My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Enfermería Global
On-line version ISSN 1695-6141
Enferm. glob. vol.22 n.69 Murcia Jan. 2023 Epub Mar 20, 2023
https://dx.doi.org/10.6018/eglobal.525701
Originals
Evolution of the stigma towards mental health in training health specialists in Asturias
1Área de Gestión Clínica de Salud Mental del Área Sanitaria III del Principado de Asturias. Asturias. España. carla25@outlook.es
2Servicio de Transformación y Gestión del Conocimiento de la Dirección General de Calidad, Transformación y Gestión del Conocimiento de la Consejería de Salud del Principado de Asturias. Asturias. España
Introduction:
Several studies have analysed social stigma among medical and nurse students or health care workers towards people with mental disorders. However, there is no evidence of social stigma training in residents during their specialised health training (FSE).
Objective:
This study aims to evaluate social stigma in residents in clinical specialities, the “anti-stigma” training during their residency, and its influence on the beliefs and attitudes they had in the first and last year of specialisation.
Materials and Methods:
A cross-sectional descriptive study in a sample of 250 residents of nursing, medicine, and clinical psychology: 141 in the first year of speciality and 109 in the last year, selected by random sampling proportional to the total number of residents in each year. The CAMI-S scale was used to measure social stigma, and a self-made questionnaire was used for sociodemographic variables. Both were created in the FORMS app and sent via email. The mean and standard deviation (SD) were obtained for “integration and contact”, “social distance”, “dangerousness and avoidance”, and overall stigma. Overall score for no stigma was between 80-100.
Results:
Response rate of 57.6%: 72.2% women, 64.6% 23-28 years old, 54.2% in the first year, 51.4% medical specialisation and 29.9% nursing. Only 20.1% had received “anti-stigma” training. Overall mean stigma of 86.7 (SD=8.5); 87.3 (SD=7.9) in the first year and 86.1 (SD=9.1) in the last year (P=0.398); 90.0 (SD=8.2) if they received training and 86.1 (SD=8.4) if they did not (p=0.027).
Conclusions:
Overall scores favourable to "anti-stigma" were obtained for people both in their first and last year of specialty. When there was "anti-stigma" training during residency, the results were even more favourable. It would therefore be beneficial to include content on "anti-stigma" in residency training programmes.
Keywords: Social stigma; mental health; residence; social change
INTRODUCTION AND RATIONALE
Throughout history, the concept of mental illness has changed, going from a magical and supernatural case study initially to the scientific-rational perspective we have today1,2.
The Royal Spanish Academy defines stigma as: “Disdain, affront and bad reputation”3. In mental health, its impact is twofold: first, personal stigma, such as the prejudice that people with mental illness turn against themselves, and second, social stigma, such as the reaction of the general population towards people with mental illness4.
This social stigma is marked by stereotypes, prejudices and discrimination that in a certain way help a majority group to categorise society and quickly identify those they may consider potentially dangerous.
In contrast, “anti-stigma” movements guide their efforts to normalise mental illness, seeking to eradicate stigma and associated discrimination in the media, education, health and labour market5,6.
Despite these movements and historical development, the stigma surrounding the mentally ill is still there: strange, dangerous, unpredicTable, they generate mistrust and compassion "from a distance". Even health personnel have maintained these beliefs by exercising their profession according to the political and social ideologies of the time1,7.
It is the patients themselves who report that their mental illness often takes up health care time when they attend primary care services, i.e., their mental illness somewhat eclipses the physical symptoms, losing their organic origin8.
Specialised health training, which can be accessed by nurses, psychologists, doctors, pharmacists, physicists, biologists and chemists, includes in its cross-disciplinary training plan courses to increase their bioethical knowledge so as to lead them to act more diligently in their professional sphere9. However, in terms of "anti-stigma" education or mental health education in general, a multicentre study evaluating stigma towards people with mental health problems in health science students found that there is a priority for this type of education in nursing and medical students10. Patients with mental health problems are labelled by health students as deviant, challenging, incompetent, or unable to parent appropriately.
