My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Enfermería Global
On-line version ISSN 1695-6141
Enferm. glob. vol.22 n.69 Murcia Jan. 2023 Epub Mar 20, 2023
https://dx.doi.org/10.6018/eglobal.533011
Originals
Psychological effects of social distancing on medical students
1Medical degree student from the UNINOVAFAPI University Center. Teresina-PI, Brazil
2Graduated in Medicine from the Federal University of Ceará (UFC). Brazil
3Graduated in Medicine from the Health Sciences Center of UFRN. Specialist in Clinical Oncology for SBOC/AMB. Brazil
4Nurse. PhD candidate for EEAN - Anna Nery School of Nursing. Rio de Janeiro-RJ. Brazil. ellen_hill@hotmail.com
5Nurse. Post-doctorate at the Federal University of Santa Catarina. Associate Professor of the Department of Fundamental Nursing at EEAN/UFRJ. Rio de Janeiro-RJ. Brazil
Method:
A cross-sectional, descriptive and observational study with a quantitative approach, carried out in a University Center by applying an online electronic form to 170 university students, using the Patient Health Questionnaire-9, an instrument that assesses depressive disorder, and the General Anxiety Disorder-7 scale, which assesses and monitors anxiety.
Results:
It was verified that 42.9% of the students had moderate anxiety and 37.0% of the participants had moderate depressive disorder. Medical students aged between 25 and 29 years old with no previous psychological disorder were the most susceptible to presenting greater signs of depression and anxiety during the pandemic, and the students reported that they would have liked to have received psychological support from the university during this period.
Conclusions:
Educational institutions need to provide multilateral support, including early mental health interventions, especially during pandemic times.
Keywords: Mental Health; Scales; Anxiety; Depression; Students
INTRODUCTION
COVID-19 was first described on December 31st, 2019, in Wuhan, China, and after the decree recognizing the pathology as a pandemic, several measures to contain the infection and reduce care appointments in health systems have been implemented by local health authorities. These measures differed in terms of administrative spheres (federal, municipal, and state governments), but the most common approach was the social distancing practice1.
This measure to contain infection generated inherent behavioral changes, just as it happened in other pandemics, such as the 1918-1919 flu pandemic, which had high mortality rates and affected one out of three individuals at the global level. If at that time the priority was not to know the psychological effects of social distancing in a pandemic, in 2022, this has changed, becoming important to evaluate this impact on people's mental health2.
Studies conducted in the country of origin of the disease, China, have shown that social isolation has led to the onset of anxiety disorders, depression, somatization disorder and stress, identified in the general population, and specifically in health students3,4.
University students are a group susceptible to the onset of mental disorders. Nearly 15% to 25% of university students develop some type of psychiatric disorder during their training, with depression and anxiety as the most prevalent, which are most frequent during medical training. Suicide attempts are the second leading cause of death among medical students, which is directly related to the effects of major depression5)(6)(7.
The medical course is recognized as an environment of constant stressful conditions, resulting from the significant demands coming from the academic environment, the family, the labor market and the achievement of personal goals, which cause a series of concerns about expected performance; consequently, part of these students have low self-esteem, feelings of inadequacy and decreased self-confidence. Despite the high incidence of psychological distress in this population, few people seek psychological or psychiatric help5,6.
Accordingly, the rapid spread of COVID-19 and the social isolation measure have led to changes in education, such as suspension of face-to-face classes and internships, introduction of new teaching methodologies, and incorporation of digital technologies. This scenario marked by tension and uncertainties associated with the stressful variables of medical training were related to a higher frequency of mental disorders, especially anxiety and depression3)(4)(5.
In addition to that, in this pandemic period, medical students were exposed to frequent contact with death and suffering, deconstruction of medical omnipotence, awareness of the problems inherent to the profession, fear of becoming ill, fear of transmitting the disease to family members, and insecurity about completing the academic year, among others8.
Given the above, and taking into consideration the social distancing measure and the COVID-19 pandemic situation, it is important to know the students' psychological status, as they are a vulnerable population to mental disorders. This study aims at estimating the prevalence of anxiety and depression symptoms in medical students at a University Center in the municipality of Teresina, PI, describing the students' profile during the COVID-19 pandemic period.
MATERIAL AND METHOD
A cross-sectional, descriptive and observational study with a quantitative approach was carried out at a University Center located in the municipality of Teresina, PI. The data were collected from October 1st, 2020, to January 1st, 2021, among the medical students, as they are in the age group most susceptible to developing psychological disorders and have a tendency for depressed mood due to their routine studies and internships9.
