My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Enfermería Global
On-line version ISSN 1695-6141
Enferm. glob. vol.21 n.67 Murcia Jul. 2022 Epub Sep 19, 2022
https://dx.doi.org/10.6018/eglobal.502051
Reviews
Effective communication strategies among health professionals in Neonatology: an integrative review
1Federal University of Piauí - Campus Amilcar Ferreira Sobral. Floriano- PI. Brazil
2Colegio Técnico de Floriano (CTF/UFPI). Brazil
Objective:
To identify strategies available in the scientific literature on effective communication among health professionals in Neonatology.
Methods:
This is an integrative review carried out from April to August 2021, by consulting the following databases: BDEnf, LILACS, IBECS, MEDLINE/PUBMED, Scopus and Science Direct. Studies whose titles and abstracts were related to effective communication strategies among health professionals to promote safety in Neonatology were included, and duplicates and integrative/systematic/bibliographic/narrative reviews were excluded.
Results:
The strategies aimed at promoting effective communication found in this review were SBAR, P.U.R.E and handoffs.
Conclusions:
These strategies are conFigured as effective in improving communication between the multidisciplinary teams in Neonatology, reflecting positively on quality of care and on patient safety.
Keywords: Communication; Patient Safety; Neonatology; Health Personnel
INTRODUCTION
Effective communication among health professionals is an indispensable factor to ensure patient safety in the health services1, especially in the Neonatology scope2. The Ministry of Health, following the recommendations of the World Health Organization (WHO), through the World Alliance for Patient Safety, listed effective communication as the second international goal as a guarantee for quality in care and patient integrity within health units3.
When there is a deficit in communication, the possibility of professional errors increases and, as a consequence, the emergence of adverse events intensifies2. The Joint Commission research study that analyzed a total of 936 sentinel events during 2015 confirms that ineffective communication is the root cause in over 70% of the serious medical errors, including perinatal injuries and deaths4,5.
Among the main obstacles to effective communication are overvaluation of information of a clinical nature, crossing of messages regarding service information and personal information, lack of motivation6, lack of time, shortage of personnel, lack of standardization of the information, incompetence or lack of knowledge about the importance of such action7, excessive or reduced amount of information; limited opportunity for possible questions; inconsistent quality of information; omitting or passing on erroneous information; illegible records; and interruptions and distractions caused by the use of telephones, in addition to unnecessary interruptions by family members8.
In the scope of the neonatal intensive unit, it is also evident that the many noises from the monitors, delays and early departures of professionals, crying of the newborns, parallel conversations between professionals and complications with patients interfere in the process of effective communication between the health teams9.
Following this direction, the assistance provided to newborns, as it refers to a heterogeneous group, can be considered a significant challenge for health professionals with regard to effective and safe communication, with the need to invest in an organizational culture based on objectives and strategies with effective communication configurations10.
In order to overcome barriers that prevent Effective Communication among health professionals, a number of studies point to communication skills training programs, practical simulations and standardized ways to present the patient's information2,11. In addition to that, among the main tools to qualify communication are integration of the care team, practice of information double-check, use of computerized systems, systematic and judicious handoffs between professionals, multidisciplinary rounds, care transfer between sectors and regular team meetings12.
Given the understanding that effective communication is indispensable to ensure safety and quality of care, especially for newborns, in addition to favoring an environment with pleasant and respectful human relationships for the work process13, the objective was to identify strategies available in the scientific literature on effective communication among health professionals in Neonatology.
METHOD
The research method used was the integrative literature review, which covers the study of theoretical and empirical literature, as well as the mapping of studies with different methodological approaches14.
For developing this research, six stages were followed, described below: 1) Choice and definition of the topic and definition of a research hypothesis or question, 2) Sampling or search in the literature, definition of inclusion and exclusion criteria, 3) Organization and summarization of the information to be extracted from the studies selected and categorization of the studies, 4) Evaluation of the studies included in the review, 5) Interpretation of the results and suggestions for future research studies, and 6) Presentation of the review/knowledge synthesis15.
