Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Enfermería Global
versión On-line ISSN 1695-6141
Enferm. glob. vol.20 no.64 Murcia oct. 2021 Epub 25-Oct-2021
https://dx.doi.org/10.6018/eglobal.472871
Originals
Analysis of the multicausal model of anemia level in children 6-35 months old in Peru
1 .Enfermera. Departamento de Investigación de la Facultad de Ciencias de la Salud. Universidad Católica Sedes Sapientiae. Perú. kortiz@ucss.edu.pe
2 . Enfermero. Coordinador del Departamento de Investigación de la Facultad de Ciencias de la Salud. Universidad Católica Sedes Sapientiae. Perú.
3 . Nutricionista. Departamento de Investigación. Facultad de Ciencias de la Salud. Universidad Católica Sedes Sapientiae. Perú. Centro de Salud Los Libertadores de la DIRIS Lima Norte, MINSA.
4 . Médico cirujano. Director académico de la Facultad de Ciencias de la Salud de la Universidad Católica Sedes Sapientiae. Perú
5 .Estadístico e informático. Magister en Salud Pública con mención en Epidemiología. Profesor de la Escuela de Posgrado de la Universidad Norbert Wiener. Perú
Introduction
Iron deficiency anemia in children from 6 to 35 months is a severe public health issue.
Objective
to determine the prevalence of anemia level and related factors in children under three years applying multicausal model in Peruvian population.
Materials and methods
To explanatory level research was carried out applying a secondary analysis with data found in the database of the 2019 Demographic and Family Health Survey. The main variable was the level of anemia in which Hemocue® test was used. Weighted values, frequencies, percentages, goodness-of- fit, and an ordinal regression model were taken into consideration.
Results
40.20% of children under three years old presented anemia. Factors as presence of diarrhea (OR = 1.30), 12 months of life (OR: 3.33), not starting prenatal control (OR: 1.19), male gender (OR: 1.25), mother with anemia (OR: 1.75), mothers who are 15 to 24 (OR: 1.94), water well as a source of water (OR: 1.53), Aymara as mother tongue (OR: 2.31) were associated with anemia level.
Conclusions
Among the risk factors associated with anemia according to the multicausal model, diarrhea in the last two weeks is a determinant factor, among the underlying factors are the child's age, source of drinking water, prenatal care, anemia and the woman's age. In addition, the protective factors correspond to breastfeeding for some time and the highest wealth quintile.
Keys words: Anemia. iron-Deficiency; Public Health; Risk Factors
INTRODUCTION
Iron deficiency anemia is caused by a decrease in the hemoglobin in blood due to a lack of iron in the body 1. This nutritional disorder affects every stage of life. However, women and preschool children are the most vulnerable 2. In the case of preschool children, the World Health Organization (WHO) states that 293.1 million people suffer from anemia worldwide and half of these cases are caused by iron deficiency. This happens because children in this stage have iron needs that are not supplied in the growth process 3,4. Also, the WHO in its latest report of "Worldwide Prevalence of Anemia 1993-2005" estimates that worldwide, the prevalence of anemia in these children was 47.4%, it should be taken into account when the prevalence is greater than 40% it is considered a severe public health problem, between 20- 39.9% as moderate, and between 5 -19.9% as low (4). In Peru, the prevalence of anemia in children ages 6 to 35 months according to the Demographic and Family Health Survey in 2019 was 40.1%. Most affected were those who lived in either rural (49%) or mountainous regions. (48.8%) and had a lower wealth quintile (50.9%) 5.
This high prevalence of anemia mainly affects developing countries with severe consequences for human health that irreversibly compromise the development and growth of children. Besides a decrease in the immune function that exposes them to infections, there are also decreased response capacities and activities that will cause a loss of productivity when they become adults. It also causes a high percentage of premature births, impacting the country's economy 1. In Peru it has been observed that in the last decade this prevalence has been decreasing slowly. It still remains above 40% and despite great efforts 6 it is still considered an important issue of Public Health. Furthermore, there is still difficulty in the implementation of effective measures to eradicate it in the most vulnerable populations 5.
