Meu SciELO
Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Enfermería Global
versão On-line ISSN 1695-6141
Enferm. glob. vol.21 no.66 Murcia Abr. 2022 Epub 02-Maio-2022
https://dx.doi.org/10.6018/eglobal.478501
Reviews
Difficulties and strategies associated with nurse integration in critical care provision: a scoping reviewi
1a Instituto de Ciencias de la Salud - Universidad Católica Portuguesa (ICS-UCP), RN.
1b Hospital de la Luz Torres de Lisboa. Lisboa. Portugal. diflores94@gmail.com
2a Instituto de Ciencias de la Salud - Universidad Católica Portuguesa (ICS-UCP), RN.
2b Centro Hospitalario Universitario Lisboa Central, EPE - Hospital de San José. Lisboa. Portugal.
3a Instituto de Ciencias de la Salud - Universidad Católica Portuguesa (ICS-UCP), RN.
3b Centro Hospitalario Universitario Lisboa Central, EPE - Hospital de San José. Lisboa. Portugal.
4 ICS-UCP, RN, MsNC, PhD. Lisboa. Portugal.
Introduction:
The nurses' integration in specialized care provision to critically ill patients is an increasing concern in the context of hiring and mobilizing nursing professionals. An adequate integration is crucial for the nurses' success and adaptation to the new service, as well as to ensure the quality and safety of the provided care.
Objective:
To map the existing knowledge on the difficulties experienced by nurses, as well as on the strategies that facilitate their integration in specialized care provision to the critically ill.
Method:
A scoping review was conducted, following the method proposed in the Joanna Briggs Institute Reviewers' Manual 2015. The following were used as inclusion criteria: Population - nurses; Concept - the experienced difficulties and the strategies employed to facilitate the nurses' integration; Context - the provision of care to the critically ill. A total of 13 articles, published until May 2020, were included.
Results:
The following difficulties were reported: communication issues with the team, as well as with the patients and/or their relatives; overall stress; dealing with complex health conditions, as well as with intricate procedures and/or techniques; work overload; high staff turnover rate between services; dealing with a patient's death and/or with organ donation planning. The following were pointed out as facilitating strategies: simulated practice; performing teamwork; assignment of a nursing supervisor/tutor; receiving feedback; developing resilience mechanisms.
Conclusion:
As regards care provision, the nurses' integration process requires planning and the inclusion of facilitating strategies is crucial. Simulated practice leads to the acquisition of fundamental skills, as does the assignment of a nursing supervisor/tutor and receiving feedback on the conducted tasks. In addition to overcoming the difficulties experienced, these strategies also allow developing resilience and coping mechanisms, which help prevent burnout and the adverse effects caused by the high staff turnover rate between services.
Keywords: Integration; Difficulties; Strategies; Nurse; Critically Ill Person
INTRODUCTION
Nowadays, the constant social, professional and institutional changes pose challenges to health institutions, particularly with regard to the management of human resources1.
The beginning of the career and the high rate of staff turnover between services are especially challenging realities for nursing professionals. Since they are usually required to sign short-term contracts, this implies a frequent integration processes. The acquisition of specific skills, namely within the context of care for the person in critical condition, is essential.
Regarding clinical nursing practice, Benner2 defines 5 expertise levels: “novice”, “advanced beginner”, “competent”, “proficient” and “expert”. In this respect, a nurse who is an “expert” in a given nursing context, will become an “advanced beginner” when moving to a new context, since he/she has already experienced real situations and is able to identify “significant factors that are replicated in identical situations”2.
Due to their characteristics, Intensive Care Units (ICUs) and other critical care services are, themselves, stressful places3. Professionals working there are confronted, on a daily basis, with situations of severe illness, pain, death and the need to make prompt decisions that may be influenced by time pressure3. It has been observed that these aspects, together with the frustration felt, at times, by professionals who are unable to restore a patient's health - and, thus, also their interpersonal relationship - can lead to anxiety and depression.