Stage 1, referring to the choice and definition of the theme and to the definition of a research hypothesis or question, was built and organized according to the PICo strategy (P - Population; I - Intervention/area of interest; Co - Context16, considering the following structure: P - Patient safety; I - Effective communication; Co - Neonatology. Thus, the following guiding question arose: “What effective communication strategies are used among health professionals in Neonatology?”.
Stage 2 corresponds to sampling or search in the literature, and to definition of inclusion and exclusion criteria. For selecting the publications, the following inclusion criteria were established: primary studies, with no time frame, in Portuguese, English and Spanish, and which use strategies to improve communication among health professionals in the neonatal unit. Book chapters, PhD theses, master's dissertations, case studies, experience reports, technical reports, editorials and the different types of reviews were excluded.
Stage 3 refers to the organization and summarization of the information to be extracted from the studies selected and the categorization of the studies. It is at this moment that a data collection instrument is used to gather and summarize the most important information to be extracted from the studies selected, and thus build a database that is easy to access and manage. A data collection instrument was developed using the following items: authors/year of publication, language, study objectives, type of study, level of evidence, main findings and gaps/limitations15.
The survey was carried out between April and August 2021. The search was carried out via the Coordination for the Improvement of Higher Level Personnel (Coordenação de Aperfeiçoamento de Pessoal de Nível Superior, CAPES) portal with access by the Federal University of Piauí (Universidade Federal do Piauí, UFPI) in the following databases: Banco de Dados em Enfermagem(BDEnf),Literatura Latino-Americana e do Caribe em Ciências da Saúde(LILACS) andÍndice Bibliográfico Español en Ciencias de la Salud(IBECS) viaBiblioteca Virtual em Saúde(BVS), Medical Literature Analysis and Retrieval System Online (MEDLINE) via the US National Library of Medicine (PUBMED), Scopus and Science Direct, both by Elsevier. Choice of these data was due to their academic-scientific relevance.
The controlled descriptors used in the search are inserted in the Descriptors in Health Sciences (Descritores em Ciências da Saúde, DeCS) Database and in the Medical Subject Headings (MeSH). They are the following: “Patient Safety”; “Communication”; “Neonatology”. The uncontrolled terms (keywords), synonyms of the controlled descriptors, were as follows: “Effective communication” and “Comunicação efetiva”. It is emphasized that these terms were listed after an exhaustive analysis of synonyms and combinations that corresponded to the search content. To systematize sample collection, the Boolean operators "OR" and "AND” were used, opting for different search strategies, considering that the databases have different peculiarities and characteristics.
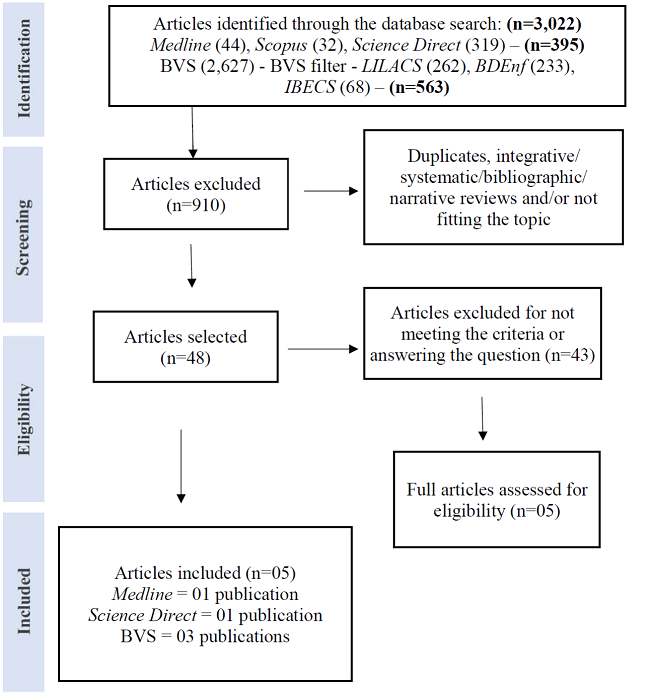
During the process of identification, selection and inclusion of primary studies, a total of 3,022 articles were identified. 395 publications were obtained in the MEDLINE, Scopus and Science Direct databases and 2,627 publications were from BVS. Of the 395 publications, 44 were found in the MEDLINE database, 32 in Scopus, and 319 in Science Direct. In BVS, due to the number of articles, it was decided to use theLILACS(262),BDEnf(233) andIBECS(68) filters, leaving 563 publications. Therefore, 958 publications were analyzed in this first stage.