Another Mexican study using the OMI-M scale in psychology students obtained perceptions of aggressiveness and higher scores in areas of social restriction and greater pessimistic prediction of recovery towards people with mental health problems11.
A literature review on stigma towards people diagnosed with borderline personality disorder indicates that both mental health nurses and social workers, psychiatrists or psychologists are a source of harmful attitudes towards people with this type of disorder12.
The majority of healthcare professionals who participated in a Spanish study conducted in 2017 believed that people with schizophrenia may pose a danger to the rest of the population or to themselves, while acknowledging that these patients do not receive the care they need. The conclusion of the research was that more "anti-stigma" training was needed13.
Another factor to consider in relation to stigma towards people with mental health problems is social contact. Previous studies evaluating the effect of combining education with direct or indirect contact found that this is the most effective strategy to improve attitudes and reduce the desire for social distance compared to education alone14.
Having a family member or friend with a mental health history would also positively influence the healthcare professional's relationship with the patient15,16.
Currently, there are studies evaluating the degree of stigma in health personnel or in nursing, medicine and psychology students17,18. However, there is little literature focusing on the attitude of healthcare residents on this issue.
According to a report prepared by the Ministry of Health in 2020, 38.9% of the population in Asturias has a mental health problem19. Based on this, residents in specialised health training (FSE) of the Principality of Asturias are very likely to have to care for patients with mental health problems throughout their careers.
It is therefore important to evaluate the beliefs, attitudes and behaviours of future specialists towards these patients and to see if they evolve during the residency period. This could help guide specialised health training (FSE) and implement plans and strategies in the field of care in order to provide better care by reducing the stigma of healthcare professionals.
AIM
The aim of the study was to evaluate the degree of stigma of residents in clinical specialities, the "anti-stigma" training received during residency and its influence on the beliefs and attitudes they had in the first and last year of the speciality.
MATERIALS AND METHODS
Study design and population
A descriptive cross-sectional study was conducted in which the target population was the first and last year residents of nursing, medicine and clinical psychology of the Principality of Asturias during the residency year 2021/2022. The inclusion of these categories is justified by the literature on stigma in the healthcare setting. The laboratory specialities of Clinical Analysis, Pathological Anatomy, Biochemistry and Hospital Pharmacy were excluded because they had less direct contact with patients.
The study population consisted of 431 residents, 20 were excluded because they did not meet the inclusion criteria described above, leaving 411: 232 (56.4%) in the first year and 179 (43.6%) in the last year of the speciality.
Sample size was calculated considering that the study would analyse mean overall stigma and assuming a standard deviation of 15 points and a desired precision of 2 for a confidence of 95%, resulting in a sample size of 250 residents.
Separate first- and last-year speciality listings were obtained and by stratified random sampling proportional to each stratum, 141 first- and 109 last-year speciality residents were selected.
Instrument
The Community Attitudes Towards Mental Illness (CAMI-S) scale, validated to Spanish by Dr Meritxell Sastre Rus17, was used to collect data. This scale consists of 20 items rated on a Likert scale of 1 to 5 points from "strongly disagree" to "strongly agree". Potential total scores range from 20 to 100 points with higher scores indicating more favourable reactions to integration.
Each item forming the scale can be classified around 3 factors ("integration and contact", "social distance" and "dangerousness and avoidance") based on the opinion on how to treat and care for a person with severe mental illness17. For this grouping, the recommendations of the author were followed17.
The score for each factor is obtained by adding the result for each item and reversing the scores of negative questions. So for questions with negative wording, the answers "disagree" and "strongly disagree" were scored 4 and 5, and the answers "agree" and "strongly agree" were scored 1 and 2.
The score ranges indicating “no stigma” for each of the three factors are: "integration and contact" 36-45, "social distance" 28-35, and "dangerousness and avoidance" 16 20. The overall score is 80-100.
