Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Enfermería Global
versión On-line ISSN 1695-6141
Enferm. glob. vol.20 no.64 Murcia oct. 2021 Epub 25-Oct-2021
https://dx.doi.org/10.6018/eglobal.459491
Originals
Parental stress scale in the neonatology unit: Statistical validation for the portuguese population
1. RN, Servicio de Neonatología del Hospital de Santa Maria, Centro Hospitalario y Universitario de Lisboa Norte, EPE; MSc, Especialista en Enfermería de Salud Infantil y Pediatría. CIDNUR - Centro de Investigación, Innovación y Desarrollo en Enfermería de Lisboa . Portugal. fatimasousa@campus.esel.pt
2. RN, MSc, PhD, Profesora Coordinadora, Escuela Superior de Enfermería de Lisboa. CIDNUR - Centro de Investigación, Innovación y Desarrollo en Enfermería de Lisboa . Portugal.
Objective:
To translate the Neonatal Unit Parental Stress scale into Portuguese and culturally and linguistically adapt it for Portugal, and to evaluate the psychometric qualities of the Neonatal Unit Parental Stress Assessment Scale - Modified Version (EASPUN-MV).
Method:
This was a quantitative methodological study to validate the Neonatal Unit Parental Stress Assessment Scale. Parents were selected by non-probabilistic sampling (n = 406 parents). Descriptive statistics, standardized Cronbach's alpha, and confirmatory factor analysis were used to calculate the sensitivity, validity, and reliability of the Neonatology Unit Parental Stress Assessment Scale (indexes of the model's goodness of fit χ2/df, CFI, TLI, RMSEA, P(RMSEA).
Results:
The empirical indexes of the EASPUN-MV’s factorial model showed accepTable goodness of fit (χ2/df=3.3; CFI=0.8; GFI=0.8; TLI=0.8 and P(RMSEA)=0.07).
Conclusion:
The Neonatology Unit Parental Stress Assessment Scale - Modified Version is a psychometrically sensitive, valid and reliable instrument that can systematically assess parental stress and facilitate the decision-making of nurses, the follow-up care of parents, and their referral to other healthcare professionals.
Keywords: Validation Study; Psychological Distress; Infant, Newborn; Neonatology; Parents; Nursing Care
INTRODUCTION
Parenting is one of the main roles in adult life and it begins during pregnancy, when mothers and fathers construct images, develop expectations, idealize their babies, and project the future. It is an expected transition in the family life cycle that no book can teach, only experience, and it represents a source of predicTable stress, which stimulates adaptation to the parental role and to the new family system. However, a premature or pathological birth and newborn admission into the neonatal intensive care unit (NICU) is, in most cases, an unexpected event that represents a source of stress for parents (1)(2)(3)(4.
The experience of having a child admitted to the NICU exposes parents to different stressors: intrapersonal, interpersonal and extrapersonal. These can be caused by the aggressive environment of this unit1)(5)(6) and the fragility of the infants, who require complex care suiTable to their condition. But other stressors could be parents' perception of their inability to care for their child7,8 and to protect them from pain and from procedures9,10; difficulty in transitioning into parenthood due to the change in their parental role; and uncertainty regarding the infant’s illness, hospital stay, and prognosis. Parents suffer negative psychological effects, experience an interruption in the development of the bonding and attachment process, and feel like they are failing in their parental role. The experience of parents in the NICU can prevent them from becoming emotionally attached to their child; thus, NICU admissions are recognized as potentially traumatic for parents11.
Parental stress levels are associated with hospitalization the severity of the infant’s disease, especially in the first days, and some responses displayed by parents include anxiety, helplessness, fear, guilt, shame, depression, sadness and disappointment, feeling loss of control over what is happening to them, and uncertainty about their ability to cope with daily parental tasks12,13. Families experience moments of uncertainty regarding the future of their newborns, and their own future, and have to face new demands and adaptations, given that NICU admission affects various spheres of life, such as the personal, financial, occupational and social dimensions14.