Subsequently, selection was performed, considering, at first, as potentially eligible, the studies whose titles and abstracts were related to effective communication strategies among health professionals to promote safety in Neonatology and excluding duplicates and integrative/systematic/bibliographic/ narrative reviews; in this stage, 48 publications were chosen to be read in full, 16 in MEDLINE, five (5) in Scopus, 14 in Science Direct, three (3) in LILACS, two (2) in BDEnf, three (3) in IBECS and five (5) in LILACS and BDEnf.
For final selection, the studies were read in full and meticulously, verifying if they met the pre-established inclusion and exclusion criteria (MENDES; SILVEIRA; GALVÂO, 2008). Thus, 43 studies were excluded, leaving five (5) studies, one (1) in MEDLINE, one (1) in Science Direct and three (3) in BVS (LILACS/BDEnf - 2; IBECS - 1), which were included in the sample of this review.
The research was carried out independently by two reviewers, in order to guarantee methodological rigor and reliability of the results, in order to minimize probable systematic errors or measurement bias of the studies, due to failures in the interpretation of the results as well as in their design. For this, the proposed script was used in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) methodology and is represented in the followingflowchart.
Flowchart 1. Search strategy for selecting the articles included in the review, considering the recommendations set forth in the Preferred Reprinting Items for Systematic Reviews and Meta-Analyses(PRISMA)
The level of evidence of the articles was determined according to the classification proposed by the Joanna Briggs Institute - JBI (2014): Level 1 - Experimental Projects (Level 1.a - Systematic review of Randomized Controlled Clinical Trials (RCCTs); Level 1.b - Systematic review of Randomized Clinical Trials (RCTs) and other study designs; Level 1.c - RCTs; Level 1.d - Pseudo-RCTs); Level 2 - Quasi-experimental designs (Level 2.a - Systematic review of quasi-experimental studies; Level 2.b - Systematic review of quasi-experimental designs and other smaller studies; Level 2.c - Prospective quasi-experimental controlled study; Level 2 .d - Pre-test - post-test or historical/retrospective control group study);
Level 3 - Observational - Analytical Projects (Level 3.a - Systematic review of comparable cohort studies; Level 3.b - Systematic review of comparable cohort and other lower study designs; Level 3.c - Cohort study with control group; Level 3.d - Case-controlled study; Level 3.e - Observational study without a control group); Level 4 - Observational - Descriptive Studies (Level 4.a - Systematic review of descriptive studies; Level 4.b - Cross-sectional study; Level 4.c - Case series; Level 4.d - Case study); and Level 5 - Experts' Opinion and Bench Research (Level 5.a - Systematic Review of Experts' Opinion; Level 5.b - Experts' Consensus; Level 5.c - Bench research/single expert opinion)17.
The studies included in the review were selected and analyzed with detail and rigor, in Stage 4, looking for explanations for divergent or contradictory results18. In Stage 5, Interpretation of the results and suggestions for future research studies, after a critical analysis of the studies, the reviewer performed an interpretation of the results, a comparison with theoretical knowledge, considerations, conclusions and implications arising from the integrative review. It corresponds to the phase of discussion of the results in conventional research15,18.
In Stage 6, presentation of the review/knowledge synthesis contains the elaboration of the document that should analyze the characteristics of the stages examined and the main results shown in the analysis of the articles included. In this way, a thorough review of all the articles chosen was carried out, which made it possible to interpret the data and, with that, provided a summary of the existing knowledge. In this integrative review, the analysis of the results was performed in a descriptive way, with a synthesis of each study included in the sample. Such data were grouped and organized in the order in which they were listed. The ethical and legal aspects were ensured, guaranteeing legitimacy of the authors, who were cited at all times when the articles were mentioned.