The WHO, among other studies, have carried out searches on the prevalence of anemia in preschool children that are considered a severe problem in Public Health. However, there is great interest in the causes or contributing factors that must be identified and addressed to eradicate anemia 3)(4)(7)(8)(9)(10. Thus, there is a conceptual model proposed in various studies on the predictors of anemia 6)(7)(9)(11 and undoubtedly at the biological level, it is known that the main causes of anemia are due to the loss of erythrocytes, because of a decrease in their production. In addition to these causes, there are others, which include inadequate intake and absorption of micronutrients, hemoglobin disorders and exposure to infectious diseases. (Such as the presence of parasites or diarrhea) 6)(8)(12. Second, there are underlying causes at the household/family level such as access to water and sanitation, availability of health services, childcare practice, and access to various sources of food. Finally, there are root causes related to the socioeconomic scenario and cultural behaviors (9). For the present work, the models used by Shenton and Balarajan were adapted for the construction of the conceptual framework of the problem, categorizing and selecting the factors (immediate, underlying and basic or distal) 9,11.
Despite the fact that anemia is considered an important Public Health issue, scientific research on anemia in preschool children carried out in Peru is less compared to other countries 7)(8)(9)(12)(13, and has generally involved small sample sizes, from groups that were not representative of the whole country and did not take into account most of the predictors of the conceptual model of anemia 10)(14)(15)(16. It is important to fight and deal with anemia as soon as possible, especially in children under three years, because it is that preschool age group that has such a high prevalence of anemia in Peru 5,17, as mentioned in the National Plan for the Reduction and Control of Maternal and Child Anemia and Chronic Child Malnutrition 2017-2021 6. Enacting this plan would improve children's health and therefore their productivity levels in the future. For these reasons, the objective of the study was to determine the prevalence of the level of anemia and its associated factors in children under three years of age using a multicausal model in Peruvian population.
MATERIALS AND METHODS
Design and research sample
An explanatory-level study was carried out through a secondary analysis with data from the database of the 2019 Demographic and Family Health Survey (ENDES 2019) 5. The sampling carried out was two-stage through clusters (1st stage with 3,253 clusters), stratified by areas and zones of Peru (2nd stage with 36,745 selected dwellings) to obtain national representativeness. For this, questionnaires were individually delivered to women between 15 and 49 years old to collect information on their health status and that of their children under five years, as well as their demographic dynamics. ENDES addresses many health problems, including women's reproduction and child health, including breastfeeding, nutrition, vaccinations, anemia, and diarrhea 5. The effective sample was of 10,421 children from 6 to 35 months with complete information related to the selected predictors of childhood anemia.
Level of anemia
The main variable was anemia level, an ordinal qualitative variable, grouped into: no anemia (≥10.9 g / dl), mild anemia (10.0-10.9 g / dl), moderate anemia (7, 0-9.9 g / dl) and severe anemia (<7.0 g / dl) (19). The Hemocue® test was used as an analyzer to measure the hemoglobin concentration. Hemoglobin levels were adjusted for altitude applying the Pediatric Nutrition Surveillance System (CDC / PNSS) and Dirren 20 formula.
Factors associated with anemia level
The variables were adapted to the models used by Shenton and Balarajan for the construction of conceptual framework of the problem, categorizing and selecting the factors 9,11. Furthermore, the review by Siekmans 18 was used, which considers malnutrition as a reliable indicator of exposure to anemia.
On one hand, the immediate factors were; diarrhea in the last 14 days, qualitative dichotomous (yes or no). Fever in the last 14 days, qualitative dichotomous (yes or no). Antiparasitic medication for the child, qualitative dichotomous (yes or no). Chronic malnutrition, qualitative dichotomous (yes or no) using the Height for Age indicator (T / E) and if it is less than -2 standard deviation (SD). Iron supplement for the child, qualitative dichotomous (yes or no) measured through the following questions; took iron in syrup, powder as micronutrients, drops or other presentation in the last seven days; and doses of vitamin A for the child, qualitative dichotomous (yes or no) measured if he has received doses in the first two months.