The need to understand how parents respond to stress in the NICU has led to the construction of models that conceptualize parental stress. These models recognize the presence of determinants that influence how parents experience the demands of parenthood. Some of these determinants may be multifactorial in origin, such as the personal characteristics of parents and their prenatal and perinatal experiences and the severity of the newborn's illness. Other factors may include perceived uncertainty, concerns related to prognosis, loss of the parental role, and personal resources available to the parents, such as family and financial support15,16.
To better understand stressors in the NICU, the scientific literature has developed two scales exclusively for this context, the Parental Stress Scale: Neonatal Intensive Care Unit (PSS: NICU)2)(17)(18) and the Neonatal Unit Parental Stress (NUPS) scale19,20. The use of parental stress assessment scales in NICUs has shown that sources of stress include how infants look and behave, treatments to which they are submitted, how easily parents development attachment to their newborns, parental role alterations, the sights and sounds of the NICU, and relationships with health professionals15)(19)(21) . The Neonatal Unit Parental Stress (NUPS) scale was created after the statistical validation of the PSS:NICU for the population of the United Kingdom and its subsequent cultural adaptation. Some authors reviewed various items and suggested the construction of a new dimension related to the birth experience, practical strains and pressures, and the transition into the parental role, and then proposed the design of the new scale. According to its authors, the new scale presented good internal reliability and construct validity. When used with mothers and fathers within the first two weeks of their NICU experience, it discriminated between different domains of stress, and identified a relationship between perceived family support and social/practical stress. Parents are the first regulators of their children and they play a decisive role in their children's development and future5,22. Given this reality, it is important that health professionals, especially nurses, adopt a collaborative care philosophy that is non-traumatic and family-centered, and that they develop anticipatory care that promotes transition into the parental role.
The use of an instrument to assess parental stress in the NICU allows for consistency of nursing care and implementation of infant- and family-centered care, promotes parenting, and increases the visibility of the nursing staff.
OBJECTIVE
The objective of this study was to carry out the translation, cultural and linguistic adaptation, and psychometric evaluation of the Neonatal Unit Parental Stress (NUPS) scale into Portuguese and for the Portuguese population, ensuring the validity and reliability of its construction.
METHOD
This was a quantitative methodological study to validate the Neonatal Unit Parental Stress Assessment Scale - Modified Version (EASPUN-MV). The process of translating the NUPS scale into Portuguese and adapting it to the cultural context of Portugal was authorized by the original creator of the scale, Tilly Reid, and was supported by the revised recommendations of the Cross-Cultural Adaptation of Health-Related Quality of Life Measures23. The translation of the original English version into Portuguese was carried out by two translators: A (professional translator, Portuguese, bilingual, with knowledge in the area of study); and B (Portuguese, bilingual, with knowledge about the study and in the area of health and psychometrics), resulting in two versions of the scale. After analyzing the two versions and their backtranslations, differences were analyzed, and any necessary adjustments were made before submitting the instrument to an expert panel. The final assessment resulted in the Neonatal Unit Parental Stress Assessment Scale - Modified Version (EASPUN-MV).
The study was conducted in seven NICUs in the public and private sector in the greater Porto area and in Lisbon and Vale do Tejo. Data collection took place between July 2019 and May 2020. The study was approved by the Administration Councils and Ethics and Data Protection Committees of the institutions involved, all the parents who participated in the study signed free and informed consent forms.
Instrument
The original NUPS scale, developed in the UK by Tilly Reid et al., consists of 65 items on which parents rate their experience with NICU stressors on a scale from 1 to 5, where 1 is ‘not at all stressful’ and 5 is “extremely stressful’, and zero (0) means that the parents have not had that experience. The items are distributed into 4 dimensions: the Physical Environment and Sounds (AFS) with 9 items; Infant Look, Behavior and Treatment (ACBT), with 15 items, Parent’s Relationship with Infant and Parental Role (RBPP), with 23 items; and Family and Social Relationship (RFS), with 18 items. Parents completed the scale within the first 96 hours of the infant's admission to assess levels of parental stress. The EASPUN-MV was given to parents 48 to 72 hours after birth and they were asked to return it the following day. The instrument was given to the parents, preferably by the infant’s reference nurse, who had been informed about the purpose of the study and application of the scale during the data collection period. A sociodemographic questionnaire was also administered (age, sex, level of education, prior experience in the NICU, type of birth, and data related to the newborn such as gestation at birth and weight).