RESULTS AND DISCUSSION
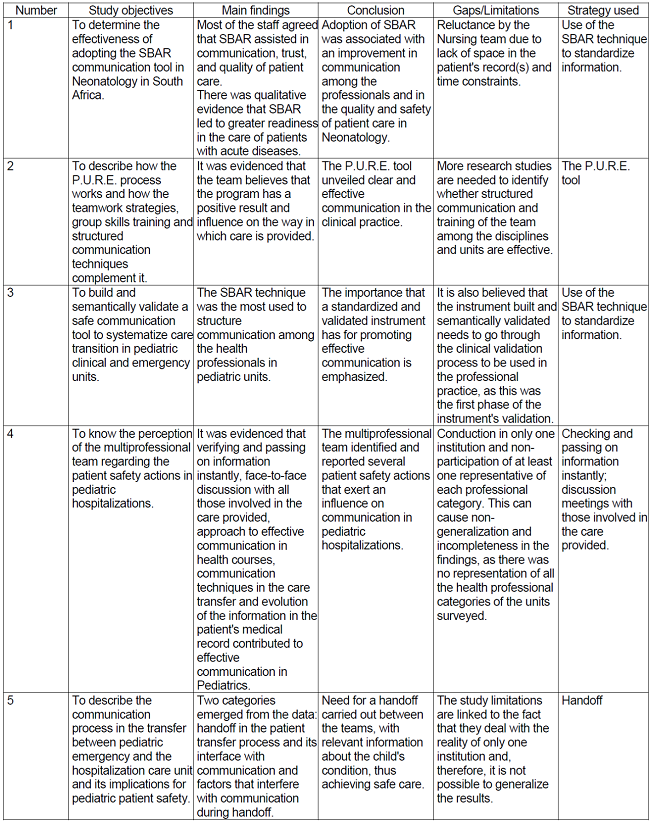
The five articles selected are described below, withChart 1related to the variables of characterization of the studies: database, authors/year of publication, type of study, level of evidence and language; andChart 2with the following variables: study objectives, main findings, conclusion, gaps/limitations and strategy used to improve communication among health professionals.
It was evidenced that the studies are indexed in three databases, most of them in BVS (n=3; 60%), published in 2012 and 2021 (n=1; 20% each year), descriptive study type (n=4; 80%), with level of evidence 4 (n=4; 80%) and in the Portuguese language (n=3; 60%).
The reduced number of studies included in this review can be justified by the scarcity of research studies on the theme of effective communication among health professionals carried out in a Neonatology environment, which shows that this topic should be disseminated in studies of this nature; in addition to that, the levels of evidence identified show lack of studies with strong scientific evidence.
The studies that comprised this review evidenced that the effective SBAR (Situation, Background, Assessment and Recommendation) communication strategy is the most used to improve care in the hospital environment (n=2; 40%).
Adoption of the SBAR tool is associated with an improvement in communication among the professionals and in the quality and safety of patient care in Neonatology (A1), in addition to being an important standardized and validated instrument for promoting effective communication among health professionals in pediatric units (A3)19,21.
SBAR (Situation, Background/Context, Assessment and Recommendation) is a standardized communication tool recommended by the Joint Commission, the Agency for Healthcare Research and Quality (AHRQ), the Institute for Health Care Improvement (IHI), the World Health Organization (WHO) and the United Kingdom National Health Service. It is a structured method for communicating critical information that requires immediate attention and action, contributing to effective management escalation and increased patient safety in Neonatology, reducing the barrier to effective communication across different hierarchies and staff levels, and acting as a reminder that encourages prior preparation for communication19.
It was originally developed to be implemented in acute health care settings with the intention of improving nurse-physician communication; however, it has also been shown to improve communication among other health professionals. Thus, other specialties adhered to use of the tool, such as Anesthesia, Surgery, Obstetrics, Emergency, Intensive Care, Pediatrics and Neonatology4.
A narrative review with studies that used the SBAR communication tool among health professionals in a health care setting also agrees that it is a reliable and validated communication tool that has shown a reduction in adverse events in a hospital setting, improved communication among health professionals and promoted patient safety. It also states that it was developed to structure conversations between physicians and nurses about situations that require immediate attention4.
