My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Enfermería Global
On-line version ISSN 1695-6141
Enferm. glob. vol.20 n.64 Murcia Oct. 2021 Epub Oct 25, 2021
https://dx.doi.org/10.6018/eglobal.465261
Originals
Nursing triage in acute stroke
1. Graduada en Enfermería. Servicio de Urgencias. Hospital Universitario de Salamanca. Profesora Asociada. Facultad de Enfermería y Fisioterapia. Universidad de Salamanca. España. arvico@usal.es
2 .Médico Urgenciólogo. Profesor Titular de Universidad. Facultad de Enfermería y Fisioterapia. Universidad de Salamanca. España.
In recent decades, the role of nursing in triage and screening of patients in emergency services, both in prehospital environment and especially in hospitals, is essential and indisputable. In order to analyze the triage carried out by nursing to detect patients with acute stroke, and if necessary improve it, a retrospective study was carried out of the cardinal presentations of stroke, the scale of the National Institute of Health of the United States, and the modified Rankin scale, applied in the nursing triage set at the Salamanca University Hospital, during the period between 2016 and 2019, both inclusive. The total number of clinical records analyzed was 1572. The analysis is focused on the reliability, evaluated by nursing, of the cardinal presentations of acute stroke, and of the two scales, compared to the traditional rapid algorithms for stroke detection, in particular the FAST method, and the Cincinnati scale. Our study shows that there are several clinical presentations that escape the rapid scales, so it is essential to expand the triage methods of acute stroke carried out by nursing, in order to avoid delays in detection and definitive treatment (time-dependent disease). Thus, the expanded identification of cardinal presentations, together with the use of more detailed scales applied by trained nurses, appear to be very useful tools for the detection of acute stroke.
Key words: Stroke; triage; cardinal presentation; nursing
INTRODUCTION
Triage is the first contact of the patient, the family, and the caregivers, with the health professional, both at the pre-hospital and hospital levels1. Triage methods are rapid scales and protocols intended to classify and prioritize patients in need of urgent care. Morbidity and mortality can be prevented if patients are quickly classified and treated efficiently, since many deaths occur within the first hours of admission2. With a precise triage system, carried out by trained people, and with adequate algorithms, the incidence of adverse events decreases significantly, especially in time-dependent diseases. If the triage is well carried out by appropriate health professionals, it is a key tool in the classification and prioritization of emergency treatment in the hospital setting, as well as in the criteria for pre-hospital and inter-hospital emergency transport3,4.
In most hospital triage areas, the nurse is the first clinically trained health professional who will assess the clinical situation of patients. He must detect the most important clinical data, and decide if the patient should be treated immediately, or if the pathology is not dangerous to life, and can wait a reasonable time. Therefore, its main objective is that patients can be, as soon as possible, selected, classified, treated, or discharged in a timely manner4)(5)(6.
Considered as blue codes, time-dependent pathologies, such as acute stroke, acute coronary syndrome, or severe trauma, cannot be delayed under any circumstances, and must be discovered immediately through correct triage. Acute stroke is a serious, life-threatening clinical emergency condition that requires immediate detection and treatment (the faster treatment is received, the less harm and injury the patient suffers). Patients with acute stroke are therefore usually evaluated for the first time in hospitals, by nurses responsible for the triage area. Different studies have clearly demonstrated the effectiveness of triage protocols for this pathology in reducing the time from the patient entering the hospital to the final specific treatment 7,8.
For many years now, different methods have been used to correctly triage stroke, both at the pre-hospital and hospital level. The FAST (Face/Arm/Speech/Time) and FASTER (Face/Arm/Stability/Eyes/React) methods and the Cincinnati scale (Facial droop/Arm drift/Speech) are three of the most common. However, these simple methods may be totally insufficient in a nursing triage area 9)(10)(11)(12 with a potential risk of error and delay in diagnosis, when the cardinal presentation is not so typical to be framed in these methods.
Based on the above, the objective of the present study is to carry out a retrospective analysis of the cardinal presentations of acute stroke detected in the hospital triage area by the nursing professional, together with the immediate application of the NIHSS13 (National Institute of Health Stroke Scale) and MRS14 (Modified Rankin Scale) scales, at the University Hospital of Salamanca, during the period between 2016 and 2019.
MATERIAL AND METHODS
In this study we have analyzed a total of 2080 medical records of patients with confirmed acute stroke. The patients correspond to the area of influence of the Salamanca University Hospital (including the 112 Emergency Service), during the period from 2016 to 2019, both inclusive. The information of the patients was obtained from the medical records under the strict control and supervision of the Documentation Service of the University Hospital of Salamanca. Data management was carried out under the rules of the Ethics Committee for the use of the information collected in the patients' medical records.