In a study conducted with 117 professionals, work overload and the lack of staff were reported as the most stressful factors in an ICU3. But, in emergency services, there are other unexpected and challenging situations capable of contributing to the nurses' exhaustion and fatigue4. Namely, the stress involved in emergent care has been reported to increase the nurses' emotional and work overloads4. In this regard, integration is decisive to the nurses' successful adaptation to the institution, while simultaneously allowing the further development of skills, the attainment of self-confidence and the strengthening of their professional identity5.
A critically ill patient is a person whose life is threatened by failure, or imminent failure, of one or more vital functions and whose survival depends on advanced means of surveillance, monitoring and therapy6.
In view of this problem, the adequate integration of nurses in care provision to critically ill patients is an increasing concern. Establishing a proper integration process is crucial for the nurses' successful adaptation to the new service, ensuring the quality and safety of the provided care. It is therefore essential to understand the difficulties felt, as well as the strategies employed to facilitate their integration process.
In order to understand the current “state of the art” on this matter, we conducted a survey and the critical appraisal of the related evidence. The majority of the articles addressed, mainly, the strategies employed to facilitate the nurses' integration process7-9. However, some works also addressed the difficulties experienced by nurses, as well as the skills required to provide a high-quality care to the critically ill9-11. In this regard, we believe there is a gap in the articulation between the main difficulties and the primary strategies used to support the nurses' integration.
In view of the above, we envisioned a thorough study on this matter, which would be useful and an added value for nurse managers, multidisciplinary teams and nurses seeking integration, by allowing to answer the following research questions:
Which difficulties are usually experienced by nurses during their integration in critical care services?
Which strategies facilitate the nurses' integration in critical care provision?
MATERIALS AND METHODS
To perform a preliminary analysis of the “state of the art”, we used the PubMed® database and employed the following descriptors: “Nurs*”, “Critical Care” and “Integration”. The search results revealed a low number of recent scientific papers associated with this subject, most of them referring to articles with a low level of evidence. An a priori protocol was prepared, following the methodology proposed by the Joanna Briggs Institute (JBI). This helped to conduct the first research stage, by allowing the organization of the information gathered.
Given the apparent knowledge gap, we considered pertinent to more accurately map the phenomenon12), by conducting a scoping review that allowed analyzing the existing literature, in order to map and summarize the existing evidence on the topic13. Given its importance, this work's relevance became clear and we proceeded to define the eligibility criteria, based on the PCC mnemonic. In this regard, we considered the following inclusion criteria: as Population (P), the Nurses; as Concept (C), the difficulties experienced and the strategies used to facilitate their integration; as Context (C), the provision of care to critically ill patients. On the other hand, we considered the following as exclusion criteria: regarding Population, works mentioning health professionals other than nurses; concerning Concept, articles referring to financial costs and work satisfaction; with respect to Context, studies related to COVID-19, as well as palliative or “end-of-life” care, pain management, organ donation, specific procedures and pediatrics.
We hope this scoping review may act as a precursor to future research, namely as a starting point for a subsequent systematic review12,14.
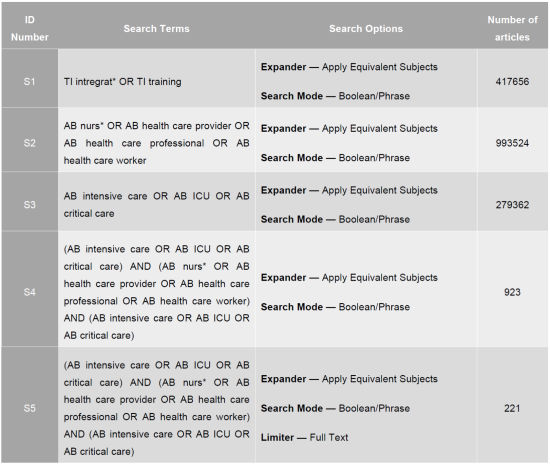
A strategy was defined for the Boolean search, which consisted in performing a preliminary assessment to find the appropriate health descriptors, using the MeSH and DeCS indexing tools. Several “subject” descriptors were defined right from the start, with some synonymous words and concepts having emerged during the preliminary analysis of the “state of the art”, as well as during the first stage of the database search. Other descriptors were found in articles freely available at the “Open Access Scientific Repository of Portugal” (“Repositório Científico de Acesso Aberto de Portugal”, RCAAP).