In addition to the scale, a self-developed questionnaire was administered that collected information on year of birth (subtracting from 2021, the variable "age in years" was created) and on nominal qualitative variables: sex; speciality; care for patients with mental disorder; personal, family and friend history of mental disorder; training received on social beliefs towards people with mental disorder and through which resource; and its influence on beliefs and labels placed on people with mental disorder. Information was also collected from ordinal qualitative variables such as the year of residence completed at the time of taking the survey.
Procedure
Pilot test
A pilot test was conducted with 17 second- and third-year residents of Family and Community Medicine to study the suitability of the questionnaire for sociodemographic variables to the desired objective, evaluating clarity of the questions, their appropriateness, extent and comprehension.
After the test, a total of 5 responses were obtained. As a result, some sociodemographic data and their order of presentation were modified. In addition, the definition of mental disorder was included in the description of the CAMI-S. The remaining variables were classified into three sections: sociodemographic variables, personal training variables, and personal and family clinical variables.
Recruitment
A personalised email was sent to residents inviting them to take part in the study with a short cover letter from the authors explaining the purpose of the work and with the access link to the questionnaire built in the FORMS application. The questionnaire was sent at two distinct times, the first was sent on a Tuesday and a reminder was sent two weeks later on a Friday20.
Data analysis
The SPSS (Statistical Package for the Social Sciences) statistical package version 14.0 was used to analyse the results obtained. The absolute and relative frequencies of qualitative variables and the mean and standard deviation (SD) of quantitative variables were analysed. As training on social beliefs towards people with mental disorders is a primary endpoint of the study, in addition to the percentage, its 95% confidence interval was also obtained.
Mean score, overall standard deviation and 95% confidence interval were obtained for the overall CAMI-S score and each of its 3 factors. Since the sample followed a normal distribution, for the comparison of the questionnaire with the sociodemographic variables, the Student's t test was used, considering significant differences with a p value ≤ 0.05 and when zero is not included in the 95% confidence interval of the difference in means.
Scores for each factor also showed the percentage of residents without stigma.
Ethical considerations
The study protocol was approved by the Clinical Research Ethics Committee of the Principality of Asturias (registration code: 2021.440) Participants were informed that by completing the survey they consented to participate in the study. Data processing was performed anonymously in accordance with applicable data protection regulations.
To ensure the confidentiality of participants and in compliance with the Data Protection Act, residents were contacted by email from the Transformation and Knowledge Management Service belonging to the Directorate General for Quality, Transformation and Knowledge Management of the Regional Health Department of the Principality of Asturias (Spain).
RESULTS
A total of 144 residents completed the final questionnaire. This represents an overall response rate of 57.6%.
One hundred percent (7/7) of residents with degrees in Clinical Psychology, 67.2% (43/65) in Nursing and 53.1% (94/178) in Medicine responded.
Demographic and speciality variables
The predominant profile was that of a woman (72.2%) with an average age of 28.2 years (SD 3.8) who was in her first year of residence (54.2%). Overall, 51.4% had a medical speciality and 29.9% a nursing speciality. Table 1 shows the absolute and relative frequencies of the sociodemographic data collected.
When asked about their mental health history, 9.0% of residents (n = 13) had or had had a mental disorder. There were 2.8% (n = 4) of residents who did not want to answer. Over half, 54.9% (n = 79), had relatives and/or friends who had or had had a mental disorder. In this item, 8.4% (n=12) did not want to answer.
CAMI-S score and its factors
Table 2 shows the overall mean stigma score and score for the three study factors, with the standard deviation (SD) and 95% confidence interval (95% CI). The results found are associated with favourable “anti-stigma” positions.
The percentage of residents with scores in the ranges indicating "no stigma" was 77.8% (n = 112) in the factor "integration and contact", 80.6% in "social distance" (n = 116) and 81.9% in "dangerousness and avoidance" (n = 118).
Relationship between stigma and speciality year
In the comparative analysis between the year of speciality and the mean score obtained on the scale and its factors, the differences found were not statistically significant (Table 3).