Three groups of data were analyzed: the cardinal presentations, and the NIHSS and MRS scales. Some clinical records did not contain all the data under study or were not clearly specified. When it affected two of them, they were discarded. Most of the time they were due to the absence of the NIHSS score along with the MRS. Thus, the final number of stories analyzed in the four years was 1572 (2016: 375. 2017: 371. 2018: 421. 2019: 405.)
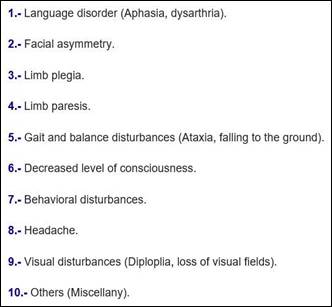
The cardinal presentations were divided into ten different groups, in order to have an easy to apply, but expanded method of detecting possible presentations, both typical and less frequent, as shown in Table 1.
The NIHSS scale was always performed after rapid triage of cardinal presentations, during the period in the emergency department prior to computed tomography. NIHSS includes different items, as specified in Table 2. Each item is scored from 0 to 2, 0 to 3, or 0 to 4 points. The total score ranges from 0 to 42 (the higher the score, the more severe the stroke). The original NIHSS13 scale (Table 2) has been applied to our study, as it is the most widely used, although there are several versions available (NIHSS with 5, 8 and 11 items).
MRS14 is a 6-point disability scale with possible scores ranging from 0 to 5. Typically, a separate category is added for patients who die (6). Although there are different versions of the Rankin scale, for our study we have used the most widely used modified version in emergency departments and neurology (Table 3).
RESULTS
In the distribution by gender, we found a slight predominance of male patients (871), compared to female (701), which represents 55.40%, compared to 44.60%. A total of 70 patients were in the group under 50 years of age. The group with the highest number was that of 50 to 80 years with a total of 908, with 594 patients being within the group of more than 80 years. In percentage they represent 4.46%, 57.76% and 37.78% respectively.
Analyzing the cardinal presentations (Image 1), the clinical data with the highest expression were language disorders with a total of 285 patients (18.13%). The way of describing them by relatives and caregivers was very diverse, including expressions such as "He does not speak", "It is difficult for him to speak", "He is not understood", and "He speaks strangely".
In the ataxia group all gait disturbances / difficulties were included, as well as falls, both at home and on public roads. A total of 240 patients (15.26%) presented this cardinal presentation.
Paresis (231, 14.69%) and plejia (189, 12.02%), ranked fourth and fifth respectively. They were referred to as "Difficulty moving a limb", "Weakness of a limb", "Not moving a limb", etc.
Facial asymmetry, accounted for a total of 139 cases (8.84%). Referred to in a very typical way with expressions such as "His mouth has been twisted" or "One side of his mouth has fallen off".
Behavioral alteration was the cardinal presentation in 7.44% of all cases, assuming 117 patients in absolute numbers. It should be noted that although in some cases the behavior modification was evident, in others it was subtle changes, often habit changes, sudden changes in character, even mood effects.
Headache, be it holocranial, hemicranial or regional, stood out as the onset in 56 cases (3.56%). It was observed in several cases, after imaging diagnosis, that the location of the pain referred by the patient had a clear relationship with the affected vascular territory. The least frequent cardinal presentation detected in this study was ocular alterations with a total of 31 cases (1.97%). The most frequent clinical finding in this group was diplopia.
Finally, in some histories the onset symptoms were not clearly defined, or presented other forms, corresponding more to other underlying pathologies or epiphenomena, than to clinical data related to stroke.
Considering the NIHSS scale, the most important number of patients was in the range between 12-15 points, with a total of 474 cases (30.15%), closely followed by the range between 16-20 points, with a total of 435 patients (27.67%).
87 patients (24.62%) were located in the group between 7 and 11 points, while 186 (11.83) were located in the area with the highest score, above 20 points. With less than 7 points, a total of 36 patients (2.29%) and the group of histories in which the NIHSS were not explicitly recorded at the beginning of the image (64, 4.07%).
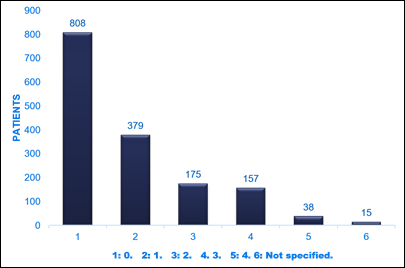
Finally, analyzing the MRS, the most important group of patients presented 0 points, being a total of 808 (51.40%), which indicates that their previous baseline status allowed them to be valid for all possible activities of daily life.
