My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Enfermería Global
On-line version ISSN 1695-6141
Enferm. glob. vol.20 n.62 Murcia Apr. 2021 Epub May 18, 2021
https://dx.doi.org/10.6018/eglobal.428511
Originals
Preliminary study of the end-of-life process through data triangulation in a regional Hospital
1Facultad de Ciencias de la Salud de Melilla. Universidad de Granada. Departamento de Enfermería. España. maso@ugr.es
2Facultad de Educación y del Deporte de Melilla. Universidad de Granada. Departamento de Métodos de Investigación y Diagnóstico en Educación. España.
Objective:
To know the characteristics of the end-of-life process in a Regional Hospital, according to the actors involved, establishing convergence/divergence elements in care process, decision-making, information and knowledge.
Method:
Observational, cross-sectional, descriptive, convergent of mixed methods and data triangulation study. Carried out on a sample of 63 subjects, of which 25 were health professionals, 19 family caregivers and 19 medical records of patients who died in the course of a year.
Results:
Data triangulation shows discrepancies between family members and health professionals regarding care quality and the information provided. The lack of documentation in medical records of care aspects related to decision-making or terminal sedation stands out.
Conclusion:
This study provides an integrated view of end-of-life care provided in a Regional Hospital, identifying priority areas of intervention in order to improve quality of life in this process, such as patient involvement in decision-making, appropriate completion of medical records and health professional training.
Key words: Palliative Care; Research Techniques; Patient Care; Family; Health Personnel
INTRODUCTION
Terminally ill patients, as well as their families and the health professionals who care for them, face a complex situation1 that requires comprehensive assistance aimed at each of the actors involved in this process. In addition to presenting physical signs and symptoms such as pain, malnutrition and the effects of treatment, patients require attention to other needs such as respect for their decisions, privacy, adequate information, understanding, compassion and assistance in facing their situation. This implies the need to provide psychological, social and spiritual support to both patients and their families and to have a health team with specialized training, especially in bioethical aspects, communication skills, emotional support and teamwork dynamics, working in a coordinated and effective way among the different health care network settings2.The multidisciplinary nature of the health teams requires that, beyond specific training and skills of each professional field, a shared training is provided, in which each team member knows what the other does in order to offer a real and quality comprehensive care.
Regarding the aspects that determine proper care in this process, the majority of the reviewed studies highlight access to palliative care, training and experience of health professionals, treatment objectives, comprehensive care provision, patient and family involvement, end-of-life planning and respect for patient wishes3)(4)(5.
In clinical practice, the high rate of hospitalization of patients in this situation is more associated with aggressive treatments directed towards prolonging life rather than alleviating symptoms. Likewise, it is frequent that during hospitalization patients have scarce information, communication and participation in the process5,6.
The existence of different organizational models, heterogeneity of resources, diversity of the level of training of health professionals, as well as cultural, political, ethical and religious aspects, determine the approach of the end-of-life process. All of these factors make up a care complexity that must respond to different areas of need, knowing the perspective of the different participants involved in the process7)(8)(9)(10.
Several studies have analyzed these issues from health professionals experience, highlighting the need for adequate training to provide quality care11)(12)(13. In relation to the selection of the place where care is provided, some authors find discrepancies in the perception that health professionals and families have when deciding on home care, highlighting the importance of learning to work in conjunction with good professional-caregiver coordination, the provision of resources and patient participation in this decision6. It is important to analyze the quality of life of the caregivers, the extent of knowledge about diagnosis and prognosis and communication between patients, families and health professionals in hospital units that provide end-of-life care14.
The project was carried out at the Melilla Regional Hospital, which is the only one in the city and has a capacity of 172 beds, serving a population of 86,120 inhabitants, according to recorded data from the National Institute of Statistics in 201715. Due to the frontier nature of this city, this health center serves a population with a significant cultural diversity that increases the complexity of health care at the end-of-life. The aims of this study were: to analyze how the end-of-life care procedures are developed in oncological and non-oncological patients hospitalized in this city according to the actors involved, identifying elements of convergence/divergence in pre-established categories: care process, information and knowledge about diagnosis, prognosis and treatment, and decision-making.
METHOD
Study design
The methodological framework was that of mixed methods research, an orientation that allows a comprehensive investigation to address complex situations, under an approach that combines two or more strategies, quantitative or qualitative, in a single research project16.