Participants
The study used a non-probability, accidental, casual or convenience sample24, where all parents of newborns admitted to NICU during the data collection period were considered eligible. Only in cases with terminally ill infants, where social services were involved, with severe maternal illness, or where neither parent spoke nor understood Portuguese were the participants excluded.
A total of 406 (n=406) parents of newborns admitted to NICU participated in the study, with the goal of reaching a minimum of 5 observations per item to guarantee variability to estimate model parameters25)(26)(27. Of the parents who participated in the study, 66% (65.8) were female and 34% were male (34.2). The minimum age was 18 years old and the maximum, 51 years old, with an average of 32 (32.45), and a standard deviation of 5 years (5.24). Most parents had a basic education (55.7%), most with 12 years of schooling (37.7%), followed by 9 years (15.5%), 6 years (1.5%), and 4 years (1%). Of those with higher education (44.3%), 33% had an undergraduate degree and 11.3% had a master's degree. For most parents, that was their first experience with the NICU (93%), while only 7% had already gone through that experience. Only 21% of mothers had had natural vaginal deliveries, while the other 79% had obstructed births (of these 63% resulted in caesarean sections, 2% in the use of forceps, and 2% in the use of vacuum extraction). The infants were hospitalized for a minimum of 1 day and a maximum of 26 days (mean of 6 days and standard deviation of 4 days). The mean weight of the newborns was 2,366 g with a standard deviation of 940 g (min=520 g and max=4,290 g) and mean gestation was 35 weeks (min=24 weeks and max=42 weeks, and standard deviation was 4 weeks).
Procedures
The Neonatology Unit Parental Stress Assessment Scale - Modified Version (EASPUN-MV) was administered in seven public and private NICUs between July 2019 and May 2020. To quantitatively evaluate the content validity of the items, a panel of 10 experts (nurses and physician experts in neonatology) was used, according to the Lawshe model (1975). This model consists of item-by-item assessment, using a three-point scale on which the experts evaluated whether the item was "unnecessary to assess parental stress" (1); "useful, but not necessary to assess parental stress" (2); or ""essential to assess parental stress" (3). Only 8 items were considered non-essential, which greatly surpassed the 50% level of agreement among the experts necessary for the scale to present content validity28. The content validity ratio (CVR) was created to be interpreted as if it refers to one correlation (with values between -1 and 1). If all the experts on a panel report the items as essential, the CVR will be 1 (adjusted to 0.99); if at least half of the experts classify them as essential, the result is negative; if the number of items classified as essential does not reach 100%, but surpass 50%, as was the case in this study, the CVR falls between 0-0.99%, which is adequate for studies of this nature.
The psychometric qualities of the scale were assessed using SPSS Statistics® and AMOS® (Software SPSS® Statistics v.26) (SPSS, an IBM Company, New York, NY). The sensitivity of the EASPUN-MV items was evaluated using asymmetry (g1) and kurtosis (g2) coefficients, with reference values |g1|< 3 and |g2|< 7, respectively, and critical ratios <225)(27)(29) . The reliability of the four dimensions of the scale was calculated based on the mean correlations between the items of the scale, weighted by the variances, considering accepTable reliability if α ≥ 0.7026. Construct reliability was evaluated using composite reliability, while construct validity was calculated using factorial validity, convergent validity, and mean extracted variance (MEV). The results for composite reliability (CR) ≥ 0.70 and mean extracted variance (MEV) ≥ 0.50 indicate that the scale used valid and reliable constructs27.