On the other hand, the underlying factors were: source of tap water, nominal qualitative (water network, bottled water, well water, and tanker trucks suppliers). Health insurance coverage, qualitative dichotomous (yes or no). Child’s age (months), qualitative ordinal (less than 12 months, 12-23 months and 24-35 months). Birth order number, qualitative ordinal (1, 2-3 and 4+). Sex of the child, qualitative dichotomous (man and woman). Maternal age (years), qualitative ordinal (15-24 years, 25-29 years, 30-34 years and 35-49 years). Dietary diversity, qualitative dichotomous (<4 and ≥4) considering seven groups (i) grains, roots and tubers; (ii) legumes and dried fruits; (iii) dairy products; (iv) fresh food (meat / fish / poultry); (v) eggs; (vi) fruits rich in vitamin A and vegeTables; and (vii) other fruits and vegeTables. Diet quality, nominal qualitative (vegeTable only, animal only, and both). Breastfeeding, qualitative nominal (never breastfed, ever breastfed, and currently breastfeeding). Anemia in the mother, qualitative dichotomous (yes or no). Iron supplement during pregnancy, qualitative dichotomous (yes or no). Prenatal control (number of visits), qualitative dichotomous (≥6 and <6). Prenatal control in the first trimester, qualitative dichotomous (no and yes) and care in a health center for diarrhea, fever or vomiting by the child qualitative dichotomous (yes or no).
Finally, the basic or distal factors were: educational level of the mother, qualitative ordinal (no education, primary, secondary and higher). Mother tongue, qualitative nominal (Spanish, Quechua, Aymara and another language). Wealth quintile, ordinal qualitative (upper quintile, fourth quintile, intermediate quintile, second quintile and lower quintile), said variable took into account the assets or wealth of the households that were surveyed. Therefore, it depends on the disposition of the goods, services and characteristics of each household. Maternal autonomy for decision making, qualitative dichotomous (yes or no). Maternal attitudes that justify domestic violence qualitative dichotomous (yes or no). Children at home, qualitative ordinal (1, 2 and + 3). Beginning of maternity, qualitative ordinal (10-24 years, 25-29 years, 30-34 years and 35-45 years). Births in the last five years, qualitative ordinal (1, 2 and + 3). Waiting time (years) since the last child, qualitative ordinal (0, 1, 2 and + 3). Natural, qualitative nominal region (Lima and Callao, rest of the coast, mountains and jungle). Residence, qualitative dichotomous (urban and rural). Altitude, qualitative ordinal (<1,000, 1,000 to 1,999, 2,000 to 2,999, 3,000 to 3,999 and ≥4,000) and emotional violence, qualitative dichotomous (yes or no).
Statistic analysis
For the statistical analysis, contingency Tables were prepared using the Stata SE version 14 program to obtain frequencies and percentages. The degree of association between the level of anemia and the factors was estimated with the Chi-square test. The goodness-of- fit was performed with the Hosmer Lemeshow test for the factors and subsequently considered under the ordinal regression model estimating the Odds ratios (OR) and 95% confidence intervals.
Because ENDES is a complex two-stage sample, weighted values were considered. In addition, ENDES 2019 guaranteed the anonymity of the participants using codes for them. Finally, all participants gave verbal consent.
RESULTS
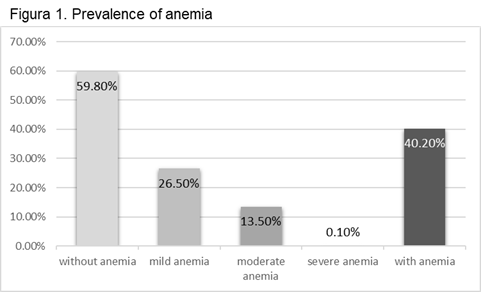
Figure 1 shows that there is a low percentage of severe anemia, however, in general, 40.20% of all children had iron deficiency anemia.