The strategy adopted to carry out the database search consisted in combining the different descriptors with the Boolean operators “AND” and “OR”, as presented in Appendix I, until the following sequence was established: (AB intensive care OR AB critical care) AND (AB nurs* OR AB health care provider OR AB health care professional OR AB health care worker) AND (TI Integrat* OR TI training).
The search encompassed the following databases: CINHAL® Complete; MEDLINE® Complete; Nursing & Allied Health Collection™: Comprehensive Edition; Cochrane Plus Collection; Library, Information Science & Technology Abstracts (LISTA); and MedicLatina™. We considered pertinent the addition of RCAAP to the previous list, as this allowed locating evidence that had not been published in scientific journals - and that eventually led to the inclusion of three freely available articles in the final sample.
We decided to include articles written in Portuguese, English, Spanish or French, and published until May 2020. Still regarding the publishing date, given the scarce evidence available on the topic, it was determined to establish no lower limit.
The following types of study were favored: primary studies, secondary studies, and opinion articles. The articles' availability in full text was initially considered a limiting factor. However, during the search, one relevant article was identified which was not available in full text and, after contacting its authors, we were kindly granted access, in order to include it in our research.
Three independent reviewers contributed to the final sample's selection, by reading the eligible articles' title, abstract and full text. The bibliographic references found in the selected articles were also considered throughout this process. Unanimity among the research team was required for article inclusion.
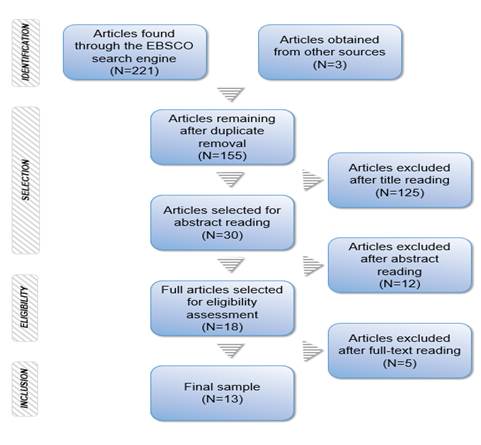
The sample selection process was systematized, using a PRISMA (“Preferred Reporting Items for Systematic Reviews and Meta-Analyses”) flow diagram, which is presented further on, in Figure 1.
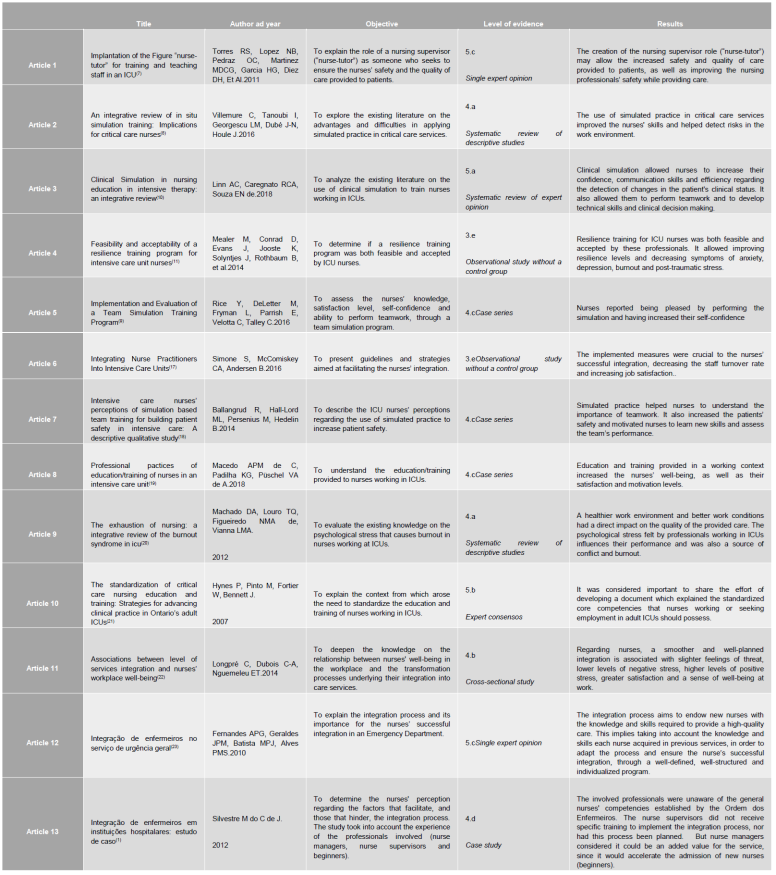
Subsequently, several Tables were prepared with the purpose of organizing the extracted data. Table 1 was filled in immediately after performing the full-text reading of the articles included in the sample, discriminating them by title, author(s) and year, objective, level of evidence and findings.