Different sources and methods of data collection have been used to seek convergence/divergence through triangulation16,17. In this case, the sample consists of 3 categories of participants (family members, patients and health professionals) and different perspectives, on which an observational, cross-sectional, descriptive, convergent of mixed methods and data triangulation study was carried out. Data were organized in 3 defined categories for analysis: 1) health care process, 2) information and knowledge of health status and clinical situation, and 3) decision-making.
Participants and settings
Participants were:
Health professionals at the Melilla Regional Hospital from the following units (given that there is no specific palliative care unit): Surgery (32 beds), Internal Medicine (32 beds) and Intensive Care Unit (ICU) (6 beds), selected by intentional sampling, maintaining the 1:2 physician/nurse ratio according to the number of physicians and nurses that made up the staff of the units in which the study was carried out. Inclusion criteria were: to be part of the above mentioned units staff at the time of data collection and to agree to participate by signing an informed consent. Each participant represented a case. Professionals who had been working in the unit for less than six months were excluded, as well as errors in the filling of the questionnaire.
Medical records of patients who have died over the course of a year. As inclusion criteria, it was established that the cause of exitus stated in death records of the documentation service were chronic diseases such as Oncological Disease, Chronic Kidney Disease (CKD), Respiratory Insufficiency/Chronic Obstructive Pulmonary Disease (COPD), Heart Failure (HF) and Liver Failure (LF). Deaths that occurred within 24 hours of admission were excluded, as well as records in which several diagnoses were registered as the cause of death and those in which renal, respiratory, cardiac and/or hepatic failure were the cause of the exitus but as complications of other diseases. 19 histories were analyzed in total.
Family member / primary caregiver of patients who died in the hospital that met the following inclusion criteria: family member of a patient who died due to an advanced or terminal illness directly involved in patient's care during the end-of- life; a period of between 1 and 6 months should have elapsed from the death of the patient; and family caregiver acceptance to participate in the study. Each participant represented a case. Family caregivers who at the time of the survey showed difficulties in remembering data or were in a significant state of psychological distress were excluded.
After the application of the inclusion and exclusion criteria, the study was carried out on a sample of 63 subjects, of which 25 were health professionals, 19 family caregivers and 19 medical records of deceased patients.
The small sample size is determined by the reduced units capacity and beds in which terminally ill patients are located.
Once reviewed the literature and after consulting expert panels from different disciplines (nursing, medicine, anthropology, social services and psychology), ad hoc questionnaires were prepared to collect data from health professionals and family members. Health professionals questionnaire consisted of 23 items using a Likert-type scale with five options, ( 1 = totally disagree and 5 = totally agree; 1 = low quality and 5 = high quality; 1 = uncommon and 5 = very common; 1 = not an obstacle and 5 = it is a serious obstacle, according to the question) The questionnaire was divided 11 sections that included data on care structure and process; physical, psychological, social, cultural and spiritual/existential aspects of provided care; dying patient care aspects; ethical issues; qualifications of self-, colleagues and institution professional practice; frequency of ethical dilemmas in care context and identification of barriers to optimal end-of-life care.
The questionnaire to know the opinion and perception that family members have about end-of-life care quality was designed with dichotomous questions, organized in five sections (sociodemographic data of the family caregiver; data referred to the deceased patient and his/her illness; symptoms control during the last month; information and support from health professionals and opinion about end-of-life care). The participating relatives were contacted by phone. Questionnaires were carried out at each participant's residence in a single meeting.
For both family and health professional questionnaires, an informed consent signed by the participants was obtained.
For data registration from medical records, a document designed to facilitate the collection of data that can be contrasted with those obtained from the other named sources was prepared, including sociodemographic and clinical variables, end-of-life medical decisions in the last 3 months of life of the patient, treatments/interventions carried out in the last 14 days, 7 days and 48 hours of life, identification of terminal clinical situation during the last 3 months of life and the prognostic factors related to this clinical situation. For selection and identification of medical records, one year data were requested from the hospital mortality records in relation to any of the aforementioned diseases that caused the death of the patients. Access to medical records was obtained after hospital authorization. Admission / discharge, medical and nursing clinical reports were reviewed.
Statistical analysis
SPSS statistical package (version 20.0 Inc., Chicago, IL) was used. Qualitative variables were described by frequency and quantitative variables by mean and standard deviation. Pearson's Chi-square test was used for inferential statistics. A p-value of ≤0.05 was considered to be statistically significant for all analyses. Quantitative results were organized by grouping the analyzed factors in the questionnaires according to the established categories, carrying out data transformation and integrating them into the defined categories.
In each category, the information obtained from each source was compared and convergent, complementary or divergent elements were established, as well as whether they were present or absent.