Experience and training on social beliefs towards people with mental disorders during specialization
Table 4 shows the relative and absolute frequencies about residents' experience and training on social beliefs towards people with mental disorders.
Table 4. “Anti-stigma” training during specialisation (n = 144).
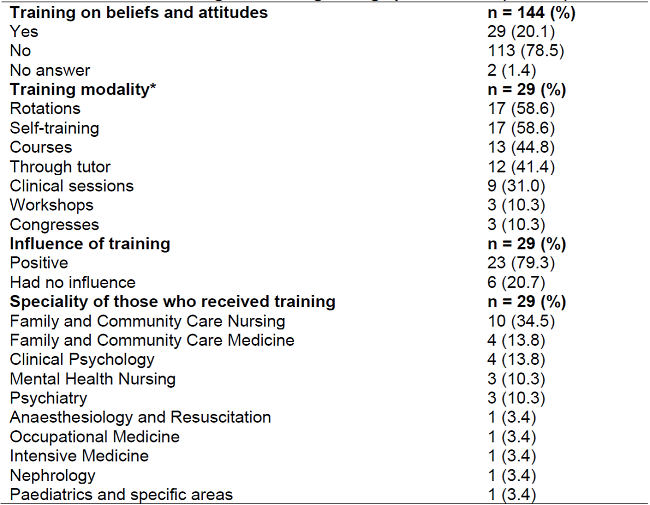
Note:Training modality*. They could answer more than one option.
According to the type of speciality in training, 55.6% (10 out of 18) of residents of the Mental Health speciality received some training and 25.9% (14 out of 54) of residents of Family and Community Care.
Of the 144 residents, 97 (67.4%) believed that general training in psychopathology and/or specific training in stigma would be necessary to improve beliefs and attitudes towards people with mental disorders. Only 1 resident (0.7%) said they did not believe any training was necessary.
At the time of the survey, 137 (95.1%) participating residents replied that during their training and/or working life they had treated someone with mental health problems. This contact positively influenced the beliefs and attitudes of 81 participants (59.1%) and negatively affected 6 participants (4.4%).
Relationship between stigma and training received
When the influence of training on the degree of stigma was assessed, statistically significant differences were obtained in the factors "social distance" and "dangerousness and avoidance" and in the overall CAMI-S score (Table 5).
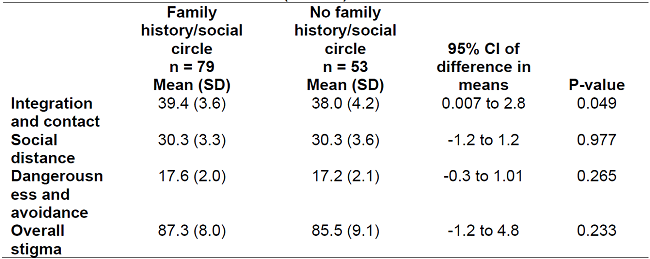
Relationship between stigma and personal, family or social history of mental disorder
Having had or having a mental disorder did not show any relationship with the total score on the scale or any of its factors (Table 6). This was not the case when there was a family history or social circle of mental disorder, finding statistically significant differences in the factor “integration and contact” (Table 7).
Table 6. CAMI-S score based on personal history (PH) of mental disorder (n = 140).

Note.p < 0.05 was considered statistically significant
Note 2:Participants who did not wish to answer were excluded from the analysis
DISCUSSION
In response to the objective of this study, the overall mean stigma score in first and last year residents in specialised health training was 86.7 (95% CI: 85.3-88.1). This result is in the upper half of the range of possible CAMI-S scores from 20 to 100, with the highest scores being more favourable reactions to integration.
The average score observed in the subscales “integration and contact”, “social distance” and “dangerousness and avoidance” is included in the score range considered “without stigma”, with the majority of residents located in those ranges. Comparisons with other studies using the CAMI-S scale cannot be made as none were found.