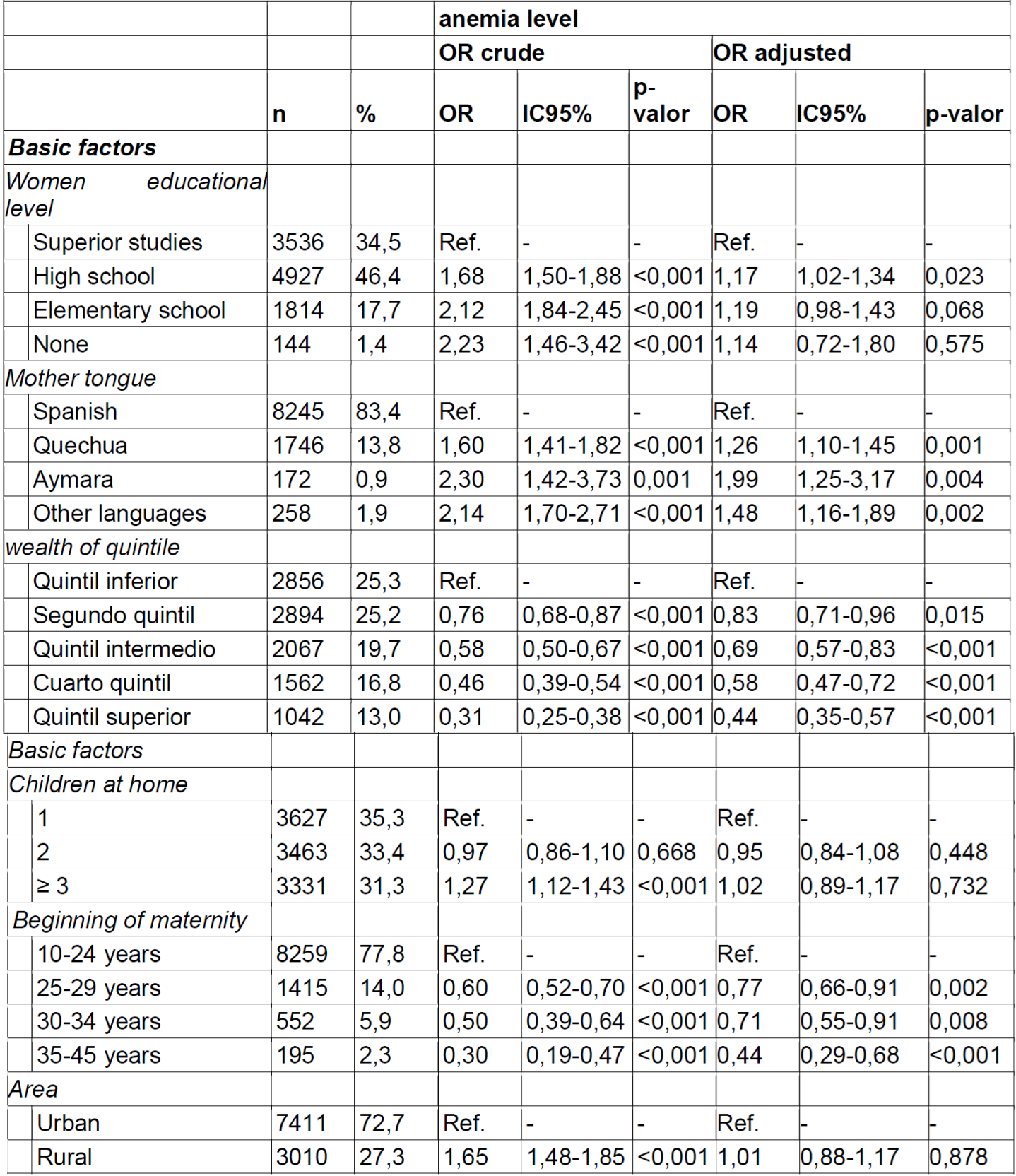
Of the total of children under three years, 15.4% had diarrhea in the last two weeks, while 66.8% did not consume an iron supplement. Regarding the underlying factors, children aged 24 to 35 months and 12 to 23 months were the most represented (40.0%); and the proportion of boys and girls in the sample was similar with 51% and 48.9% respectively. Of all the mothers, 27.3% reported being 15 to 24 years. In addition, 50.5% are currently breastfeeding; and 19.7% presented anemia. Regarding the basic factors, the highest percentages were observed in the lowest wealth quintile (25.3%) and the beginning of motherhood who are 15 to 24 years (77.8%). The rest of the description of the factors can be seen in Table 1. On the other hand, in the results of the bivariate associations with the unadjusted model, it was evidenced that most of the factors were significantly associated with the level of anemia as shown. detailed in Table 1, Tablas 1, 2 and 3 , except for the factors: vitamin A dose, health insurance coverage, iron supplement during pregnancy, maternal autonomy for decision-making, maternal attitudes that justify physical and emotional violence because in the multiple regression they did not comply with the goodness-of-fit detailed below.
In the same Tables 1, Tablas 1, 2 and 3 the multiple regression that has been carried out in the study can be visualized. For the direct factors, the probability of the level of anemia was estimated with the immediate factors, obtaining a good fit of 0.37; For the underlying factors, the relationships between them and the probability of the level of anemia were evaluated, having a good fit of 0.38; For the basic factors, the relationship between them and the level of anemia in children under three years was considered, in this model it reported a fit of 0.08.