An Italian study corroborates that using the SBAR tool in a hospital environment improves transfer of the patients' information between professionals from the multidisciplinary team and that it can be useful in monitoring the impact on patient safety, thus improving communication23.
Other effective communication strategies among health professionals in the hospital environment were also mentioned in this review (n=1; 20% each strategy), such as P.U.R.E. (Purposeful, Unambiguous, Respectful, Effective) - A220, verifying and passing on information instantly - A422and handoffs - A58.
P.U.R.E. is an acronym used to facilitate the communication process in the perinatal and neonatal environment and professional development, having the following meaning: Purpose - It is defined as a goal that is desired towards which an action is carried out; Unambiguous - Containing direct and clear words; Respectful - Treatment that shows honor, proper acceptance and courtesy; and Effective - Accurate communication between sender and receiver. P.U.R.E. intends to ensure that the message is delivered, understood, received and acted upon by professionals; in addition to that, it recognizes the contributions of each team member who uses it. It is a flexible approach that can incorporate other communication tools such as SBAR20.
The P.U.R.E. strategy was also used in the study by Veltman and Larison24, who identified communication failures as a significant cause of adverse outcomes in Obstetrics, emphasizing the importance of this strategy to conduct and monitor structured communications and existing relationships between the professionals. The participants on this study identified the importance of this team-building strategy as a positive force in improving communication in their unit.
In addition to this strategy, two studies were also cited that brought effective communication as an indispensable resource for patient safety, using, for this, handoffs in communication between the health professionals8,22.
A study emphasized handoff in the patient transfer process and its interface with communication and the factors that interfere with communication during this activity. With the results, it was observed that the consequences arising from failures in communication among hospital units and among teams can seriously compromise patient safety, causing a break in the continuity of care and treatment offered, highlighting the importance of communication as continuity of the care provided to the patient8.
Through Ordinance No. 529, the Ministry of Health instituted the National Patient Safety Program, which aims at promoting actions targeted at improving health care safety, including communication in the environment of the health services.25. Effective communication is an indispensable strategy to ensure patient safety and the main facilitators of effective communication are verifying and instantly passing on information, face-to-face discussion with all those involved in the care provided, an approach to effective communication in health courses, communication techniques in care transfer and evolution of the information in the patient's medical record22.
Among these failures, noise, excessive or reduced amount of information, limited opportunity for possible questions, inconsistent quality of information, omission or passing on of erroneous information, non-use of standardization, illegible records, interruptions and distractions caused by the use of telephones or by family members8stand out.
A study pointed out failure of communication and its standardization among health professionals, as well as the inadequate recording of information in the patient's medical record, as barriers to effective communication. In addition, they mentioned the following among the main tools to qualify communication and integration of the care team: practice of information double-check, use of computerized systems, systematic and judicious handoffs among professionals, multidisciplinary rounds, care transfer between sectors and regular team meetings12.
Some of the strategies used by the professionals to improve communication are as follows: planning of periodic meetings, focusing on performance assessments and feedback with the entire multidisciplinary team to point out problems in search of solutions. In addition to that, the team's recognition of destructive behaviors and openness to dialog were also cited as strategies for effective communication13.
These tools cited in the literature are part of the proposals for improvements in effective communication among health professionals in several studies found in the initial search; however, few studies apply this approach to the Neonatology area, which justifies the importance of this integrative review. Furthermore, although using different strategies to improve communication among health professionals, the results above point to the need to use standardized instruments as strategies for effective communication among them.
CONCLUSION
Based on the scientific production presented in thecorpusof this research, although there is an incipient number of studies on the theme involving effective communication strategies among health professionals in Neonatology, these strategies are conFigured as effective in improving communication among the multidisciplinary team members, especially when it comes to critically-ill patients.
Based on this premise, it is worth highlighting the strategies that aim at promoting effective communication found in this review, namely: SBAR, P.U.R.E. and handoffs. Thus, it reinforces the use of validated strategies, as they have psychometric properties.
Therefore, the magnitude regarding the use of standardized information through instruments is understandable, as it is proven effective for effective communication in health services, especially in Neonatology, positively reflecting on care quality and on patient safety.