Factors with an MEV greater than the square of the correlation among the factors were considered to have discriminant validity27,30. To analyze the factor validity of the model, confirmatory factor analysis was used, together with several empirical indexes to assess the model’s goodness of fit, such as the Chi-square fit test (x2/df), the comparative fit index (CFI), the goodness of fit index (GFI), the Tucker-Lewis index (TLI), and the root mean square error of approximation (RMSEA≤0.05).
RESULTS
The psychometric qualities of the EASPUN-MV were evaluated by estimating the sensitivity, validity and reliability of the items of the scale’s four dimensions using a sample of parents whose newborns had been admitted to NICUs. The dimensions were: Physical Environment and Sounds (AFS); Infant Look, Behavior and Treatment (ACBT) Parent’s Relationship with Infant and Parental Role (RBPP); and Family and Social Relationship (RFS). The analysis of the standardized estimates of the original scale (Neonatal Unit Parental Stress Scale - NUPS) with 65 items showed that some items had factor loadings below the reference value (β=0.5), which was reflected in the empirical indexes of the model fit, with adequate values between 0.60 and 0.70. The factorial model was adjusted, removing the items whose factor loadings were lower than the reference value (6 items from the AFS dimension; 3 items from the ACBT dimension; 11 items from the RBPP dimension; and 5 items from the RFS dimension). Thus, the modified scale had 40 items - the Neonatal Unit Parental Stress Assessment Scale-Modified Version (EASPUN-MV). The sensitivity of the EASPUN-MV items was assessed using asymmetry (g1) and kurtosis (g2) coefficients, whose results were lower than all the reference values, in all of the items, and the critical ratios were lower than 2 25)(27)(29) . Factor validity was evaluated via confirmatory factor analysis (CFA). This method is used when the researcher has previous information about the factorial structure that needs to be confirmed. The method allows evaluating the goodness of fit of a theoretical measurement model to the correlation structure observed between manifest variables27.
The four dimensions of the EASPUN-MV presented moderate correlation, as shown in Table 1.
Table 1: Pearson’s correlation coefficient between the four dimensions of the EASPUN-MV
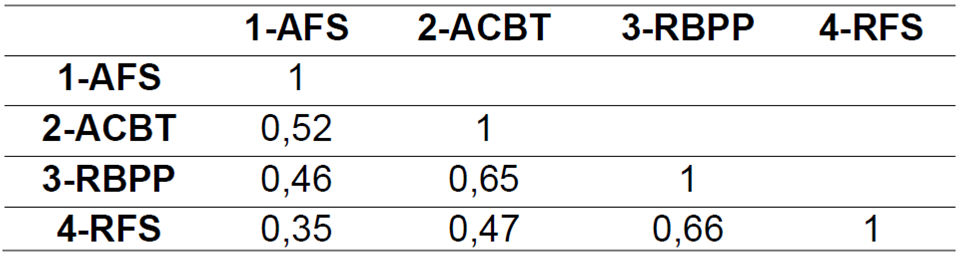
Not: Correlation is significant at the 0,01 level (2-tailed)
The reliability of all of the items and their dimensions was estimated based on the measurement of internal consistency, with Cronbach's α greater than the reference value, and for all of the items (α=0.94) and the 4 dimensions of the EASPUN-MV (AFS with 3 items, α=0.86; ACBT with 12 items, α=0.88; RBPP with 12 items, α=0.87, and FRS with 13 items, α=0.90). The factor loadings of the standardized estimates of the 40 items, obtained through confirmatory factor analysis, were higher than the reference value (β =0.50) (Table 2 and Figure 1).
Table 2: Standardized factor loadings (β) of EASPUN-MV items (40 items), obtained through confirmatory factor analysis and Cronbach's Alpha (α), for the four dimensions (n=406)

Figure 1 presents the factor analysis for EASPUN-MV with the factor loadings and goodness of fit indexes that support the four dimensions of the modified scale. The empirical indexes of the goodness of fit of the EASPUN-MV's factorial model improved when compared to the original scale with accepTable values (Chi-squared goodness of fit test χ2/df=3.3; comparative fit Index, CFI=0.8; goodness of fit index, GFI=0.8; Tucker-Lewis index, TLI=0.8, and root mean square error of approximation, RMSEA=0.07.