Table 1. Association among the direct factors of children 6 -35 months and anemia level. ENDES 2019.

Finally, in Figure 2, the joint interaction between the previous factors cited was carried out with the increase anemia level, the following variables remaining statistically significant: children under 12 months (OR = 3.33 95% CI 2.76- 4.03), having Aymara as their mother tongue (OR = 2.31 95% CI 1.35-3.93), mothers who are between 15 and 24 years old (OR = 1.94 95% CI 1.53-2, 44), mothers who have anemia (OR = 1.75 95% CI 1.53-2.00), have a water well as a source of water (OR = 1.53 95% CI 1.08-2.17) , children who have had diarrhea in the last 14 days (OR = 1.30 95% CI 1.13-1.50), male gender child (OR = 1.25 95% CI 1.12-1.39) , that the mother had a prenatal check-up in the first trimester (OR = 1.19 95% CI 1.02-1.39). However, an inverse relationship was found with two variables that have a protective effect with the level of anemia, these are: children who ever breastfed (OR = 0.65 95% CI 0.58-0.74) and being in the upper quintile (OR = 0.52 95% CI 0.40-0.69). This multicausal effect is also seen in this Figure with a goodness - of- fit of 0.32.
Table 2. Association among the underlying factors of children 6-35 months and anemia. Level ENDES 2019.

DISCUSSION
Anemia prevalence in children under three years old in Peru is estimated at 40.20%. As a result, it is still considered a severe public health issue; Despite the fact that the percentage of moderate and severe anemia is low and that a substantial decrease in the prevalence has been shown in the last decade 5,6, there is evidence of an increase in the disparities between the regions of Peru, the area of residence and has remained relatively constant over time 6. The analysis using the multicausal model helped to identify that the factors: diarrhea in the last 14 days, source of drinking water, age and child’s gender; age and anemia in mothers, breastfeeding and prenatal care; wealth quintile and mother tongue were associated with the anemia level.
In this research, children who had diarrhea in the last two weeks were more likely to have severe anemia (OR: 1.30). This finding is similar to a study in northern Ethiopia 12 and Peru 10 showed diarrhea presence is a risk factor for anemia in children with an OR of 1.3 and 1, 2 correspondingly. For proper digestion and absorption of nutrients, the functional integrity of small and large intestine is necessary; and the absence of inflammatory processes 21. Because of this, the iron that is physiologically absorbed mainly in the duodenum would prevent the presence of intestine inflammation which is characterized by persistent diarrhea and this would become more severe when blood is found in stool 6. Because of this, nutritional anemia due to iron deficiency is considered a frequent condition in children with chronic diarrhea 22, which must be rapidly detected with important child care by their mother as practices for prevention 10.
Another finding in relation to the previous one is that having water well as a source of water involves a greater probability that children will suffer from anemia 9. Nationwide 91.1% of households have access to treated water, but only 38.7% of them have water with a sufficient proportion of residual chlorine similar to or greater than 0.5mg / l, a proportion that is lower in rural areas compared to urban areas 6 because of the location of underground wells which unfortunately, are exposed to being contaminated by sewage water filtering, becoming one of the main vehicles of disease transmission, affecting the most vulnerable population, including children. In this regard, inadequate access to drinking water eases the entry of parasites, among other infections that cause iron deficiency anemia through different mechanisms such as diarrhea 12,23.
The prevalence of anemia in childhood is considered a Public Health issue. In Peru, it happens in children under three, compared to other countries in Africa, in which it is evidenced in children under five. However, all researchers agree that children under 12 months are the age group most likely to have anemia 7)(8)(10)(13. This result is due to the fact that six-months children depend on the complementary feeding and dietary iron intake, for this reason if the diet rich in iron was insufficient, unbalanced, delayed or rejected, it will cause iron deficiency anemia 24.