It is therefore suggested to elaborate a standardized instrument of the checklist type that may come to be used as a tool to promote and sensitize health professionals as to the importance of effective communication in the Neonatology service. The strategies listed above will enable the creation of possible items that will compose the checklist for effective communication among health professionals.
REFERENCIAS
1. Marques JM, Alves LHP, Oliveira NS, Marta CB, Silva RCL. Safety culture and the communication process among nursing team members. Rev Enferm Atual In Derme. 2019 [cited 2021 Aug 09];87(25). doi: 10.31011/reaid-2019-v.87-n.25-art.219 [ Links ]
2. Vanderbilt AA, Pappada SM, Stein H, Harper D, Papadimos TJ. Increasing patient safety with neonates via handoff communication during delivery: a call for interprofessional health care team training across GME and CME. Adv Med Educ Pract. 2017[cited 2021 Mar 09];8:365-7. doi: 10.2147/AMEP.S129674. [ Links ]
3. Agência Nacional de Vigilância Sanitária (Anvisa). Assistência Segura: uma reflexão teórica aplicada à prática [Internet]. Brasília: Anvisa; 2017 [cited 2021 Aug 19]. Available from: https://www.saude.go.gov.br/images/imagens_migradas/upload/arquivos/2017-09/2017-anvisa---caderno-1---assistencia-segura---uma-reflexao-teorica-aplicada-a-pratica.pdf [ Links ]
4. Shahid S, Thomas S. Situation, Background, Assessment, Recommendation (SBAR) Communication Tool for Handoff in Health Care - A Narrative Review. Safety in Health 2018[cited 2021 Jul 29];4:7.doi: 10.1186/s40886-018-0073-1 [ Links ]
5. Yamada NK, Catchpole K, Salas E. The role of human factors in neonatal patient safety. Semin Perinatol. 2019[cited 2021 Jul 29];43(8):151174. doi: 10.1053/j.semperi.2019.08.003 [ Links ]
6. Calha A, Neto E, Grade L, Engenheiro O, Sapatinha S. Determining factors of communication effectiveness in nursing teams. Rev Rol Enferm. 2018[cited 2021 Aug 05];41(11/12):26-31. Available from: https://pesquisa.bvsalud.org/portal/resource/pt/ibc-179937 [ Links ]
7. Olino L, Gonçalves AC, Strada JKR, Vieira LB, Machado MLP, Molina KL et al. Effective communication for patient safety: transfer note and Modified Early Warning Score. Rev Gaúcha Enferm. 2019[cited 2021 Aug 06];40(esp):e20180341. doi: 10.1590/1983-1447.2019.20180341 [ Links ]
8. Silva MF, Anders JC, Rocha PK, Silva MOV, Souza S, Carneiro ES. Transfer between hospital units: implications of communication on pediatric patient safety. Rev Enferm UFPE. 2017[cited 2021 Aug 05];11(10):3813-20. [ Links ]
9. Gonçalves MI, Rocha PK, Souza S, Tomazoni A, Paz BPD, Souza AIJ. Patient safety and change-of-shift reporting in neonatal intensive care units. Rev Baiana Enferm. 2017[cited 2021 Aug 09];31(2):e17053. doi: 10.18471/rbe.v31i2.17053 [ Links ]
10. Duarte SCM, Azevedo SS, Muinck GC, Costa TF, Cardoso MMVN, Moraes JRMM. Best Safety Practices in nursing care in Neonatal Intensive Therapy. Rev Bras Enferm 2020[cited 2021 Nov 12];73(2):e20180482. doi: 10.1590/0034-7167-2018-0482 [ Links ]
11. Nogueira JWS, Rodrigues MCS. Effective communication in teamwork in health: a challenge for patient safety*. Cogitare Enferm. 2015[cited 2021 Feb 02];20(3):630-4. doi: 10.5380/ce.v20i3.40016 [ Links ]
12. Biasibetti C, Hoffmann LM, Rodrigues FA, Wegner W, Rocha PK. Communication for patient safety in pediatric hospitalizations. Rev Gaúcha Enferm. 2019[cited 2021 Aug 09];40(esp):e20180337. doi: 10.1590/1983-1447.2019.20180337 [ Links ]