In Brazil, nearly 20,000 physicians graduate each year. Therefore, it is estimated that, multiplied by the number of years of Medicine undergraduate studies, there are approximately 120,000 medical students in the country. Considering the worst-case scenario that maximizes the number of medical students in Brazil who had anxiety and depression symptoms during the pandemic, it would be 50%. Therefore, assuming 120,000 medical students with a 5% margin of error and 95% confidence, at least 170 participants are required10.
Data collection was carried out with all classes from the 1st to the 12th period of the medical course at the aforementioned university. The inclusion criteria were as follows: a) age 18 or older; b) regularly enrolled in the institution; c) participation in the synchronous meeting via the virtual learning environment held with each class to clarify the research. The sample consisted of 170 students and 37 questionnaires were excluded for being incomplete.
Considering the new reality brought about by the pandemic, collection was done through online electronic technology. Synchronous meetings were scheduled via a virtual learning environment; on these occasions, the research was presented and the students were later sent a link via email or WhatsApp, on which they clicked and were directly forwarded to the form, where the Free and Informed Consent Form was available on the first page and only after confirmation of consent did the participants have access to the questionnaire and the research scales.
The data collection instrument was a form divided into two parts: a sociodemographic questionnaire and another with scales that assessed depression and anxiety disorders: Patient Health Questionnaire-9 (PHQ-9) and the General Anxiety Disorder-7 (GAD-7), respectively. Both are consistent with the criteria set forth in the Diagnostic and Statistical Manual of Mental Disorders-Fourth Edition (DSM-IV)11.
The first part of the questionnaire consisted of six questions, three of which were about sociodemographic data and three about having a previous diagnosis of psychiatric illness, whether they maintained isolation and avoided social interaction, and whether they would have liked to have received psychological care from the university.
The second part of the form consisted of 16 questions, through the evaluation scales. PHQ-9 comprises nine items with scores ranging from 0 to 27, and verifies the frequency of depressive symptoms in the past two weeks; in turn, GAD-7 comprises seven items with scores ranging from 0 to 21, and assesses anxiety symptoms in the past two weeks. In order to interpret the data from the scales, the parameters contained in the literature were used11.
The frequency distributions of the sociodemographic data and data related to the answers given to the GAD-7 and PHQ-9 instruments were expressed by means of relative frequency (%) Tables. After collection, the data were transferred to Microsoft Excel 2016 and statistically analyzed in the Statistical Package for the Social Sciences (SPSS)® program, version 22.0. There was no identification of the participants in this study, guaranteeing anonymity and confidentiality of the data collected.
In compliance with Resolution No. 466/12 of the National Health Council belonging to the Ministry of Health, this research was approved by the Research Ethics Committee (Comitê de Ética em Pesquisa, CEP).
RESULTS
The sample consisted of 170 students, with predominance of the female gender (71.8%). Among the data collected, 74 (42.3%) declared themselves as brown-skinned and 60 (35.3%) as white-skinned. In relation to the age range, 62 (36.5%) are from 25 to 29 years old, although there was no significant difference with those aged from 22 to 25 (34.2%).
When asked if they had a diagnosis of any psychiatric illness, 28 (16.5%) reported having a clinical diagnosis. In relation to the pandemic, 116 (68.2%) remained isolated and avoided social interaction, and 110 (64.7%) reported that they would have liked to have received psychological care from the university during the social isolation period caused by the COVID-19 pandemic.
Regarding GAD-7, which assesses the students' anxiety level, it was found that 73 (42.94%) had moderate anxiety symptoms and only 7 (10.0%) of the participants had no degree of anxiety (Figure 1).
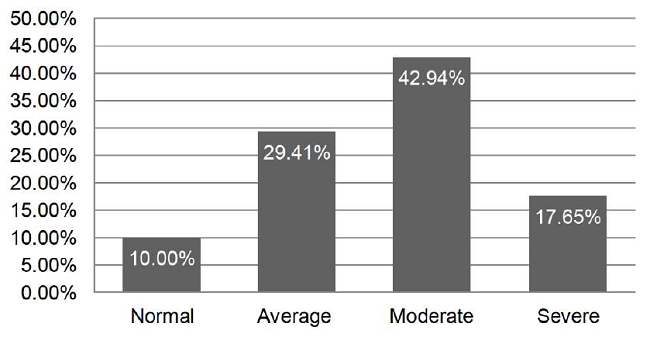
Figure 1: Degree of anxiety in the participants according to the GAD-7 questionnaire. Teresina, PI, Brazil, 2021.