The present investigation showed that boys were more likely to have severe anemia compared to girls 10,15. An investigation revealed statistical gender differences in relation to diarrhea due to parasites, due to the fact that boys, unlike girls, are more exposed to sources of infection related to their playing habits and other indoor activities and they almost never adopt hygienic practices 25. That is to say that it can be inferred that diarrhea, which is more frequent in children, causes anemia. However, at the level of iron requirement, there is no difference according to gender 26. Therefore, it is recommended to address in depth this factor associated with anemia.
the research evidences the role of mothers is a key factor in identifying the presence of anemia in their children, which is why a greater probability of anemia is observed in children whose mothers are younger (15 to 24 years) as shown by two investigations in Peru 10,15. The majority of adolescent or young women living in developing countries, as well as in many developed countries, who have not planned to have children or are not considering responsible parenthood, initiate pregnancy with limited iron in their body. In other words, at the level of nutritional requirement, iron stores in pregnancy directly influence the health of the fetus and this could mean a greater risk for iron deficiency in childhood 27.
The previous statement can be contrasted with another finding of the study where this increased probability of anemia is shown in children under three years who have mothers with anemia. These findings are similar to several international and national studies 7)(8)(9)(10)(15. The possible explanation is that mothers of infants with anemia started pregnancy with decreased hemoglobin or had anemia within the trimester of pregnancy 27,28. The strongest data seem to indicate that the children of mothers with iron deficiency anemia are born with decreased iron stores, because a newborn has iron stores that come mainly from the maternal iron supply during intrauterine life 27,28.
Women who did not have prenatal care in the first trimester were more likely to have children with anemia 10. In prenatal care, it is very important in health of the pregnant woman because actions and procedures aimed at prevention, diagnosis and treatment are carried out to identify risks, diseases and abnormalities during pregnancy, both in the mother and the fetus, and avoid thus maternal and perinatal morbidity and mortality. Pregnant women who are not controlled are more vulnerable to complications; however, if they are detected early, they can be treated on time 6.
Mothers who breastfed their children after 6 months were less likely to have anemia in their children compared to those who are currently breastfeeding 10. This is because from 6 months of age, complementary foods and feeding practices are especially important in determining micronutrient sufficiency in children from 6 to 23 months, since breast milk at this age makes progressively less contribution to nutritional needs. Some studies agree, saying that discontinuing breastfeeding and starting with food would relate to a lower probability of developing anemia 10.
Concerning the basic factors associated with anemia in children, the mother's Aymara language was a risk factor 10, while the highest wealth quintile was a protective factor 9,10. The linguistic background such as the Aymara and Quechua languages of a pregnant woman or mother is still considered in Peru a barrier to maternal and child health 29. Even a study reported in women with Aymara language from Bolivia concludes that there is limited access to primary health care due to travel time, physical, climatic, technological and socioeconomic barriers 30, but this could disappear due to the improvement of the educational and socioeconomic level of households, in order to avoid inequities in the mothers and their children’s health.
Among the limitations in research, some factors could not be found in the ENDES, such as ecological factors, the presence of malaria and parasitosis, economic policies, foods fortified with iron, genetic hemoglobin disorders, among others, which would give a better understanding of childhood anemia. On the other hand, the study has strengths because the results are nationally representative and consistent with the literature, it is also the first study in Peru that analyzed the data based on a multicausal model.
CONCLUSION
40.20% of children under three years suffer from anemia in Peru, which represents a severe public health issue. Included among the risk factors associated with anemia according to the multicausal model is diarrhea in the last two weeks as an immediate factor. Other underlying factors include; being under one year of age, being male, having water well as access to water, the presence of anemia in the mother, and a lack of prenatal controls during pregnancy. Also, breastfeeding was considered a protective factor. Finally, among the basic factors, Aymara as a mother tongue is considered a risk. Households belonging to the highest wealth quintile represents a lower risk.
It is recommended to introduce policies to reduce the prevalence of anemia. Secondly, prenatal care visits are necessary to ensure that mothers receive adequate nutrition during pregnancy. Furthermore, improving the quality of care that mothers provide to their children, accompanied by monitoring of nutrition in the short and long term, (including interventions to encourage populations to diversify children's foods and fortify them with iron). Thirdly, improving access to drinking water and better sanitation in various households in Peru would be beneficial, since diarrhea has an effect on anemia. Finally, strategies must be implemented to include Aymara-speaking mothers and the lowest wealth quintile in the provision of health services with equity.