13. Moreira FTLS, Callou RCM, Albuquerque GA, Oliveira RM. Effective communication strategies for managing disruptive behaviors and promoting patient safety. Rev Gaúcha Enferm. 2019[cited 2021 Aug 09];40(esp):e20180308. doi: 10.1590/1983-1447.2019.20180308 [ Links ]
14. Whittemore R, Knafl K. The integrative review: updated methodology. J Adv Nurs. 2005 [cited 2021 Jul 28];52(5):546-53. doi: 10.1111/j.1365-2648.2005.03621.x [ Links ]
15. Mendes KDS, Silveira RCCP, Galvão CM. Revisão integrativa: método de pesquisa para a incorporação de evidências na saúde e na enfermagem. Texto Contexto Enferm. 2008[cited 2021 Jul 28];17(4):758-64. doi:10.1590/S0104-07072008000400018 [ Links ]
16. Karino ME, Felli VEA. Enfermagem baseada em evidências: avanços e inovações em revisões sistemáticas. Ciênc Cuid Saúde. 2012[cited 2021 Aug 19];11(5):11-5. doi: 10.4025/cienccuidsaude.v11i5.17048. [ Links ]
17. JBI? Joanna Briggs Institute. Levels of evidence. [Internet] 2014 [cited June 1, 2018]. Available from: http://joannabriggs.org/jbi-approach.html#tabbed-nav=Levels-of-Evidence [ Links ]
18. Sousa LMM, Marques-Vieira CMA, Severino SSP, Antunes AV. A Metodologia de Revisão Integrativa da Literatura em Enfermagem. Revista Investigação em Enfermagem. 2017[cited 2021 Nov 12];2. Available from: https://repositorio-cientifico.essatla.pt/handle/20.500.12253/1311 [ Links ]
19. Raymond M, Harisson MC. The structured communication tool SBAR (Situation, Background, Assessment and Recommendation) improves communication in neonatology. S Afr Med. 2014[cited 2021 Jul 29];104(12):850-2. doi: 10.7196/samj.8684 [ Links ]
20. Gephart SM, Cholette M. P.U.R.E. Communication: A Strategy to Improve CareCoordination for High Risk Birth. Newborn Infant Nurs Ver. 2012[cited 2021 Aug 04];12(2):109-14. doi: 10.1053/j.nainr.2012.03.007 [ Links ]
21. Silva MF, Rocha PK, Echevarria-Guanillo ME, Bertoncello KCG, Souza S, Schneider KLK. Construction of the instrument for care transition in pediatric units. Texto Contexto Enferm. 2021[cited 2021 Aug 04];30:e20180206. 10.1590/1980-265X-TCE-2018-0206 [ Links ]
22. Biasibetti C, Rodrigues FA, Hoffmann LM, Vieira LB, Gerhardt LM, Wegner W. Patient safety in pediatrics: perceptions of the multi-professional team. Rev Min Enferm. 2020[cited 2021 Jul 27];24:e1337. doi: 10.5935/1415.2762.20200074. [ Links ]
23. Calza S, Mora RDRD, Subbrero M, Scelsi S. Validazione linguistico culturale di un questionario per valutare l'uso della tecnica SBAR nel setting ospedaliero. ANIARTI Associazione Nazionale Infermieri di Area Critica. 2020[cited 2021 Jul 29];37(3). Disponível em: https://scenario.aniarti.it/index.php/scenario/article/view/439 [ Links ]
24. Veltman L, Larison K. PURE conversations: Enhancing communication and teamwork. Journal of healthcare risk management. J Healthc Risk Manag. 2007[cited 2021 Oct 13];27(2):41-4. doi: 10.1002/jhrm.5600270208. [ Links ]
25. Ministério da Saúde (BR). Portaria nº. 529, de 1 de abril de 2013. Institui o Programa Nacional de Segurança do Paciente (PNSP) [Internet]. Diário Oficial da União. 1 de abril de 2013 [cited 2021 Aug 09]. Available from: http://bvsms.saude.gov.br/bvs/saudelegis/gm/2013/prt0529_01_04_2013.html [ Links ]
Received: November 22, 2021; Accepted: January 03, 2022











 text in
text in