Regarding the data related to PHQ-9, which assesses the presence and degree of depressive disorder, it was observed that 63 (37.0%) of the participants had moderate depressive disorder, and that a small proportion (16 [(9.4%]) had no symptoms of this disorder (Figure 2).

Figure 2: Degree of depressive disorder in the participants according to the GAD-7 questionnaire. Teresina, PI, Brazil, 2021.
Female medical students aged from 25 to 29, who declared to be brown-skinned, with no previous psychological disorder and who were in social isolation as recommended by the health authorities, were the most susceptible and presented the greatest signs of depression and anxiety during the pandemic.
DISCUSSION
The results confirm the repercussions of the social isolation imposed by the pandemic on medical students' mental health, with indications of how gender, age, previous psychological illness and social isolation influence the onset of mental disorders such as anxiety and depression. These results are consistent with other international studies which evidenced that medical students aged from 24 to 28 years old have more anxiety and depression symptoms when compared to other age groups12,13.
One hypothesis is that it is in this age group that the transition from late adolescence to adulthood takes place, which is characterized by important psychosocial changes, as well as that, since they are medical students, they are more exposed to an academic environment consisting of a large volume of content to study, emotional stress and financial impositions, favoring psychological distress14.
The pandemic, social isolation and closure of universities may also have affected these students' psychological conditions, due to the break in their connections and the interruption of their study routine, socialization and leisure, in a period of their lives when emotional frailty increases; therefore becoming more vulnerable to depression and anxiety symptoms15.
Some studies point to a poor adaptation to Education at a Distance (EAD) on the part of medical students, showing that this teaching method has led to difficulties studying, reduced concentration and problems adapting to the virtual platforms after the implementation of the social isolation measures; in addition to other stress sources regarding loss, delay in the semester, and accumulation of issues with resumption of face-to-face classes16.
In relation to gender, the results indicate that female medical students were at a higher risk for anxiety and depression disorders. In contrast, another study showed that men are more prone to depressive symptoms. The tendency to develop these disorders may vary according to gender and age group, but it can also be related to the questionnaires used to evaluate the depression and anxiety symptoms that were applied during the surveys, as well as the places where they were carried out17.
Another conjecture is that the association between depression, anxiety and the female gender can be due to the social demands of the multiple roles to be played by women, to the psychological shock resulting from the fear of infection by children or family members, and to the need to reassert their ability in medical environments commanded by the male gender, as well as the hormonal changes that emerged due the lack of face-to-face contact. In addition to that, women have a better perception of their feelings; therefore, they express their symptoms more clearly18.
Beyond the biological ills of the disease, the COVID-19 pandemic has exerted an impact on medical students' everyday life, negatively affecting mental health, especially among those in their final semesters, due to the fear of returning to internships and of infecting themselves and others with a potentially fatal virus. Thus, the longer the pandemic lasts, the more the demands on the emotional exhaustion of these students18,19.
In this study, most of the university students remained isolated and avoided social interaction during this period. The above corroborates with a cross-sectional survey conducted in India with 83 medical students, where most of the students adopted a social distancing stance, avoiding attending large gatherings, stopping going out of the house or completely isolating themselves20.
Although few students reported prior diagnosis of any psychiatric illness, other research studies confirmed that students more often develop mental disorders during medical training. It is therefore important to understand the main factors that caused this psychological wear out, mainly during the pandemic period, especially to prevent those situations that can contribute to deterioration of pre-existing conditions or diseases21,22.
The results also showed that the students would have liked to have received psychological care. Offering online emotional support in universities during the pandemic can provide a space for sharing and communication about issues of personal and academic life, enabling the creation of strategies for coping with difficulties in the new reality experienced23.
In this way, better welcoming and a reduction of conflictive situations can help minimize these frequent conditions in medical schools, as they impact not only on the students' own quality of life, but also on the way in which they will deal with their patients in the future24.
As a limitation of this study, we should mention the use of a virtual environment for conducting the research, which may have excluded some students who did not have access to this type of technology. Another important point is that the data from this study were collected during the period when the restrictive measures for commercial activities and services were in effect in the state of Piauí; in other words, the most critical moment of the pandemic in the state, when the restrictive measures and social isolation were intensified and everyone seemed to be exhausted and unmotivated.
CONCLUSION
The research on anxiety and depression conducted in this study indicated that a significant percentage of the students reported moderate to severe levels of anxiety and depression, with higher intensity among women. This exerts a negative impact on construction of the students' professional profile, as these pathologies also affect physical health and trigger the onset of other diseases.