REFERENCIAS
1. Organización Mundial de la Salud. Carencia de micronutrientes [Internet]. Ginebra: OMS; 2020 [citado el 12 de agosto de 2020]. Disponible en: https://www.who.int/nutrition/topics/ida/es/ [ Links ]
2. Organización Mundial de la Salud. Metas mundiales de nutrición 2025. Documento normativo sobre anemia [Internet]. Ginebra: OMS; 2017 [citado el 12 de agosto de 2020]. Disponible en: https://apps.who.int/iris/bitstream/handle/10665/255734/WHO_NMH_NHD_14.4_spa.pdf?ua=1 [ Links ]
3. Organización Mundial de la Salud. Administración de suplementos de hierro en niños de 6 a 23 meses de edad [Internet]. Ginebra: OMS; 2015 [citado el 12 de agosto de 2020]. Disponible: https://www.who.int/elena/titles/iron_supplementation_children/es/ [ Links ]
4. Organización Mundial de la Salud. Worldwide prevalence of anaemia 1993-2005 [Internet]. Ginebra: OMS; 2008 [citado el 12 de agosto de 2020]. Disponible en: https://apps.who.int/iris/bitstream/handle/10665/43894/9789241596657_eng.pdf?sequence=1 [ Links ]
5. Instituto Nacional de Estadisticas e Informatica. Perú. Encuesta Demográfica y de Salud Familiar 2019 [Internet]. Lima: INEI; 2020 [citado el 12 de agosto de 2020]. Disponible en: https://www.inei.gob.pe/media/MenuRecursivo/publicaciones_digitales/Est/Endes2019/ [ Links ]
6. Ministerio de Salud. Plan Nacional para la Reducción y Control de la Anemia Materno Infantil y la Desnutrición Crónica Infantil 2017-2021 [Internet]. Lima: MINSA; 2017 [citado el 12 de agosto de 2020]. Disponible en: http://bvs.minsa.gob.pe/local/MINSA/4189.pdf [ Links ]
7. Khanal V, Karkee R, Adhikari M, Gavidia T. Moderate-to-severe anaemia among children aged 6-59 months in Nepal: an analysis from Nepal demographic and health survey, 2011. Clinical epidemiology and global health. 2016;4(2), 57-62. DOI: https://doi.org/10.1016/j.cegh.2015.07.001 [ Links ]
8. Muchie KF. Determinants of severity levels of anemia among children aged 6-59 months in Ethiopia: further analysis of the 2011 Ethiopian demographic and health survey. BMC Nutr 2, 51 (2016). DOI: https://doi.org/10.1186/s40795-016-0093-3 [ Links ]
9. Shenton LM, Jones AD, Wilson ML. Factors Associated with Anemia Status Among Children Aged 6-59 months in Ghana, 2003-2014. Maternal and Child Health Journal. 2020;24:483-502. DOI: https://doi.org/10.1007/s10995-019-02865-7 [ Links ]
10. Velásquez JE, Rodríguez Y, Gonzáles M, Astete L, Loyola J, Vigo WE, et al. Factores asociados con la anemia en niños menores de tres años en Perú: análisis de la Encuesta Demográfica y de Salud Familiar, 2007-2013. Biomédica. 2016;36(2):220-229. DOI: http://dx.doi.org/10.7705/biomedica.v36i2.2896 [ Links ]
11. Balarajan Y, Ramakrishnan U, Özaltin E, Shankar AH, Subramanian SV. Anaemia in low-income and middle-income countries. The lancet. 2011;378(9809):2123-2135. DOI: https://doi.org/10.1016/S0140-6736(10)62304-5 [ Links ]
12. Wasihun AG, Teferi M, Negash L, Marugán J, Yemane D, McGuigan KG, Dejene T A. Intestinal parasitosis, anaemia and risk factors among pre-school children in Tigray region, northern Ethiopia. BMC Infectious Diseases. 2020;20(379):1-11. DOI: https://doi.org/10.1186/s12879-020-05101-8 [ Links ]
13. Xin QQ, Chen BW, Yin DL, Xiao F, Li RL, Yin T, et al. Prevalence of anemia and its risk factors among children under 36 months old in China. Journal of tropical pediatrics. 2017,63(1):36-42. DOI: https://doi.org/10.1093/tropej/fmw049 [ Links ]