The next two groups with the highest number of patients were those with a score of 1 (379, 24.11%) or 2 points (11.13%). 157 patients (9.99%) had a total of 3 points at the time of stroke diagnosis and 38 patients (2417%) added 4 points.
It should be noted that there were no cases of patients with 5 or 6 points, which is totally logical given that it would mean a previous maximum disability (5 points) or a previous death (6 points) and that in 15 patients (0.95%), MRS was not indicated.
DISCUSSION
Classification and triage by nurses and other health professionals, both at the prehospital and hospital level, is a complicated method/technique, as it is sometimes performed in a difficult and adverse environment. The emergency services are often overwhelmed by the huge number of patients demanding clinical care as quickly as possible. In response to these special conditions, many studies have demonstrated the efficiency of the nursing triage process. Nursing triage is an effective intervention to detect life-threatening diseases, especially time-dependent ones. In a triage environment, nurses must manage appropriate algorithms/scales to detect these dangerous states of patients15)(16)(17)(18)(19.
Acute stroke is the second leading cause of death worldwide and one of the leading causes of disability, with an increasing incidence in developed countries. Ischemic stroke caused by arterial occlusion is responsible for most cerebrovascular accidents (more than 70%). Since it is a time-dependent situation, the correct management must include a rapid and precise triage and diagnosis, to achieve, if necessary, reperfusion of the ischemic brain area with intravenous thrombolysis and / or endovascular thrombectomy20.
Simple traditional stroke triage methods are useful tools to easily detect acute stroke (very few item scales). They include the FAST and FASTER algorithms, and some scales such as the Cincinnati scale. They are widely used especially by pre-hospital emergency services, as they are easy and quick to learn or perform and have a good ability to identify potential stroke patients. However, it only evaluates the presence of some symptoms (facial paralysis, upper limb weakness and speech disturbances), but does not evaluate other less frequent cardinal presentations, and the severity of the stroke21. Therefore, the use of scales and methods with greater sensitivity in the detection of patients with acute stroke in triage sets becomes essential.
The NIHSS scale is a systematic evaluation tool, valid for detecting acute stroke, measuring its severity, guiding the appropriate treatment, and predicting the patient's outcome13. Furthermore, it provides a common language for the exchange of information among healthcare professionals. The NIHSS scale is quick and easy to administer by trained professionals (5-7 minutes) and requires minimal equipment. There are much more complex methods to handle large volumes of different clinical data, but they are not suitable for use in triage emergency services due to their complexity22,23) being reserved more for intensive care units.
The MRS scale is frequently used in acute strokes to detect the patient's previous state and the later state at the time of leaving the hospital, but also to select which patients should or should not be treated. It is a coded scale from 0 (no symptoms) to 5 (severe disability) and 6 (death). The MRS scale in stroke/triage trials can divide patients into two groups: Scores from 0 to 2/3 are positive for specific treatments such as endovascular (if they meet the rest of the requirements). However, the rest of the scores (>3) are defined as negative for this type of treatment. A limitation of this scale has been the subjective determination between categories and the reproducibility of the score by examiners and patients.
As observed in our study through the analysis of cardinal presentation, there are multiple forms of presentation of acute stroke. Several of them, the most frequent, would be easily framed and detectable, using the traditional FAST/FASTER methods and the Cincinnati scale, but other presentations clearly escape these rules. Presentations such as decreased level of consciousness (15.84%), behavioral disturbances (7.40%), headache (3.56%), and ocular disturbances (1.90%) are not considered in them and represent a total of 27% of the presentations. If they are considered, it may be that they delay the diagnosis, escaping the initial detection in a triage room, with the serious consequences that this can have.
In other words, more than 25% of strokes may go undetected in the triage room if simple and excessively rapid triage scales are followed. Therefore, the use of extended cardinal presentation triage schemes should be an essential tool, as shown in Table 1. In this sense, the use of more complete scales such us NIHSS by trained nurses becomes essential. Along with this, as an essential complement to rapid screening for immediate treatment, the application of the MRS scale should be required in the triage area as a key tool for the selection of patients who should receive immediate treatment and which should not.
Thus, the experience and skills of nursing professionals24)(25)(26)(27, the combination of a selective search for cardinal presentations with a selected group of symptoms, together with the NIHSS and MRS scales, constitute useful tools for screening and the correct diagnosis of acute stroke. The key role of nursing professionals becomes fundamental in the present and in the immediate future of hospital triage, and must be considered in all emergency services.
