of being dismissed and of other stressful situations associated with injuries in the workplace. Such scenarios produce high levels of psycho-social suffering in seropositive women and the stigma associated with HIV perpetuates isolation and solitude as a refuge for concealing ones serostatus11.Thus, self-stigmatization and fear of discrimination hinder the initiation of relationships and the creation of social support networks.
Social support is the most relevant factor for adherence and an essential aspect of coping and committment skills for improving adherence to ART24. In the study participants, social, family and work support has been described as insufficient or non-existent, which may be one of the precipitating elements of therapeutic non-compliance of 59.3%. Within the social support concept, positive personal relationships improve the experience and acceptance of the disease and in turn improve adherence to ART. However, negative experiences on a community and family level compromise adherence due to ruptures in the social fabric and difficulties within the family microsystem25. Reason why, social health care should focus its efforts not only on the individual but also in their social environment6.
The need to establish strategies to promote and / or improve ADH is evident, applying the gender perspective to avoid bias in health care 26 and establishing programs focused on improving self-esteem and strengthening the attitude towards the disease through emotional support 27.
Study Limitations and Strengths
In general terms, sample size may be a factor limiting the extrapolation of results. Therefore, in the quantitative stage, data from several instruments were utilized and cross-referenced in order to confirm the outcomes. further limitation to the quantitative stage which is to be highlighted is that the SMAQ questionnaire overestimates adherence since it is self-referring14,28 and lies in the SMAQ questionnaire presenting a limited scoring system and a predisposition to please. Furthermore, the pharmacy registry overestimates adherence given that it assumes patient take the medication registered therein. Nonetheless, the combination of both methods enables the degree of adherence to be adequately analysed29.
Likewise, in the qualitative stage theoretical data saturation was achieved. In this stage, it was also not possible to discard certain social desirability bias in which participants might modify their responses for the sake of better appearances, mainly supported by the self-stigmatization processes described in the results. Notwithstanding, there was an element of trust in the relationship between the interviewer and the participants given that the former was a pharmacy staff member and was familiar with their adherence status, which facilitated a more open dialogue on matters of personal motivation and gender with regard to adherence to treatment.
Implications for Future Research and Practice
Generally, nursing care should not be limited to a biological and social level, but should also involve the existential sphere, in order to respect patient dignity and help compensate for the deficits produced when a person’s health is lacking. In this sense, healthcare for women with HIV/AIDS should be oriented towards developing educational and guidance protocols with gender and cultural considerations in order to address the psycho-social factors involved in adherence processes. Approaching social determinants of health such as socio-economic and educational status are noteworthy elements to be developed in the endeavour to improve ADH.
REFERENCIAS
1. ONUSIDA. Estadísticas mundiales sobre el VIH de 2017. Hoja informativa- Día Mundial del Sida 2018 [Internet]. 2018 [Citado el 24 de abril de 2020]. Disponible en: http://www.unaids.org/es/resources/documents/2018/UNAIDS_FautSheet [ Links ]
2. ONUSIDA. Informe mundial ONUSIDA, Informe sobre la epidemia mundial de Sida 2013 [Internet]. 2013[citado 20 de abril de 2020]. Disponible en: http://www.unaids.org/sites/default/files/media_asset/UNAIDS_Global_Report_2013_es_1.pdf [ Links ]
3. Centro Nacional de Epidemiología- ISCIII. Vigilancia Epidemiológica del VIH y sida en España: Sistema de Información sobre Nuevos Diagnósticos de VIH y Registro Nacional de Casos de Sida. Área de Vigilancia de VIH y Comportamientos de Riesgo. [Internet] 2016 [citado 27 de abril de 2020]. Disponible en: www. Isciii/ISCIII/es/contenido/fd-servicios-cientifitecnicos/fdvigilancias-alertas/fdenfermedades/fds-sida/pdfsida/Informe_VIH_SIDA_2016_def.pdf [ Links ]
4. European Centre for Disease Prevention and Control. Annual Epidemiological Report 2016- HIV/AIDS.Stockholm: ECDC. Stockholm: ECDC; 2016. Disponible en: http:// ecdc.europa.eu/en/healthtopics/aids/surveillance-reports/Pages/Annual-Epidemiological-Report-2016.aspx [ Links ]
5. Panel de expertos GeSida/ PNS. Recomendaciones de GeSida/Plan Nacional sobre el Sida respecto al tratamiento antirretroviral en adultos infectados por el virus de la inmunodeficiencia humana [Internet]. 2018. Disponible en: http://www.gesida-seimc.org/wp-content/uploads/2018/01/gesida_TAR_adultos_v3-1.pdf [ Links ]
6. Barroso J, Leblanc N, Flores D. It´s not just the pills: A qualitative meta- synthesis of HIV antiretroviral adherence research. J Assoc Nurses AIDS Care. 2017;28(4):462-78. doi: 10.1016/j.jana.2017.02.007. [ Links ]