No influence of the speciality year on the degree of stigma was observed. Although training is considered an effective measure to reduce stigma13,15, only 20.1% of residents had been trained in beliefs towards people with mental disorders during their time in specialisation.
The study confirmed the benefit of this training, since those who received it had lower stigma scores, both overall and in each of the three factors of the CAMI-S scale. However, no statistically significant results were found in the factor "integration and contact", perhaps due to chance, since, observing the confidence interval of the difference of the means, it can be assumed that a larger sample of trained residents would give a different result.
Similar results have been found in other studies, concluding that social distance as an indicator of stigma is lower among professionals who had received "anti-stigma" training14,15,21. Such training would promote the integration of the mentally ill patient into the community environment and reduce avoidance attitudes and the view of the patient as a dangerous person.
The research carried out showed a better result of stigma when there is a history of relatives or friends with mental disorder, but only on the factor "Integration and contact" and no possible reasons are found to explain it. Prior contact, whether from family or friends with mental illness, positively influences beliefs and attitudes towards these patients16.
Having a personal history of mental disorder made no difference in stigma. In this respect, the literature consulted does not take a clear position. Some authors claim that there are more favourable and positive attitudes when it is the health personnel themselves who have a personal mental health history16: they see stigma as unfair and take it as a personal goal of change. However, others point out that some seem to apply prejudice to themselves which negatively affects their self-esteem and self-efficacy by limiting the possibility of counteracting inaccurate stereotypes22,23.
Healthcare professionals have a duty to perform their functions guided by bioethics and prioritising patient well-being and holistic care, and evidence argues that a lack of mental health training causes an imbalance in this care. Currently in Asturias, more than half of healthcare residents in training care for mental health patients following social constructs more than medicine, nursing and evidence-based psychology24.
There is now an urgent need to include unified and regulated "anti-stigma" training in cross-disciplinary and non-cross-disciplinary training schemes. It's not too late yet, 6 out of 10 residents who are still in their first year of speciality have no training, but can still get it. Not only has this training been found to be effective, but it has shed light on those interventions that have been most effective in reducing the stigma of students and healthcare professionals towards patients with mental illness16,25.
The lack of a specific training plan that includes content on mental health, and more specifically, on "anti-stigma", in the face of the established need for it, corroborates the low importance and low interest for investment of resources in this health sector26, despite the growing interest it is generating in both public and political media27,28.
Limitations
Although the CAMI-S scale is a reliable tool for assessing stigma in the Spanish population, and can therefore be used for residents of nursing, medicine and clinical psychology, it does not take into account the characteristics of each of the professions.
Overall, it appears that the majority of residents in the study population have "anti-stigma" attitudes towards people with mental disorders. However, the fact that 42.4% of selected residents have decided not to participate in the study implies a selection bias that may compromise the validity of the results obtained. If non-participation was motivated by stigma attitudes, the results observed in the study would be overestimated.
As respondents were aware the purpose of the study and as it is a controversial subject, the social desirability bias and the Hawthorne attention or effect bias are also likely to have occurred, albeit to a lesser extent because it is an anonymous questionnaire.
CONCLUSIONS
First- and last-year residents of specialised health training in Asturias have high "anti-stigma" scores for patients diagnosed with mental illness. Although there is no significant change in their beliefs and attitudes towards these patients from the start to the end of their speciality, there is evidence of the benefit of training on a lesser degree of stigma. In addition, the history of family or friends with mental health problems improves residents' view of this group.
It is necessary that the training plan of residents of specialised health training include regulated and unified content in mental health and more specifically in the area of "anti-stigma". This would impact on healthcare providers' view of mental health patients, thereby improving the care provided.