Ethical considerations
This research project was approved by the Ethics and Research Committee of the hospital. All personal data obtained in this study are confidential and have been treated in accordance with the Organic Law on Protection of Personal Data 15/99 and the Royal Decree 1720/2007 of 21 December, which approved the regulations for the development of this law.
RESULTS
Mean age of the family members who participated in the study was 57.2 ± 14.49 years, with a minimum age of 29 and a maximum of 83. Health professionals mean age was 42.4 ± 6.99 years, with a minimum of 28 and a maximum of 55; and the mean age of the deceased patients registered in the selected medical records was 76.5 ± 9.66 years, with a minimum of 52 and a maximum of 92.
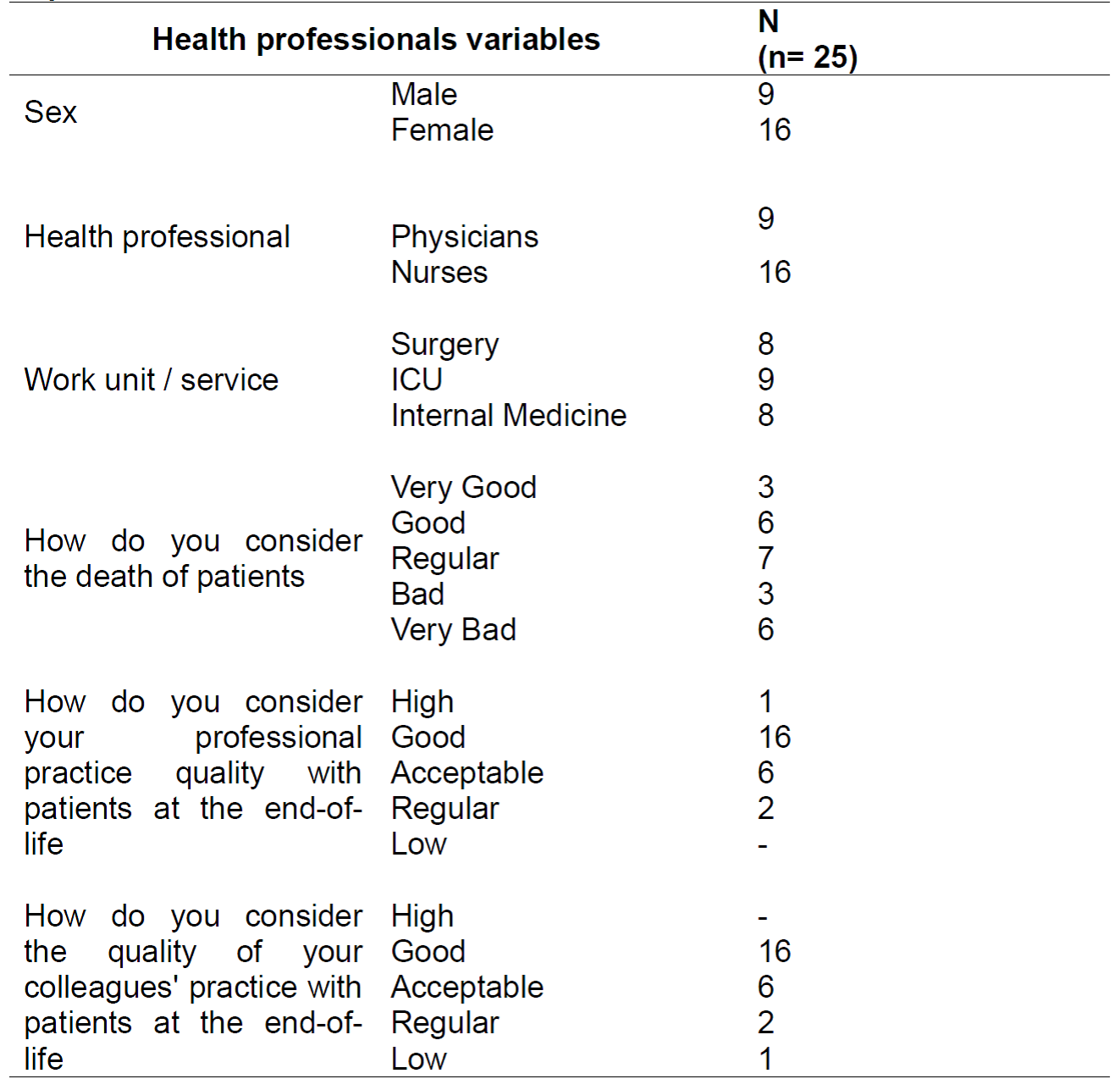
Remaining sociodemographic characteristics, as well as the results referring to health professionals and caregivers opinion, and data recorded in medical records are shown in Tables 1, 2 and 3.