7. Shubber Z, Mills EJ, Nachega J b., Al. E. Patient-reported barriers to adherence to antirretroviral theraphy: a systematic review and meta-analysis. PloS Med. 2016;13. doi: 10.1371/journal.pmed.1002183. [ Links ]
8. Puskas C, Hogg R. Unlocking adherence: is gender the key? Lancet. 2014;2(1). doi: 10.1016/S2352-3018(14)00033-2 [ Links ]
9. Kanters S, Park JJ, K.. Interventions to improve adherence to antiretroviral theraphy: a systematic review and network meta-analysis. Lancet HIV. 2017;4(1):31-40. doi: 10.1016/S2352-3018(16)30206-5 [ Links ]
10. UNAIDS. 5 Years since ICPD. 2017. Disponible en: http://www.unaids.org/publications/documents/human/gender/newsletter.pdf. [ Links ]
11. Peltzer J, Ogawa L, Tusher S, Farnan R, Gerkovich M. A Qualitative Description of HIV- Infected African American Women´s Experiences of Psychological Distress and Their Coping Strategies. J Ass Nurses AIDS Care. 2017;28(2):226-37. doi: 10.1016/j.jana.2016.09.010. [ Links ]
12. Rivera M, Varas N, Coriano D, Padilla M, Reyes M. Ellos de la calle, nosotras de la casa: el discurso patriarcal y las experiencias de mujeres que viven con el VIH/SIDA en Puerto Rico. In: La agenda emergente de las ciencias sociales Conocimiento, crítica e intervención (5o Congreso Nacional de Ciencias Sociales). Consejo Me. Madrid; 2015. p. 682-92. [ Links ]
13. Varela MT, Salazar IC, Correa D, Duarte C, Tamayo JA, Salazar AE. La evaluación integral de la adherencia al tratamiento en mujeres con VIH/SIDA: validación de un cuestionario. Rev Col Med,. 2009;40(4):386-97. doi: 10.15446/rsap.v17n4.38429 [ Links ]
14. Ibarra O, Morillo R. Lo que debes saber sobre la adherencia al tratamiento. Sociedad Española de Farmacia Hospitalaria (SEFH) [Internet]. Boehringer Ingelheim, editor. Badalona; 2017. Disponible en: www.sefh.es/bibliotecavirtual/Adherencia2017/libro_ADHERENCIA.pdf [ Links ]
15. Limaylla M, Ramos N. Métodos indirectos de valoración del cumplimiento terapéutico. Cienc e Investig. 2016;19(2). [ Links ]
16. Knobel H, Alonso J, Casado J, Collazos J, González J. Validation of a simplifield medication adherence questionnaire in a large cohort of HIVinfected patients: the GEMMA Study. AIDS. 2002;16(4):605-13. doi: 10.1097/00002030-200203080-00012 [ Links ]
17. Bonner, K., Mezochow, A., Roberts, T., Ford, N.,& Cohn, J. (2013). Viral load monitoring as a toll to reinforce adherence: a systematic review. J Acquir Immune Defic Syndr. 64(1):74-8. [ Links ]
18. Panel de expertos GeSida/SPNS. Factores que condicionan el exito del tratamiento antirretroviral. En GeSida/PNS., Documento de consenso de Gesida/Plan Nacional sobre el sida respecto al tratamiento antirretroviral en adultos infectados por el virus de la inmunodeficiencia humana. Ministerio de Sanidad Servicios Sociales e Igualdad de España. Madrid; 2016. 82-86 p. [ Links ]
19. Asboe D, Aitken C, Boffito M, Booth C, Cane P. British HIV Association guidelines for the routine investigation and monitoring of adult HIV-1 infected individuals. HIV Med. 2011;13(1). doi: 10.1111/j.1468-1293.2011.00971.x [ Links ]
20. Li L, Lin C, Ji G. Gendered Aspects of Perceived and Internalized HIV- Related Stigma in China. Women Health. 2016;59(7):1031-43. doi: 10.1080/03630242.2016 [ Links ]
21. Valencia- García D, Rao D, Strick L, Simoni J. Women's experiences with HIV - related stigma from health care providers in Lima, Peru:" I would rather die than go back for care". Heal Care Women Int. 2017;38(2):144– 158. doi: 10.1080/07399332.2016.1217863 [ Links ]
22. Molero F, Fuster M. La influencia del prejuicio y la discriminación. Encuentro FIPSE sobre la investigación de la perspectiva social del VIH/Sida. FIPSE, editor. Asturias; 2006. [ Links ]
23. Knowlton R, Bohret A, Yang Cui WL, Chande G. Main partner factors associated with worse adherence to HAART among women in Baltimore Maryland: a preleminary study. AIDS Care. 2011;23(9):1102-10. doi: 10.1080/09540121.2011.554516 [ Links ]
24. Caiola C, Barroso J, Sharron L. Black mothers Living with HIV picture the social determinants of health. J Ass Nurses AIDS Care. 2018;29(2):204-19. doi: 10.1016/j.jana.2017.09.011 [ Links ]
25. Garibi C. La compleja relación violencia de género- sida. Un acercamiento a la violencia institucional como factor de vulnerabilidad de las mujeres ante un VIH. Sex salud y Soc. 2009;3:82-105. Disponible en: http://www.insp.mx/salud/index.html [ Links ]
26. Valls-Llobet C. Manifestaciones y medicalización del malestar en las mujeres. Consumo. Ministerio de Sanidad y Consumo (Observatorio de la Salud de la Mujer) y la Universidad Complutense de Madrid (Grupo de Investigación Estilos Psicológicos, Programa de formadores/as en perspectiva de género en salud. Madrid; 2005. [ Links ]
27. La Fauri M, Zíñiga M. Mujeres colombianas viviendo con el VIH/Sida: Contextos, experiencias y necesidades de cuidados de enfermería. Enfer Glob. 2011;10(24):317-27. doi: 10.4321/S1695-61412011000400024 [ Links ]
28. Pagès- Puigdemont N, Valverde-Merino MI. Métodos para medir la adherencia terapéutica. ARS Pharm. 2018;59(3). doi:10.30827/ars.v59i3.7387 [ Links ]
29. Ortega Valin L. Adhesión al tratamiento Antirretroviral: Una actualización. In: 2o Seminario de Atención Farmacéutica (Grupo de trabajo de la SEFH) Libro de sesiones. Icono. Madrid; 2002. p. 178-90. [ Links ]
Received: July 20, 2020; Accepted: September 25, 2020











 texto em
texto em