CONCLUSIONS
In the light of our results, the specific role that nursing plays in the triage room in general, and in the detection of time-dependent diseases, with special mention of acute stroke, is crucial. Given that more than 25% of acute stroke presentations are not typical, the nursing professionals should reinforce their specific training in the extended triage scales and less frequent presentations of this time-dependent disease.
REFERENCIAS
1. Wolf LA, Delao AM, Perhats C, Moon MD, Zavotsky KE. Triaging the Emergency Department, Not the Patient: United States Emergency Nurses' Experience of the Triage Process. J Emerg Nurs. 2018; 44(3): 258-66. DOI: 10.1016/j.jen.2017.06.010. [ Links ]
2. Bazyar J, Farrokhi M, Salari A, Khankeh HR. The principles of triage in emergencies and disasters: a systematic review. Prehosp Disaster Med. 2020; 35(3): 305-313. DOI: 10.1017/S1049023X20000291. [ Links ]
3. P. Funderburke, P. Exploring best practice for triage. J Emerg Nurs. 2008; 34(2): 180-182. DOI: 10.1016/j.jen.2007.11.013. [ Links ]
4. Haghigh S, Ashrafizadeh H, Mojaddami F, Kord B. A survey on knowledge level of the nurses about hospital Triage. J Nurs Educ. 2017; 5 (6): 46-52. DOI: 10.21859/jne-05067. [ Links ]
5. Magnusson C, Herlitz J, Axelsson C. Affiliations expand Pre-hospital triage performance and emergency medical services nurse's field assessment in an unselected patient population attended to by the emergency medical services: a prospective observational study. Scand J Trauma Resusc Emerg Med. 2020; 28(1): 81. DOI: 10.1186/s13049-020-00766-1. [ Links ]
6. Reisi Z, Saberipour B, Adienh M, Hemmatipour A, Shahvali E.A. The level of awareness of the emergency department nurses of the triage principles in teaching hospitals. J of Nurs Mid Sci. 2018; 5 (1): 32-37. DOI: 10.4103/JNMS.JNMS_5_18 [ Links ]
7. William J. Powers, Alejandro A. Rabinstein, Teri Ackerson, Opeolu M. Adeoye, Nicholas C. Bambakidis, Kyra Becker, José Biller, Michael Brown, Bart M. Demaerschalk, Brian Hoh, Edward C. Jauch, Chelsea S. Kidwell, Thabele M. Leslie-Mazwi, Bruce Ovbiagele, Phillip A. Scott, Kevin N. Sheth, Andrew M. Southerland, Deborah V. Summers, and David L. Tirschwell and on behalf of the American Heart Association Stroke Council. 2018 Guidelines for the Early Management of Patients With Acute Ischemic Stroke: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke. 2018; 49: e46-e99. DOI: 10.1161/STR.0000000000000158. [ Links ]
8. Ekundayo OJ, Saver JL, Fonarow GC, Schwamm LH, Xian Y, Zhao X, Hernandez AF, Peterson ED, Cheng EM. Patterns of emergency medical services use and its association with timely stroke treatment: findings from Get With The Guidelines-Stroke. Circ Cardiovasc Qual Outcomes. 2013; 6: 262-269. DOI: 10.1161/CIRCOUTCOMES.113.000089. [ Links ]
9. BE-FAST (Balance, Eyes, Face, Arm, Speech, Time) Reducing the Proportion of Strokes Missed Using the FAST Mnemonic Aroor SS, Singh R, Goldstein LB, Stroke. 2017; 48: 479-481. DOI: 10.1161/STROKEAHA.116.015169. [ Links ]
10. Rudd M, Buck D, Ford GA, Price CI. A systematic review of stroke recognition instruments in hospital and prehospital settings. Emerg Med J, 2016; 33(11): 818-822. DOI: 10.1136/emermed-2015-205197. [ Links ]
11. Schlemm E, Ebinger M, Nolte CH, Endres M, Schlemm L. Optimal transport destination for ischemic stroke patients with unknown vessel status: use of prehospital triage scores. Stroke. 2017; 48: 2184-2191. DOI: 10.1161/STROKEAHA.117.017281. [ Links ]
12. Venema E, Lingsma HF, Chalos V, Mulder M, Lahr MMH, van der Lugt A, van Es A, Steyerberg EW, Hunink MGM, Dippel DWJ, Rozemberg B. Personalized prehospital triage in acute ischemic stroke. Stroke. 2019; 50: 313-320. DOI: 10.1161/STROKEAHA.118.022562. [ Links ]