Table 2. General data of health professionals and end-of-life care quality, Melilla, ME, Spain, 2019.
Regarding health care process characteristics, data analysis showed that in general, patients spend their last month of life in hospital, but even when they stay at home during that last month, end up dying in the hospital. In medical records, data concerning healthcare process, information/knowledge and decision-making were very scarce, and rarely organized or named for proper identification. To avoid interpretations and assumptions that could be understood as a result manipulation, it was decided to consider as absent all data that were not properly identified.
Healthcare process (Table 4)
Elements of this category in which significant differences were found between family members and health professionals were related to pain and other symptoms management. Health professionals mainly considered that the pain and symptoms were controlled most of the time, while relatives thought that it was only achieved sometimes. Family members and health professionals agreed in their positive evaluation in relation to the accompaniment of patients during the process and in their negative evaluation with respect to spiritual care. No information regarding healthcare process was found in medical records.
Table 4. Healthcare process, Melilla, ME, Spain, 2019.

(#)Not recorded on Medical Record (*)Family/Health professionals/medical records (**)Family/Health professionals
Information and Knowledge (Table 5)
With regard to the information and knowledge available to family and patient, very different results were obtained. 57.9% of family members considered that they were always or most of the time informed about diagnosis and prognosis. 40.0% of health professionals had the same opinion. However, this information was registered in only 31.6% of the medical records.
Table 5. Family/patient information and knowledge, Melilla, ME, Spain, 2019

(#)Not recorded on Medical Record (*)Family/Health professionals/medical records (**)Family/Health professionals
Decision-making
Comparative data from the different sources of information showed important discrepancies mainly between health professionals and family members. Family members considered in more than half of the cases (58.8%) that their opinion and that of the patient had been taken into account. However, health professionals stated in 45.8% of the cases that these opinions were not considered, as well as in medical records, in which this opinion was not recorded in 89.5%.
Concerning whether the patient made direct decisions, the answer was negative for all health professionals and for 89.5% of the family members. There was no data recorded in the medical records on this subject. In terms of decisions about specific measures such as the limitation of therapeutic effort (LTE) and the indication of No Cardiopulmonary Resuscitation (CPR), there was a significant difference of opinion over CPR. For 89.5% of the family members, there was no indication for non-resuscitation, while 52% of the health professionals thought that it was indicated. Data from medical records showed that this indication was recorded in only one case (5.3%). Regarding whether the place of death of the patient was the preferred one, 89.5% of family members and patients considered that it was not, while 68% of health professionals mentioned that it was. As for the decision of terminal sedation, 16.7% of the family members said that this option was available, compared to 32% of the health professionals who expressed the same opinion. There was no registration of this decision in the medical records.
DISCUSSION
Results show the lack of relevant data collected in medical records; in particular, it is not indicated whether the patient has advanced directives or has expressed preferences and wishes on how it would like the end-of-life process to be, which is consistent with other studies findings 18. Among the possible explanations found in the reviewed literature, we found lack of competence19, knowledge of legal requirements and lack of time20, information that is important to register in order to ensure patient safety21.
Another noTable finding has been the verification of healthcare quality at the end-of-life, which can be qualified as deficient if we consider indicators such as the number of hospitalizations in the last thirty days of life6. Our results show that all patients died in the hospital and that almost 3 out of 4 patients were admitted at least once during the month prior to death or had repeated hospitalizations, which seems to be related to a perception of a bad experience. However, data related to the intensity of the interventions are indicative of good quality of care.
Regarding the perception of relatives about the control of symptoms during the thirty days previous to the death of patients, other authors describe variability in satisfaction, specifically with the management of dyspnea. A higher level of dissatisfaction is also observed with general hospital care versus home care 22. This could not be found in our study since all patients died in the hospital.
Concerning the information and knowledge provided, discrepancies were observed. Health professionals had a worse opinion about the information given to the family members than the actual family members. This can be explained because perhaps for relatives it is enough to be aware of the severity of the situation without knowing about details that could disturb their emotional balance.
This result is consistent with the widespread situation in our country of the conspiracy of silence in palliative care and reality concealment requested by the family members7.