Acknowledgements
We would like to thank the participants for agreeing to participate in this work and Dr Meritxell Sastre-Rus for providing us with the necessary keys to use the CAMI-S scale
REFERENCES
1. Stucchi-Portocarrero S. Estigma, discriminación y concepto de enfermedad mental. Revista de Neuro-Psiquiatria. 2013;76(4):218-223. [ Links ]
2. Espino-Granado A, editor. La atención a la Salud Mental en España. Estrategias y compromiso social. En Toledo: Ministerio de Sanidad y Consumo; 2005. Disponible en: https://www.sanidad.gob.es/va///organizacion/sns/planCalidadSNS/pdf/excelencia/salud_mental/opsc_est15.pdf.pdf [ Links ]
3. ASALE R, RAE. estigma | Diccionario de la lengua española. En: "Diccionario de la lengua española" - Edición del Tricentenario [Internet]. 2022. [citado 28 de marzo de 2022]. Disponible en: https://dle.rae.es/estigma [ Links ]
4. CORRIGAN PW, WATSON AC. Understanding the impact of stigma on people with mental illness. World Psychiatry. febrero de 2002;1(1):16-20. [ Links ]
5. Tosas A. Desenvolupament d'un Itinerari d'acceleració i un Pla Antiestigma a la Taula de Salut Mental de Terrassa [Internet]. 2018 nov [citado 4 de septiembre de 2022]; Barcelona. Disponible en: http://salutmentalterrassa.org/wp-content/uploads/2019/11/181116-Presentacio-Terrassa-comprimido-ok.pdf [ Links ]
6. Global Anti-Stigma Alliance [Internet]. [citado 4 de septiembre de 2022]. Disponible en: http://antistigma.global/ [ Links ]
7. López M, Laviana M, Fernández L, López A, Rodríguez AM, Aparicio A. La lucha contra el estigma y la discriminación en salud mental: Una estrategia compleja basada en la información disponible. Revista de la Asociación Española de Neuropsiquiatría. 2008;28(1):48-83. [ Links ]
8. Navarro N, Trigueros R. Estigma en los profesionales de la Salud Mental: una revisión sistemática. Psychology, Society, & Education. 19 de julio de 2019;11:253. [ Links ]
9. Ministerio de Sanidad, Política Social e Igualdad. Orden SPI/1356/2011, de 11 de mayo, por la que se aprueba y publica el programa formativo de la especialidad de Enfermería de Salud Mental [Internet]. Sec. 3, Orden SPI/1356/2011 may 24, 2011 p. 51802-22. Disponible en: https://www.boe.es/eli/es/o/2011/05/11/spi1356 [ Links ]
10. Masedo A, Grandón P, Saldivia S, Vielma-Aguilera A, Castro-Alzate ES, Bustos C, et al. A multicentric study on stigma towards people with mental illness in health sciences students. BMC Med Educ. 7 de junio de 2021;21:324. [ Links ]
11. Mascayano F, Tapia T, Schilling S, Alvarado R, Tapia E, Lips W, et al. Stigma toward mental illness in Latin America and the Caribbean: a systematic review. Braz J Psychiatry. marzo de 2016;38(1):73-85. [ Links ]
12. Sheehan L, Nieweglowski K, Corrigan P. The Stigma of Personality Disorders. Curr Psychiatry Rep. enero de 2016;18(1):11. [ Links ]
13. Díaz-Iglesias L, Pacheco-Álvarez B, Castro-Hevia S. Actitudes de los profesionales sanitario de Atención Primaria y Salud Mental hacia personas con problemas mentales. Principado de Asturias; 2017. [ Links ]
14. Lanfredi M, Macis A, Ferrari C, Rillosi L, Ughi EC, Fanetti A, et al. Effects of education and social contact on mental health-related stigma among high-school students. Psychiatry Res. noviembre de 2019;281:112581. [ Links ]
15. Sapag JC, Velasco PR. [Stigma toward mental disorders and addictions: Study in Chilean primary care]. Aten Primaria. mayo de 2020;52:361-3. [ Links ]