Figure 1: Confirmatory factor analysis of the EASPUN-MV with 40 items, adjusted to the validation sample (n = 406).
Composite reliability (CR) is an indicator of the internal consistency of the construct in the four dimensions (FCAFS= 0.925; FCACBT=0.924 and FCRBPP=0.917 FCRBPP=0.917), while convergent validity is estimated using the mean extracted variance (MEV) of the factor. The items strongly saturated this factor (VMEAFS=0.79; VMEACBT=0.48; VMERBPP=0.47 and VMERFS=0.53), because the results were close to or greater than the reference values.
DISCUSSION
The EASPUN-MV factorial model (65 items and four dimensions), adjusted to a sample of n=406, presented adequate goodness of fit values, with χ2 / df=3.2; CFI=0.6; GFI=0.6; TLI=0.8 and RMSEA=0.07, which led to the refinement of the initial model. The factorial model was adjusted, removing the items whose factor loadings were lower than the reference values, and the modified version of the scale (EASPUN-MV) then had 40 items distributed in four dimensions (AFS with 3 items, ACBT with 12 items, RBPP with 12 items, and RFS with 13 items).
The empirical indexes of the EASPUN-MV's factorial model goodness of fit improved compared to the original scale, presenting accepTable values (Chi-square goodness of fit test χ2/df=3.3; CFI=0.8; GFI=0.8; TLI=0.6 and P(RMSEA)=0.07). The items of EASPUN-MV showed good sensitivity, both globally and in each dimension (α>0.80), and good factor loadings. Only items 27 and 39 presented values close to the reference value (β=0.50) (0.49 and 0.48, respectively), while the others yielded values greater than the reference value25,26. The four dimensions presented moderate positive correlation. Composite reliability estimates the internal consistency of the items that reflect the construct, indicating to what extent the items express the latent factor. Values higher than 0.70 indicate good reliability, which was the case with the EASPUN-MV. The convergent validity of the four dimensions using MEV yielded results greater than the reference values and was considered adequate25. The results indicate that the EASPUN-MV presents adequate factorial validity, sensitivity and reliability with a sample of parents of newborns admitted to Portuguese NICUs. Therefore, it can be considered a quality instrument to assess parental stress in NICUs.
CONCLUSION
The Neonatal Unit Parental Stress Assessment Scale - Modified Version is a psychometrically sensitive, valid, and reliable instrument that can be used to systematically evaluate parental stress in the NICU. The present study considered the four dimensions of the scale: Physical Environment and Sounds (AFS); Infant Look, Behavior, and Treatment (ACBT); Parent’s Relationship with Infant and Parental Role (RBPP), and Family and Social Relationship (RFS). This information can facilitate decision-making among nurses, providing parents follow-up care, and referring them to other healthcare professionals.