Although personal communication has become difficult due to fear of COVID-19, it is important that universities recognize that the students' mental health and psychosocial well-being in this global health crisis scenario is relevant to educators and, thus, provide the multilateral support that students need, including early mental health interventions.
Given the above, it is possible to infer that it is fundamental, mainly in a pandemic that involves social distancing, to understand the psychological behavior of university students in the medical training process, valuing the emotional points that contribute to the physical and mental well-being of these future professionals. So that, in other pandemic events and with the support of research, educational institutions will be adequately prepared for intervention and prevention regarding depression and anxiety.
REFERENCIAS
1. Bezerra ACV, Silva CEM, Soares FRG, Silva JAM. Fatores associados ao comportamento da população durante o isolamento social na pandemia de COVID-19. Ciência & Saúde Coletiva [Internet]. 2020; 25(1):2411-2421. Disponível em: https://doi.org/10.1590/1413-81232020256.1.10792020 [ Links ]
2. Oliveira EHA. Coronavírus: prospecção científica e tecnológica dos fármacos em estudo para tratamento da Covid-19. Cadernos de Prospecção [Internet]. 2020; 13(2):412. Disponível em: https://doi.org/10.9771/cp.v13i2%20COVID-19.36153 [ Links ]
3. Zanon C, Zanon LLD, Wechsler SM, Favretti RR, Rocha KN. COVID-19: implicações e aplicações da Psicologia Positiva em tempos de pandemia. Estudos de Psicologia [Internet]. 2020; 37(1): e200072. Disponível em: https://doi.org/10.1590/1982-0275202037e200072 [ Links ]
4. Ozamiz-Etxebarria N, Dosil-Santamaria M, Gorrochategui P, Idoiaga-Mondragon N. Niveles de estrés, ansiedad y depresión en la primera fase del brote del COVID-19 en una muestra recogida en el norte de España. Cadernos de Saúde Pública [Internet]. 2020;36(4):e00054020. Disponível em: https://doi.org/10.1590/0102-311X00054020 [ Links ]
5. Costa DS, Cordeiro RA, Frutuoso ES. Sintomas de Depressão, Ansiedade e Estresse em Estudantes de Medicina e Estratégias Institucionais de Enfrentamento. Revista Brasileira de Educação Médica [Internet]. 2020;44(1): e040. Disponível em: https://doi.org/10.1590/1981-5271v44.1-20190069 [ Links ]
6. Huckins JF, Silva AW, Wang W, Hedlund E, Rogers C, Nepal SK, et al. Mental health and behavior of college students during the early phases of the COVID-19 pandemic: Longitudinal smartphone and ecological momentary assessment study. Journal of medical Internet research [Internet]. 2020;22(6):e20185. Disponível em: https://doi.org/10.2196/20185 [ Links ]
7. Oliveira MF, Araujo LMB. Mental health of the medicine student. Braz J Develop. 2019;5(11):23440-52.1. Disponível em: https://doi.org/10.1097/ACM.0000000000002958 [ Links ]
8. Freitas CAD, Arruda GFAD, Arruda GCFAD, Feitosa SF. Medical students in the COVID-19 pandemic response in Brazil: ethical reflections. Revista Brasileira de Educação Médica, 2021; 45(1): e036. Disponível em: https://doi.org/10.1590/1981-5271v45.1-20200231 [ Links ]
9. Ansari A, Sherafati A, Aghajani F, Khonii MS, Aghajani R, Shahmansouri. Depression and anxiety among Iranian Medical Students during COVID-19 pandemic. Iranian journal of psychiatry [Internet]. 2020; 15(3):228. Disponível em: https://doi.org/10.18502/ijps.v15i3.3815 [ Links ]
10. Conselho Federal de Medicina. Demografia Médica: Brasil possui médicos ativos com CRM em quantidade suficiente para atender demandas da população [Internet]. Portal Médico - Conselho Federal de Medicina. 2018. Disponível em: https://portal.cfm.org.br/index.php?option=com_content&view=article&id=27983:2018-11-26-13-05-15&catid=3. [ Links ]
11. Xiao H. et al. Social distancing among medical students during the 2019 Corona virus disease pandemic in China: Disease awareness, anxiety disorder, depression, andbehavioralactivities. Int. J. Environ. Res. Public Health. 2020; 17(14):5047. Disponível em: https://doi.org/10.3390/ijerph17145047. [ Links ]