Finally, disparities in data related to decision-making, show a significant disagreement between the perceptions of health professionals and family members regarding the major subjects of decision, in addition to the deficient registration of all this in the medical records. Of note, all health professionals claim that patients are not directly involved in decision-making. This situation may explain other important aspects of disagreement, for example, the indication of non-resuscitation, or whether the patient died where he or she wanted, or the decision to administer terminal sedation. Disagreements in decision-making among health professionals has been an issue identified by other researchers. Moreover, the decision-making process and the preferences of the patient and the family will be determined by their beliefs, values and culture. The influence of these aspects must be taken into account as a critical element in the communication and experience of the end-of-life process 18,23.
The role of nursing is crucial in improving the perception of the care received. In other countries, nursing interventions are highly effective and include not only symptom monitoring, but also case coordination, symptom management education and therapeutic counseling, carried out mainly at the home of the patient or by telematics. These interventions generally include support and training of family members or primary caregivers 24. The results of this study suggest that nurse intervention, in case management, symptom control education and therapeutic counseling, is poor and can be improved. Therefore, aspects such as psychological support, training and information for patients and families should be emphasized and a planned intervention that include the aspects mentioned above should be offered as part of care led by nurses.
These results should be taken into account in the design and implementation of specific care plans that can also contribute to lower health costs.
As a limitation of this study we can point out that generalization of results would be premature given the sample size.
Given the cultural diversity of Melilla, we consider important for future research, to investigate about the satisfaction of spiritual needs from an intercultural approach since other studies have shown that it is an aspect that concerns the majority of patients 25.
It would also be interesting to study how certain factors affect the perception of quality of care. For example, the role of nursing, spiritual needs of the patient/family member or terminal illness type (oncological or not). And to explore the role of care levels, since palliative care management shows important differences between primary and specialized care 26.
CONCLUSIONS
This study provides an integrated view of the healthcare situation at the end-of-life provided at Melilla Hospital, showing priority areas of intervention, such as patient involvement in decision-making; issues that must be addressed to improve care in this process.
Contrasting information obtained from medical records, health professionals and family members showed divergences in fundamental aspects that contribute to improve satisfaction during the end-of-life period. It appears necessary to improve specific training of health professionals and to implement the completion of the medical records, including the process of informing patients and their families of the diagnosis and prognosis, in order to improve care during this stage.
Likewise, it is advisable to establish effective procedures to encourage patient and family participation in decision-making.
REFERENCIAS
1. Esteban M, Grau, IC, Castells G, Bullicg I, Busquet X, Aranzana A; et al. Complejidad asistencial en la atención al final de la vida: criterios y niveles de intervención en atención comunitaria de salud. Med. paliat. 2015; 22(2): 69-80. [ Links ]
2. Florêncio MM, Lopes de Almeida M C. The illness experience: Palliative care given the impossibility of healing. Rev. Esc. Enferm. USP. 2016; 50:7-53. [ Links ]
3. Donato CT, Matuoka Y, Yamashita C, Salvetti MG. Effects of dignity therapy on terminally ill patients: a systematic review. Rev. Esc. Enferm. USP. 2016;50(6):1011-1021. [ Links ]
4. Fascioli A. Los cuidados paliativos al final de la vida: Expresión del reconocimiento del otro. Enfermería (Montev.) . 2016; 5(2):46-53. [ Links ]
5. Sepúlveda JM, Morales JM, Morales IM, Canca JC, Crespillo E, Timonet E. El derecho a morir con dignidad en un hospital de agudos: un estudio cualitativo. Enferm. clín. (Ed. Impr.). 2014; 24(4): 211-218. [ Links ]