REFERENCES
1. Campo-González A, Amador-Morán R, Alonso-Uría RM, Ballester-López I. Estrés en madres de recién nacidos ingresados en unidad de cuidados intensivos. Rev Cuba Obstet y Ginecol [Internet] 2018;44(2):ISSN 1561-3062. Available from: http://www.revginecobstetricia.sld.cu/index.php/gin/article/view/347/277 [ Links ]
2. Miles M. Parents of Critically ill premature infants:Sources of Stress. Crit Care Nurs Q [Internet] 1989;12(3):69-74. Available from: https://pubmed.ncbi.nlm.nih.gov/2819538/ [ Links ]
3. Pichler-Stachl E, Pichler G, Baik N, Urlesberger B, Alexander A, Urlesberger P, et al. Maternal stress after preterm birth: Impact of length of antepartum hospital stay. Women and Birth 2016;29(6):e105-9. [ Links ]
4. Tobo M, Bentacu M, De la Cruz E. Estímulos, afrontamiento y adaptación en padres de recién nacidos hospitalizados en unidades de cuidado intensivo neonatal. Investig Enferm Imagen Desarro [Internet] 2017;19(2):161-75. Available from: https://www.researchgate.net/publication/321816292_Estimulos_afrontamiento_y_adaptacion_en_padres_de_recien_nacidos_hospitalizados_en_unidades_de_cuidado_intensivo_neonatal [ Links ]
5. Sanders M, Hall S. Trauma-informed care in the newborn intensive care unit: Promoting safety, security and connectedness. J Perinatol [Internet] 2018;38(1):3-10. Available from: http://dx.doi.org/10.1038/jp.2017.124 [ Links ]
6. Botchway AK. Examining the Needs and Stress Levels of Fathers with Infants Receiving Neonatal Intensive [Internet]. 2018;Available from: https://prism.ucalgary.ca/bitstream/handle/1880/106784/ucalgary_2018_botchway_augusta.pdf?sequence=3&isAllowed=y [ Links ]
7. Govindaswamy P, Laing S, Waters D, Walker K, Spence K, Badawi N. Needs and stressors of parents of term and near-term infants in the NICU: A systematic review with best practice guidelines. Early Hum Dev 2019; [ Links ]
8. Ionio C, Colombo C, Brazzoduro V, Mascheroni E, Castoldi F, Lista G. Mothers and Fathers in NICU : The Impact of Preterm Birth on Parental Distress. Eur J Psychol [Internet] 2016;12(4):604-21. Available from: https://ejop.psychopen.eu/index.php/ejop/article/view/1093/pdf [ Links ]
9. Diffin J, Spence K, Naranian T, Badawi N, Johnston L. Stress and distress in parents of neonates admitted to the neonatal intensive care unit for cardiac surgery. Early Hum Dev [Internet] 2016;103:101-7. Available from: https://www.researchgate.net/publication/307156968_Stress_and_distress_in_parents_of_neonates_admitted_to_the_neonatal_intensive_care_unit_for_cardiac_surgery [ Links ]
10. Kegler J, Neves E, Silva A, Jantsch L, Bertoldo C, Silva J. Stress in Parents of Newborns in a Neonatal Intensive Care Unit. Esc Anna Nery [Internet] 2019;23(1):1-6. Available from: https://www.scielo.br/pdf/ean/v23n1/1414-8145-ean-23-01-e20180178.pdf [ Links ]
11. Noergaard B, Ammentorp J, Garne E, Fenger-Gron J, Kofoed P. Fathers' stress in a neonatal intensive care unit. Adv Neonatal Care [Internet] 2018;18(5):143-422. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6155352/pdf/ancr-18-413.pdf [ Links ]
12. Busse M, Stromgren K, Thorngate L, THOMAS K. Parents responses to stress in the Neonatal Intensive Care Unit. Neonatal Care [Internet] 2013;33(4):52-6. Available from: https://doi.org/10.4037/ccn2013715 [ Links ]
13. Stübe M, Rosa M, Pretto C, Cruz C, Morin P, Stumm E. Níveis de estresse de pais de recém-nascidos em Unidade de Terapia Intensiva Neonatal. Rev da Rede Enferm do Nord 2018;19:3254. [ Links ]
14. Leal I, Maroco J. Avaliação em sexualidade e parentalidade. Porto: Livpsic,; 2010. [ Links ]