13. Williams LS, Yilmaz EY, Lopez-Yunez AM. Retrospective Assessment of Initial Stroke Severity with the NIH Stroke Scale Stroke. 2000; 31: 858-862. DOI: 10.1161/01.STR.31.4.858 [ Links ]
14. Banks JL, and Marotta CA. Outcomes Validity and Reliability of the Modified Rankin Scale: Implications for Stroke Clinical Trials A Literature Review and Synthesis. Stroke. 2007; 38: 1091-1096. DOI/10.1161/01.STR.0000258355.23810.c6. [ Links ]
15. Stanfield LM. Clinical decision making in triage: an integrative review. J Emerg Nurs. 2015; 41(5): 396-403. DOI: 10.1016/j.jen.2015.02.003. [ Links ]
16. Delmas, P, Fiorentino A, Antonini M, Vuilleumier S, Stotzer G, Kollbrunner A, Jaccard D, Hulas J, Rutschmann O, Simon J, Hugli O, Keranflec'h CG, Pasquier J. Effects of environmental distractors on nurse emergency triage accuracy: a pilot study protocol. Pilot Feasibility Stud. 2020 6: 171. DOI: 10.1186/s40814-020-00717-8 [ Links ]
17. Chen SS, Chen JC, Ng CJ, Chen PL, Lee PH, Chang WY. Factors that influence the accuracy of triage nurses' judgement in emergency departments. Emerg Med J. 2010; 27(6): 451-455. DOI: 10.1136/emj.2008.059311. [ Links ]
18. Mistry B, Stewart De Ramirez S, Kelen G, PSK S, Balhara KS, Levin S, et al. Accuracy and Reliability of Emergency Department Triage Using the Emergency Severity Index: An International Multicenter Assessment. Ann Emerg Med. 2018; 71(5): 581-7.e3. DOI: 10.1016/j.annemergmed.2017.09.036. [ Links ]
19. Martin A, Davidson CL, Panik A, Buckenmyer C, Delpais P, Ortiz M. An examination of ESI triage scoring accuracy in relationship to ED nursing attitudes and experience. J Emerg Nurs. 2014; 40(5): 461-468. DOI: 10.1016/j.jen.2013.09.009. [ Links ]
20. Smith EE, Kent DM, Bulsara KR, Leung LY, Lichtman JH, Reeves MJ, Towfighi A, Whiteley WN, Zahuranec D. Accuracy of prediction instruments for diagnosing large vessel occlusion in individuals with suspected stroke: a systematic review for the 2018 guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2018; 49: e111-e122. DOI: 10.1161/STR. 0000000000000160. [ Links ]
21. Berglund A, Svensson L, Wahlgren N, von Euler M; HASTA Collaborators. Face Arm Speech Time Test use in the prehospital setting, better in the ambulance than in the emergency medical communication center. Cerebrovasc Dis. 2014; 37: 212-216. DOI: 10.1159/000358116. [ Links ]
22. Sánchez F, Ballesteros, JC, Kraiem MS, Sánchez M, Moreno MN. Using Ensembles and a Clustering-Based Undersampling Approach", Appl. Sci. 2019; 9: 5287. DOI: 10.3390/app9245287 [ Links ]
23. González, J., Martín, F., Sánchez, M., Sánchez, F. and Moreno M.N. "Multiclassifier systems for predicting neurological outcome of patients with severe trauma and polytrauma in intensive care units". J Med Syst. 2017; 41:136, DOI: 10.1007/s10916-017-0789-1. [ Links ]
24. Reay G, MacDonald LS, Then KL, Hall M, Rankin JA. Triage emergency nurse decision-making: Incidental findings from a focus group study. Int Emerg. 2020; 48: 100791. DOI: 10.1016/j.ienj.2019.100791. [ Links ]
25. Levin S, Toerper M, Hamrock E, Hinson JS, Barnes S, Gardner H, et al. Machine-Learning-Based Electronic triage more accurately differentiates patients with respect to clinical outcomes compared with the emergency severity index. An Emerg Med. 2018; 71(5): 565-74.e2. DOI: 10.1016/j.annemergmed.2017.08.005. [ Links ]
26. Brosinski CM, Riddell AJ, Valdez S. Improving triage accuracy: a staff development approach. Clin Nurse Spec. 2017; 31(3): 145-148. DOI: 10.1097/NUR.0000000000000291. [ Links ]
27. Martin A, Davidson CL, Panik A, Buckenmyer C, Delpais P, Ortiz M. An examination of ESI triage scoring accuracy in relationship to ED nursing attitudes and experience. J Emerg Nurs. 2014; 40(5): 461-468. DOI: 10.1016/j.jen.2013.09.009. [ Links ]
Received: January 30, 2021; Accepted: May 31, 2021











 text in
text in