12. Xie J, Li X, Luo H, He L, Bai Y, Zheng F, et al. Depressive symptoms, sleep quality and diet during the 2019 novel coronavirus epidemic in China: a survey of medical students. Frontiers in Public Health [Internet]. 2021;8(1):1096. Disponível em: https://doi.org/10.3389/fpubh.2020.588578 [ Links ]
13. Lai J, Ma S, Wang Y Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA network open [Internet]. 2020;3(3): e203976-e203976. Disponível em: https://doi.org/10.1001/jamanetworkopen.2020.3976 [ Links ]
14. 20. Maia BR, Dias PC. Ansiedade, depressão e estresse em estudantes universitários: o impacto da COVID-19. Estudos de Psicologia [Internet]. 2020;37. Disponível em: https://doi.org/10.1590/1982-0275202037e200067 [ Links ]
15. Dias DCG, Pantoja CL, Santos BF, Oliveira OS, Silva AMF, Melo CCD, et al. Saúde Mental na Medicina: Um estudo da prevalência de sintomas depressivos e ansiosos em acadêmicos de medicina. Brazilian Journal of Health Review [Internet]. 2021;4(4):15313-15329. Disponível em: https://doi.org/10.34119/bjhrv4n4-075 [ Links ]
16. Felippe TO, Spaniol CM, Silva LA, Calabria AC, Ferreira C, Carvalho NL, Moretti M, Bellinati NVC. O estresse do estudante de Medicina durante a pandemia de COVID-19. Research, Society and Development. 2021; 10(9):e58310918372, 2021. Disponível em: DOI: http://dx.doi.org/10.33448/rsd-v10i9.18372 [ Links ]
17. Vasconcelos TC, Dias BRT, Andrade LR, Melo AF, Barbosa L, Souza E. Prevalência de sintomas de ansiedade e depressão em estudantes de medicina. Revista Brasileira de Educação Médica [Internet].2015;39(1):135-142. Disponível em: https://doi.org/10.1590/1981-52712015v39n1e00042014 [ Links ]
18. Khan KS, Mamun MA, Griffiths MD, Ullah I. The mental health impact of the COVID-19 pandemic across different cohorts. International journal of mental health and addiction [Internet]; 2022;20(1):p. 380–386. Disponível em: https://doi.org/10.1007/s11469-020-00367-0 [ Links ]
19. Pandey U, Corbett G, Mohan S, Reagu S, Kumar S, Farrell T, Lindow S. Anxiety, depression and behavioural changes in junior doctors and medical students associated with the coronavirus pandemic: a cross-sectional survey. The Journal of Obstetrics and Gynecology of India [Internet]; 2021;71(1):33-37. Disponível em: https://doi.org/10.1007/s13224-020-01366-w [ Links ]
20. Salman M, Asif N, Mustafa ZU, Khan TM, Shehzadi K, Hussain K, Tahir H, Raza MH, Khan MT. Psychological impact of COVID-19 on Pakistani university students and how they are coping. Medrxiv [Internet]. 2020; 3(2). Disponível em: https://doi.org/10.1101/2020.05.21.20108647 [ Links ]
21. Teixeira LAC, Costa RA, Mattos RMPR, Pimentel D. Saúde mental dos estudantes de Medicina do Brasil durante a pandemia da coronavirus disease 2019. Jornal Brasileiro de Psiquiatria [Internet]. 2021, 70(1):21-29. Disponível em: https://doi.org/10.1590/0047-2085000000315 [ Links ]
22. Rodrigues BB, et al. Aprendendo com o Imprevisível: Saúde mental dos universitários e Educação Médica na pandemia de Covid-19. Revista Brasileira de Educação Médica [Internet]. 2020; 44(1): e149, 2020. Disponível em: https://doi.org/10.1590/1981-5271v44.supl.1-20200404. [ Links ]
23. NishimuraY, Silva TCRP, Pereira FPCMB, Neves BA, Almeida BC, Casagrande V, Ribeiz RI, Nunes PV. Impact of the COVID-19 pandemic on the psychological distress of medical students in Japan: cross-sectional survey study. Journal of medical Internet research [Internet]. 2021;23(20): e25232, Disponível em: https://doi.org/10.2196/25232 [ Links ]
24. Ribeiro CF, et al. Prevalence of and Factors Associated with Depression and Anxiety in Brazilian Medical Students. Rev. bras. educ. med. [online]. 2020; 44(1):e021. Disponível em: 10.1590/1981-5271v44.1-20190102.ing. [ Links ]
Received: July 15, 2022; Accepted: October 01, 2022











 text in
text in 