6. Lima JS, Asensio MR, Palomo JC Ramírez EB, Lima M. Razones para decidir morir en el hospital o en el domicilio. Visión de los/las profesionales. Gac. Sanit. (Barc., Ed. Impr.). 2018; 32(4): 362-368. [ Links ]
7. Lozano B, Huertas MM. Cuidados paliativos, cuidados compartidos. Cult. cuid. 2018; 49: 100-107. [ Links ]
8. Esteban M, Fernández J, Boira RM, Martínez T, Nadal S, Castell G. Concordancia entre la complejidad observada desde diferentes niveles asistenciales en pacientes crónicos complejos, con enfermedad avanzada o al final de la vida mediante un modelo de abordaje de la complejidad. Med. paliat. 2018; 4: 236-244. [ Links ]
9. García MT, Gil E, Fernández MC, Sanz EM, Dones M, Domínguez A, et al. Programa centralizado de formación en Cuidados Paliativos. Coordinación Regional de la Comunidad de Madrid 2010-2015. Educ. med. (Ed. Impr.). 2017; 18(2): 103-113. [ Links ]
10. Rodríguez I, Villamor A, Lahosa MT, Dorca M, Mas M, Salvador MI. Conocimientos y actitudes de enfermeras de onco-hematología ante el documento de voluntades anticipadas. Rev. cuba. enferm. 2018; 34(2): 1-15 [ Links ]
11. Pascual MC. Información a familiares de pacientes en proceso final de vida en unidades de cuidados intensivos. Evaluación por parte de las enfermeras. Enferm. clín. (Ed. Impr.). 2014; 24(3):168-174. [ Links ]
12. Sánchez MR, Moreno M, Hueso C, Campos C, Varella A, Montoya R. Dificultades y factores favorables para la atención al final de la vida en residencias de ancianos: un estudio con grupos focales. Aten. prim. (Barc., Ed. Impr.). 2017; 49(5): 278-285. [ Links ]
13. Velarde JF, Luengo R, González R, González S, Álvarez B, Palacios D. Dificultades para ofrecer cuidados al final de la vida en las unidades de cuidados intensivos. La perspectiva de enfermería. Gac. Sanit. (Barc., Ed. Impr.). 2017; 31(4):299-304 [ Links ]
14. Puerto HM. Calidad de vida en cuidadores familiares de personas en tratamiento contra el cáncer. Rev. cuid. (Bucaramenga. 2010). 2015; 6(2): 1029-1040. [ Links ]
15. Instituto Nacional de Estadística. Cifras oficiales de población resultantes de la revisión del Padrón municipal a 1 de enero [Internet]. INE; 2017 [citado 2018 mar. 1]. Disponible en: https://www.ine.es/jaxiT3/Datos.htm?t=2915 [ Links ]
16. Guerrero RF, Prado M, Ojeda MG. Reflexión crítica epistemológica sobre métodos mixtos en investigación de enfermería. Enferm. univ. 2016; 13(4): 246-252. [ Links ]
17. Alzás T, García LM. La evolución del concepto de triangulación en la investigación social. Rev Pesqui Qualit. 2017; 5(8): 395-418. [ Links ]
18. Sepúlveda JM, Morales JM, Morales IM, Sánchez JC, Timonet EM, Rivas F. Análisis de la toma de decisiones compartidas al final de la vida en las historias clínicas. Med. paliat. 2017; 24(1):14-20. [ Links ]
19. Kreetapirom P, Jaruratanasirikul S, Pruphetkaew N. Audit of paediatric residents' medical records. Clin Teach. 2017; 14(3): 189-194. [ Links ]
20. López JJ, Moreno MG, Saavedra CH, Espinosa AL, Camacho JU. La importancia del registro clínico de enfermería: un acercamiento cualitativo. Nure Investigación. 2018; 15(93): 1-9. [ Links ]
21. Dy SM. Patient safety and end-of-life care: common issues, perspectives, and strategies for improving care. Am Hosp Care. 2016;33(8): 791-796. [ Links ]
22. Burge F, Lawson B, Asada Y, Mclntyre PF, Grufeld E, Flowerdew G. Bereaved family member perceptions of patient-focused family-centred care during the last 30 days of life using a mortality follow-back survey: does location matter?. BMC Palliat Care. 2014; 13:25 [ Links ]
23. Manalo MF. End-of-Life Decisions about Withholding or Withdrawing Therapy: Medical, ethical, and Religio-cultural considerations. Palliat Care. 2013; 7: 1-5 [ Links ]
24. Van Der Eerden M, Csikos A, Busa A, Hughes S, Radbruch L, Menten J, et al. Experiences of patients, family and professional caregivers with Integrated Palliative Care in Europe: protocol for an international, multicenter, prospective, mixed method study. BMC Palliat Care. 2014; 13:52. DOI: https://doi.org/10.1186/1472-684X-13-52 [ Links ]
25. Singer AE, Goebel JR, Kim YS, Dy SM, Ahluwalia SC, Clifford M, et al. Populations and interventions for palliative and end-of-life care: a systematic review. J Palliat Med. 2016; 9(9): 995-1008. [ Links ]
26. Otte IC, Jung C. Bally K, Elger BS, Schildmann J. Interprofessional Silence at the End of Life: Do Swiss General Practitioners and Hospital Physicians Sufficiently Share Information About Their Patients?. J Palliat Med. 2016; 19(9): 983-986. [ Links ]
Received: May 19, 2020; Accepted: December 21, 2020











 text in
text in 