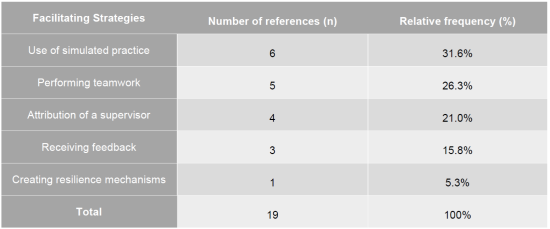
Tables 2 and 3 were elaborated afterward, during the data collection stage, with the intent of listing the main difficulties experienced by nurses (Table 2) and the strategies facilitating their integration (Table 3). They also discriminate the number of times each characteristic is mentioned in the articles, thus synthesizing the findings that directly relate to the objective and purpose of the present work15.
RESULTS
The search was carried out between August and October 2020. Afterward, the obtained data was extracted and organized as a descriptive narrative.
The initial search allowed identifying 224 eligible works. Form these, only 155 remained after removing the duplicates. Subsequently, 125 articles were excluded while performing title reading. They either addressed specific techniques and procedures, for instance Extracorporeal Membrane Oxygenation (ECMO) and dialysis, employed metrics such as the Nursing Activities Score (NAS), referred to palliative and “end-of-life” care provision or were related to the SARS-CoV-2 pandemic.
Thus, only 30 articles were selected for abstract reading. From these, 12 works were excluded because the population under study comprised nursing students or other health professionals or because they focused primarily on professional skills. Furthermore, we also excluded articles whose context was specific to a particular country.
Hence, 18 articles remained for full-text reading. Five of these were eliminated, because they focused on job satisfaction, financial costs, academic curriculum or the benefits of employing an e-learning methodology. This resulted in a final sample consisting of 13 articles. As aforementioned, Figure 1 systematizes the selection process, using a PRISMA flow diagram.
As previously mentioned, Table 1, which is exhibited below, portrays the final sample by presenting the articles' title, author(s) and year of publication, objectives and findings, and level of evidence, according to the JBI methodology16.
As mentioned previously, Tables 2 and 3 present, respectively, the different difficulties reported by nurses and the strategies employed to facilitate their integration. In both Tables, we have defined the number of references (n) as the amount of times each characteristic was addressed in the 13 articles comprising the sample. The relative frequency represents the corresponding percentage.
DISCUSSION
Critical care provision represents a highly complex environment within health-care services and requires professionals with advanced skills10, making it essential to understand which are the main difficulties experienced by nurses and which strategies facilitate their integration process, in order to enable them to provide a high-quality care.
The studies' analysis revealed that the main difficulty experienced by nurses was the existence of communication issues with the team, as well as with the critically ill patients and/or their relatives. It was also observed that poor communication increased the likelihood of nurses making mistakes that affected the quality of the provided care9. Stress was also considered a predominant difficulty, since critical care services consist of environments where daily confrontation with ethical and moral dilemmas occur11. Dealing with complex health conditions, as well as with intricate procedures and/or techniques, implies articulating between theoretical and practical knowledge. This requires the development of specific skills, as well as the acquisition of prompt and effective decision-making capabilities10. Work overload is directly related to the quality and safety of the provided care, since the nurses' work time is partially spent handling the existent differentiated technology19, e.g., when administering continuous venovenous hemodiafiltration or applying ECMO. Staff turnover between services is frequent in critical care settings, which hinders the ability to retain qualified nurses11. Finally, dealing with a patient's death, and/or with organ donation planning, may require appropriate counseling, as well as the development of coping mechanisms11.