15. Wereszczak, J.; Miles, MS; Holditch-Davis D. Maternal Recall of the Neonatal Intensive Care Unit. Neonatal NetworkThe J Neonatal Nurs [Internet] 1997;16(4):33-40. Available from: https://pubmed.ncbi.nlm.nih.gov/9216318/ [ Links ]
16. Holditch-Davis D, Miles M. Mothers' stories about their experiences in the neonatal intensive care unit. Neonatal Netw [Internet] 2000;19(3):13-21. Available from: https://www.researchgate.net/publication/11417927_Mothers'_Stories_about_Their_Experiences_in_the_Neonatal_Intensive_Care_Unit [ Links ]
17. Miles MS, Funk SG, Kasper MA. The neonatal intensive care unit environment: sources of stress for parents. AACN Clin Issues Crit Care Nurs [Internet] 1991;2(2):346-54. Available from: https://doi.org/10.4037/15597768-1991-2022 [ Links ]
18. Miles MS, Brunssen SH. Psychometric properties of the parental stressor scale: Infant hospitalization. Adv Neonatal Care [Internet] 2003;3(4):189-96. Available from: 10.1016/s1536-0903(03)00138-3 [ Links ]
19. Reid T, Bramwel R. Using the parental stressor scale: NICU with a British sample of mothers of moderate risk preterm infants. J Reprod Infant Psychol [Internet] 2003;21(4):279-91. Available from: http://dx.doi.org/10.1080/02646830310001622114 [ Links ]
20. Reid T, Bramwell R, Booth N, Weindling AM. A new stressor scale for parents experiencing neonatal intensive care: The NUPS (Neonatal Unit Parental Stress) scale. J Reprod Infant Psychol [Internet] 2007;25(1):66-82. Available from: https://www.researchgate.net/publication/262950536_A_new_stressor_scale_for_parents_experiencing_neonatal_intensive_care_The_NUPS_Neonatal_Unit_Parental_Stress_scale [ Links ]
21. Abidin RR. The Determinants of Parenting Behavior. J Clin Child Psychol [Internet] 1992;21(4):407-12. Available from: https://doi.org/10.1207/s15374424jccp2104_12 [ Links ]
22. Wolke D, Johnson S, Mendonça M. The Life Course Consequences of Very Preterm Birth. Annu Rev Dev Psychol 2019;1(1):69-92. [ Links ]
23. Beaton D, Bombardier C, Guillemin F, Ferraz MB. Recommendations for the Cross-Cultural Adaptation of the DASH & Outcomes Measures. Inst Work Heal [Internet] 2007;45. Available from: https://www.researchgate.net/publication/265000941_Recommendations_for_the_Cross-Cultural_Adaptation_of_the_DASH_QuickDASH_Outcome_Measures_Contributors_to_this_Document/references#fullTextFileContent [ Links ]
24. Marôco J. Análise Estatística com o SPSS Statistics. 7a. Pêro Pinheiro, Portugal: Report Number; 2018. [ Links ]
25. Curado MAS, Teles J, Marôco J. Analysis of variables that are not directly observable: influence on decision-making during the research process. Rev da Esc Enferm da USP [Internet] 2014;48(1):146-52. Available from: https://www.researchgate.net/deref/http%3A%2F%2Fdx.doi.org%2F10.1590%2FS0080-623420140000100019 [ Links ]
26. Hill MM, Hill A. Investigação por Questionário. 2nd ed. Lisboa: 2008. [ Links ]
27. Marôco J. Análise de Equações Estruturais. Fundamentos teóricos, Software e Aplicações. 2nd ed. Pêro Pinheiro, Portugal: ReportNumber; 2014. [ Links ]
28. Lawshe CH. A quantative approach to content validity. Pers Psychol [Internet] 1975;28(4):563-75. Available from: aepnet.org/~/media/Files/caep/knowledge-center/lawshe-content-validity.pdf [ Links ]
29. Kline RB. Principles And Practice Of Structural Equation Modeling. Nova Iorque: 2015. [ Links ]
30. Maroco J, Garcia-Marques T. Qual a fiabilidade do alfa de Cronbach? Questões antigas e soluções modernas? Laboratório Psicol [Internet] 2006;4(1):65-90. Available from: http://publicacoes.ispa.pt/index.php/lp/article/view/763 [ Links ]
Received: December 10, 2020; Accepted: March 05, 2021











 texto en
texto en 