14. Munares O, Gómez G. Adherencia a multimicronutrientes y factores asociados en niños de 6 a 35 meses de sitios centinela, Ministerio de Salud, Perú. Revista Brasileira de Epidemiologia. 2016;19(3):539-553. DOI: https://doi.org/10.1590/1980-5497201600030006 [ Links ]
15. Baca N. Factores asociados con la anemia en niños menores de tres años en condición de pobreza y pobreza extrema en el perú: 2017. SOLIDARI(E)DAD (E)-Revista Iberoamericana de Empresa Solidária. 2018;1(1):54-64. [ Links ]
16. Gonzales E, Huamán L, Gutiérrez C, Aparco JP, Pillaca J. Caracterización de la anemia en niños menores de cinco años de zonas urbanas de Huancavelica y Ucayali en el Perú. Revista Peruana de Medicina Experimental y Salud Pública. 2015; 32(3):431-439. [ Links ]
17. Arroyo J. Hacia un Perú sin anemia. Rev Peru Med Exp Salud Publica. 2017;34(4). DOI: https://doi.org/10.17843/rpmesp.2017.344.3279 [ Links ]
18. Siekmans K, Receveur O, Haddad S. Can an integrated approach reduce child vulnerability to anaemia? Evidence from three African countries. PloS one. 2014;9(3):e90108. DOI:https://doi.org/10.1371/journal.pone.0090108 [ Links ]
19. Organización Mundial de la Salud. Concentraciones de hemoglobina para diagnosticar la anemia y evaluar su gravedad [Internet]. Ginebra: OMS, 2011 [citado el 12 de agosto de 2020]. Disponible en: https://www.who.int/vmnis/indicators/haemoglobin_es.pdf [ Links ]
20. Gómez-Sánchez I, Rosales S, Agreda L, Castillo A, Alarcón-Matutti E, Gutiérrez C. Nivel de hemoglobina y prevalencia de anemia en gestantes según características socio-demográficas y prenatales. Revista peruana de epidemiología. 2014;18(2):1-6. [ Links ]
21. Riverón RL. Fisiopatología de la diarrea aguda. Revista Cubana de Pediatría. 1999;71(2):86-115. [ Links ]
22. La Rosa D, García E, Vega H, Lazo S, Gutiérrez ÁE, Sánchez N, et al. Estado inmunonutricional en niños con diarrea crónica inespecífica. Revista Habanera de Ciencias Médicas. 2014;13(6):873-883. [ Links ]
23. Chávez M, Rivera G, Romero T, Vizcarra I. El pozo: usos, seguridad y tradición en la subcuenca del río San Javier. Estudios sociales (Hermosillo, Son.). 2013;21(41):261-286. [ Links ]
24. Donato H, Cedola A, Rapetti MC, Buys MC, Gutiérrez M, Parias R, et al. Anemia ferropénica. Guía de diagnóstico y tratamiento. Arch Argent Pediatr, 107(4). 2009; 107(4):353-361. [ Links ]
25. Dana D, Mekonnen Z, Emana D, Ayana M, Getachew M, Workneh N, Vercruysse J, Levecke B. Prevalence and intensity of soil-transmitted helminth infections among pre-school age children in 12 kindergartens in Jimma Town, southwest Ethiopia. Trans R Soc Trop Med Hyg. 2015;109:225-227. [ Links ]
26. Gómez C, Sastre AA. Tabla de recomendaciones (normativas y recomendaciones nutricionales). Soporte Nutr en el paciente oncológico. 2002:317-22. [ Links ]
27. Ortiz YJ, Ortiz KJ, Castro BS, Nuñez SC, Rengifo GL. Factores sociodemográficos y prenatales asociados a la anemia en gestantes peruanas. Enfermería Global. 2019; 18(56), 273-290. [ Links ]
28. Rao R, Georgieff MK. Iron in fetal and neonatal nutrition. Semin Fetal Neonatal Med 2007;12:54-63. [ Links ]
29. Valdivia M. Etnicidad, antecedentes lingüísticos y la salud materno infantil en el Perú. Lima: INEI; 2007 [citado el 12 de agosto de 2020]. Disponible en: https://www.inei.gob.pe/media/MenuRecursivo/publicaciones_digitales/Est/Lib0699/Libro.pdf [ Links ]
30. Perry B, Gesler W. Physical access to primary health care in Andean Bolivia. Social Science & Medicine. 2000;50(9):1177-1188. [ Links ]
Received: March 12, 2021; Accepted: July 03, 2021











 texto en
texto en