While analyzing the articles' findings it was possible to deduce that the abovementioned difficulties acted as precursors, leading to the implementation of facilitating strategies, with respect to the integration process.
The importance of specialized training in critical care provision was considered as the main facilitating strategy. In this regard, the use of simulated practice, i.e., practice through the simulation of real-life issues, allowed the professionals to raise their confidence, to enhance team communication and to have the necessary awareness to detect complications earlier8)(9)(10. The second most relevant strategy was performing teamwork. This allowed increasing the effectiveness and safety of the provided care by permitting the various team members to complement (and benefit from) each others' knowledge8)(9)(10)(18. Another strategy mentioned as fundamental was the assignment of an expert nurse supervisor/tutor1,7. Receiving feedback through debriefing meetings was also reported as leading to the acquisition of important knowledge1,8. Finally, the literature highlights the creation of resilience mechanisms, such as raising self-awareness, providing self-care and ensuring personal well-being, as ways of protecting nurses from the negative effects of high levels of stress at their workplaces11)(20)(22.
In this scope, ensuring the nurses' integration into critical care services is vital to overcome adversity. This is especially relevant given the inherent complexity associated with critical care provision and the need for skilled professionals who respond efficiently to the diverse health-illness situations, by using different procedures/techniques, mastering the technologies and dealing with care systematization19. The integration process should begin with the assignment of a nurse supervisor/tutor to the new nurse. The former is responsible for monitoring the latter and should maintain this duty throughout the entire integration period, so as to enable the harmonization and strengthening of the interpersonal relationship1. Ultimately, the supervisor's role is to ensure an improvement in the quality of the provided care and the safety of the new nurse7. To accomplish this, the tutor must possess certain characteristics, namely, effective training skills and proven experience in care provision to the critically ill1)(7)(23. Preferably, the nursing supervisor should be present in the morning shift and should not be assigned many tasks related to care provision, unless the service team's needs demand so1,7.
It is known that the integration period does not have a fixed timeframe, varying from service to service, and according to the contingencies in which the integration process occurs1,23.
It is also recognized that nurses are professionally challenged when transitioning from one service to another, with newly admitted professionals usually experiencing higher levels of anxiety and stress1. This may be due to their lack of familiarity with the new team and, thus, their concern about being accepted by the senior team members. In addition, there is also the change of professional identity and the confrontation with new scenarios, new techniques and procedures1. Other stress sources related to the professionals' sense of maladjustment include: lack of formal planning with respect to the integration process, little involvement of the family/significant other in decision making, scarcity of interdisciplinary support and divergent care provision philosophies22.
The lack of team communication may lead to errors in care provision. According to a study by the Joint Commission, communication issues accounted for about 60% of the cases reported between 2011 and 20138. It is, thus, acknowledged that improving teamwork - and, thus, team communication - can prevent many adverse events. Interdisciplinary team training can facilitate this process by including simulation as an emerging teaching strategy, aimed at enhancing the professional skills and reinforcing the collaborative practice. This, in its turn, allows increasing the quality of the provided care, as well as both the patient's and the professional's safety8.
Furthermore, recreating real-life scenarios allows professionals to develop, in a controlled manner and within a safe environment, the clinical reasoning they might apply in situations where a patient's clinical condition worsens. As such, it allows them to increase both their knowledge and their self-confidence10, while also contributing to behavioral improvement and skill development, related to: collaboration, communication, leadership, self-efficacy, decision making, responsibility, confidence in one's role, and situational awareness, which favors the early detection of complications8,10. For those being trained, simulated practice is a more effective strategy than directly facing real-life situations, since it allows making mistakes and receiving subsequent feedback on the performance, without threatening the patients' lives. Besides providing experience and safety, it also facilitates decision making in real-life scenarios, thus improving the services' results10. It is, therefore, acknowledged that employing simulated practice, followed by debriefing/receiving feedback, benefits the nurses' learning process.