16. Henderson C, Noblett J, Parke H, Clement S, Caffrey A, Gale-Grant O, et al. Mental health-related stigma in health care and mental health-care settings. Lancet Psychiatry. noviembre de 2014;1(6):467-82. [ Links ]
17. Rus MS, Hidalgo JM, Canut MTL, Lorenzo AG, Sábado JT. Adaptación y validación preliminar de la forma española de la escala CAMI-S (Community Attitudes towards Mental Illness). Revista de enfermería y salud mental. 2018;(10):5-13. [ Links ]
18. Ochoa S, Martínez-Zambrano F, Vila-Badia R, Arenas O, Casas-Anguera E, García-Morales E, et al. Validación al castellano de la escala de estigma social: Community Attitudes towards Mental Illness en población adolescente. Rev Psiquiatr Salud Ment. 1 de julio de 2016;9(3):150-7. [ Links ]
19. Miguel-García F, Calvo-Reyes MC, Rodríguez-Cobo I. Salud mental en datos: prevalencia de los problemas de salud y consumo de psicofármacos y fármacos relacionados a partir de registros clínicos de atención primaria. BDCAP Series 2 [Internet]. Madrid: Ministerio de Sanidad; 2021. Disponible en: https://www.sanidad.gob.es/estadEstudios/estadisticas/estadisticas/estMinisterio/SIAP/Salud_mental_datos.pdf [ Links ]
20. Pit SW, Vo T, Pyakurel S. The effectiveness of recruitment strategies on general practitioner's survey response rates - a systematic review. BMC Medical Research Methodology. 6 de junio de 2014;14(1):76. [ Links ]
21. Nyblade L, Stockton MA, Giger K, Bond V, Ekstrand ML, Lean RM, et al. Stigma in health facilities: why it matters and how we can change it. BMC Med. diciembre de 2019;17(1):25. [ Links ]
22. Boyd JE, Katz EP, Link BG, Phelan JC. The relationship of multiple aspects of stigma and personal contact with someone hospitalized for mental illness, in a nationally representative sample. Soc Psychiat Epidemiol. 1 de noviembre de 2010;45(11):1063-70. [ Links ]
23. Corrigan PW, Rao D. On the Self-Stigma of Mental Illness: Stages, Disclosure, and Strategies for Change. Can J Psychiatry. agosto de 2012;57(8):464-9. [ Links ]
24. Sastre-Rus M. Construcción y validación de una escala para la evaluación del estigma de la enfermedad mental en Enfermería (EVEPEM) [Internet] [Tesis doctoral]. [Barcelona]: Universitat de Barcelona; 2019 [citado 22 de marzo de 2022]. Disponible en: http://diposit.ub.edu/dspace/bitstream/2445/141719/1/MSR_TESIS.pdf [ Links ]
25. Lien YY, Lin HS, Lien YJ, Tsai CH, Wu TT, Li H, et al. Challenging mental illness stigma in healthcare professionals and students: a systematic review and network meta-analysis. Psychol Health. junio de 2021;36(6):669-84. [ Links ]
26. Campo-Arias A, Oviedo HC, Herazo E. [Stigma: Barrier to Access to Mental Health Services]. Rev Colomb Psiquiatr. septiembre de 2014;43(3):162-7. [ Links ]
27. Errejón: "El plan de Salud Mental equivale a medio euro por persona al año". Redacción Médica [Internet]. [citado 26 de marzo de 2022]; Disponible en: https://www.redaccionmedica.com/secciones/sanidad-hoy/errejon-el-plan-de-salud-mental-equivale-a-medio-euro-por-persona-al-ano--8851 [ Links ]
28. Mancisidor M. Avilés asienta un servicio de psicoasesoría para jóvenes, paso previo a Salud Mental. La Nueva España [Internet]. 10 de marzo de 2022 [citado 26 de marzo de 2022]; Disponible en: https://www.lne.es/aviles/2022/03/10/aviles-asienta-servicio-psicoasesoria-jovenes-63641723.html [ Links ]
Received: May 28, 2022; Accepted: September 21, 2022











 text in
text in