On a related matter, health care institutions frequently hire human resources on a short-term basis1. This leads to a high staff turnover rate and to the services' inability to retain highly-qualified professionals. This situation frequently occurs in critical care services, where annual turnover rates can range between 25% and 60%11. Such high rates are due to the fact that nurses view those services as stressful. When working there, they usually face tense situations, high mortality and morbidity rates, daily confrontations with ethical and moral dilemmas, scenarios involving organ donation and the need to deal with grieving relatives11,20.
Consequently, nurses tend to develop psychological disorders, such as anxiety, depression, burnout syndrome, and post-traumatic stress11. In such circumstances, resilience training is seen as crucial to their positive adaptation to such constraints.
In addition, given the increasing need for nursing professionals in the various critical care services, it is important to ensure their successful integration. In this context, adequate planning is essential for the professionals' training, as well as for retaining them in those services1)(21)(23.
Furthermore, a healthier work environment and better working conditions have a direct impact on the quality of the provided care and, ultimately, on the patients' health (20. It is also recognized that feelings of well-being, satisfaction and motivation are important for the nurses' learning and training at their workplaces1,19.
CONCLUSION
The findings obtained through this research allowed us to answer the initial questions. The main difficulties experienced by nurses during their integration in care provision to critically ill patients were the following: communication issues with the team, as well as with patients and/or their relatives; stress; dealing with complex health conditions, as well as with intricate procedures and/or techniques; work overload; high staff turnover rate between services and also dealing with a patient's death and/or with organ donation planning.
After analyzing the articles' content it was possible to conclude that those difficulties acted as precursors, leading to the implementation of facilitating strategies, with respect to the integration process. These included: the use of simulated practice, performing teamwork, being supervised by a nursing tutor, receiving feedback and also developing resilience mechanisms.
We believe this study may present some limitations with respect to the diversity of available evidence, since extending the search to additional databases might have provided other important contributions to our findings. As for the database search itself, the only limiter employed was the free availability of the articles in full text.
In conclusion, the integration process requires planning to define essential aspects of the care model and this can be achieved through the development of comprehensive strategies and programs. In this regard, the use of simulated practice allows nurses to acquire a set of skills that are crucial to provide a high-quality care. Equally important is the assignment of a nursing supervisor/tutor, capable of providing valuable feedback on the performed work. In addition, nurses also overcome the experienced difficulties by building resilience and developing coping mechanisms that help them prevent burnout and lower the frequency of staff turnover between services.
In view of the above, we believe that the present work may serve as a foundation for future research. Furthermore, the challenge remains for the development of primary studies aimed at better understanding this topic, as it constitutes a transversal and pertinent phenomenon in the field of Nursing, despite having been little studied so far.
Financing:
FCT-Portugal, UIDB/04279/2020
REFERENCES
1. Silvestre M do C de J. Integração De Enfermeiros Em Instituições Hospitalares: Estudo De Caso. Universidade de Aveiro; 2012. [ Links ]
2. Benner P, Queiroz AA, Lourenço B. O Modelo Dreyfus de Aquisição de Competências Aplicado À Enfermagem. In: De iniciado a perito: excelência e poder na prática clínica de enfermagem. Coimbra: Quarteto Editora; 2001. p. 42-63. [ Links ]
3. Ballester-Arnal R, Gómez-Martínez S, Gil-Juliá B, Ferrándiz-Sellés MD, Collado-Boira EJ. Burnout y factores estresantes en profesionales sanitarios de las unidades de cuidados intensivos. Rev Psicopatología y Psicol Clínica. 2016;21(2):129-36. [ Links ]
4. Yu H, Qiao A, Gui L. Predictors of compassion fatigue, burnout, and compassion satisfaction among emergency nurses: A cross-sectional survey. Int Emerg Nurs. 2021;55:100961. [ Links ]
5. Taveira CAO. Enfermagem ... Um Percurso No Saber. Universidade Católica Portuguesa Porto; 2011. [ Links ]
6. Diário da República. Regulamento de competências específicas do enfermeiro especialista em Enfermagem Médico-Cirúrgica na Área de Enfermagem à Pessoa em Situação Crítica. Regulamento n.o 429/2018 Portugal: Ordem dos Enfermeiros; 2018 p. 19359-64. [ Links ]
7. Torres RS, Lopez NB, Pedraz OC, Martinez MDCG, Garcia HG, Diez DH, et al. IMPLANTATION OF THE FIGURE "NURSE-TUTOR" FOR TRAINING AND TEACHING STAFF IN AN ICU. Salamanca; 2011. [ Links ]
8. Villemure C, Tanoubi I, Georgescu LM, Dubé J-N, Houle J. An integrative review of in situ simulation training: Implications for critical care nurses. Can J Crit Care Nurs. 2016;27(1):23-31. [ Links ]
9. Rice Y, DeLetter M, Fryman L, Parrish E, Velotta C, Talley C. Implementation and Evaluation of a Team Simulation Training Program. J Trauma Nurs. 2016;23(5):298-303. [ Links ]
10. Linn AC, Caregnato RCA, Souza EN de. Clinical simulation in nursing education in intensive therapy: an integrative review. Rev Bras Enferm. 2019;72(4):1061-70. [ Links ]
11. Mealer M, Conrad D, Evans J, Jooste K, Solyntjes J, Rothbaum B, et al. Feasibility and acceptability of a resilience training program for intensive care unit nurses. Am J Crit Care. 2014;23(6):e97-105. [ Links ]
12. Apóstolo JLA. Síntese da evidência no contexto da translação da ciência. Escola Superior de Enfermagem de Coimbra, editor. Coimbra; 2017. 135 p. [ Links ]
13. Tricco AC, Lillie E, Zarin W, O'Brien K, Colquhoun H, Kastner M, et al. A scoping review on the conduct and reporting of scoping reviews. BMC Med Res Methodol. 2016;16:1-11. [ Links ]
14. Munn Z, Peters MDJ, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18:1-8. [ Links ]
15. The Joanna Briggs Institute. The Joanna Briggs Institute Reviewers' Manual 2015: Methodology for JBI Scoping Reviews. The Joanna Briggs Institute. Adelaide: The Joanna Briggs Institute; 2015. p. 1-24. [ Links ]
16. Joanna Briggs Institute Levels of Evidence and Grades of Recommendation Working Party. JBI Levels of Evidence. Adelaide: The Joanna Briggs Institute; 2014. p. 1-5. [ Links ]
17. Simone S, McComiskey CA, Andersen B. Integrating Nurse Practitioners Into Intensive Care Units. Crit Care Nurse. 2016;36(6):59-69. [ Links ]
18. Ballangrud R, Hall-Lord ML, Persenius M, Hedelin B. Intensive care nurses' perceptions of simulation-based team training for building patient safety in intensive care: A descriptive qualitative study. Intensive Crit Care Nurs. 2014;30(4):179-87. [ Links ]
19. Macedo APM de C, Padilha KG, Püschel VA de A. Professional practices of education/training of nurses in an intensive care unit. Rev Bras Enferm. 2019;72(2):321-8. [ Links ]
20. Machado DA, Louro TQ, Figueiredo NMA de, Vianna LMA. THE EXHAUSTION OF NURSING : A INTEGRATIVE REVIEW OF THE BURNOUT SYNDROME IN ICU. Rev Pesqui Cuid é Fundam online. 2012;4(4):2765-75. [ Links ]
21. Hynes P, Pinto M, Fortier W, Bennett J. The standardization of critical care nursing education and training: Strategies for advancing clinical practice in Ontario's adult ICUs. Dyn. 2007;18(1):23-7. [ Links ]
22. Longpré C, Dubois C-A, Nguemeleu ET. Associations between level of services integration and nurses' workplace well-being. BMC Nurs. 2014;13:1-12. [ Links ]
23. Fernandes APG, Geraldes JPM, Batista MPJ, Alves PMS. Integração de Enfermeiros no Serviço de Urgência Geral. Sinais Vitais. 2010;92:50-5. [ Links ]
Received: April 29, 2021; Accepted: November 20, 2021











 texto em
texto em