Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Enfermería Global
versión On-line ISSN 1695-6141
Enferm. glob. vol.22 no.69 Murcia ene. 2023 Epub 20-Mar-2023
https://dx.doi.org/10.6018/eglobal.517721
Originals
Validation: instrument on latent tuberculosis infection in healthcare professionals
1Federal University of Piauí. Brazil. adrianamenesesbrandao@gmail.com
2Health and Tropical Medicine, Institute of Hygiene and Tropical Medicine, University Nova de Lisboa, Portugal
Objective:
To validate the content and appearance of an instrument on latent tuberculosis infection in healthcare professionals.
Methods:
Methodological study developed in three stages, from May to November 2020. Content Validation strategies were used through the Delphi technique and Appearance Validation. The evaluation of the instrument was carried out by nine judges, nurses and doctors, with master's and doctoral degrees. To test the agreement of the judges, the content validity index and the inter-rater agreement index were used. For the pre-test, the positivity index was used.
Results:
An instrument with 48 items was developed and, after evaluation by the experts, those with a content validity coefficient lower than 0.8 were modified. Some items were added and others deleted. At the end of two evaluation rounds, the instrument resulted in 49 items, with a content validity index = 0.9; Interrater Agreement = 1,000 and positivity index =100%. The semantic assessment of the instrument (pre-test), conducted with the target population, which consisted of Primary Care professionals (doctors, nurses, dentists, and nursing technicians), obtained a positivity rate of 100%, which indicated understanding of the instrument, with no need for further changes.
Conclusion:
The instrument has content and appearance validity to assess what is proposed, considering that the reliability and agreement indices of evaluation reached values above 80%.
Keywords: Validation Study; Latent Tuberculosis; Health Personnel
INTRODUCTION
Tuberculosis (TB) is described as an infectious and communicable disease, which can be caused by any of the seven species that make up the complex Mycobacterium tuberculosis: M. tuberculosis, M. Bovis, M. africanum, M. Canetti, M. microti, M. pinnipedi and M. Caprae. However, when considering the sanitary point of view, the most important species is M. tuberculosis, which, when infecting man, can affect mainly the lungs and affect other organs and systems. Its transmission occurs from inhalation of aerosols from the airways, expelled by cough, sneezing or speech of patients with pulmonary or laryngeal TB. Therefore, only people with these forms of active TB transmit the disease1.
Every year, 10 million people fall ill with TB, which, despite being a prevenTable and curable disease, causes 1.5 million deaths each year, and is the leading cause of death from infection in the world, being the main cause of death of people with the Human Immunodeficiency Virus (HIV). According to the World Health Organization (WHO), approximately a quarter of the world's population is infected with TB-causing bacteria, with only 5 to 15% of these manifesting the disease, active. In Brazil, the incidence is 46 per 100,000 people. The rest of these are infected, but they are not sick and cannot transmit the disease, that is, they have latent tuberculosis infection (LTBI)2)(3)(4.
Currently, the need to assess the prevalence of latent TB infection in health professionals has emerged, especially in those who work in Primary Health Care (PHC)4. They are responsible for TB control actions and at the time of care are exposed to various contagion situations, which involve from lack or poor quality of personal protective equipment, especially masks with low efficiency filters, and absence of aerosol control in environments5.
In addition to the contacts of cases of active pulmonary TB, two other populations deserve special attention during screening for the identification of LTBI: people living with HIV (PLHIV) and health professionals. For PLHIV, the special focus is due to the increased risk of developing active disease, due to the less effective immune response; while for health professionals it is due to constant exposure to people with TB, increasing the risk of developing active disease. In these professionals, one should always seek and consider the possibility of recent infection6.
In this context of greater vulnerability to infection and illness, the health team presents an increased risk of three to twenty times, when compared to the general population7,8. And this group also includes students in the health area, and students of nursing, physiotherapy and medicine have increased risk of TB infection in relation to the others7,8.
Screening for LTBI is an important preventive measure against tuberculosis infection. Despite the existing studies, whose object was the LTBI in health professionals, it is understood that the instruments used to collect data from participants lack greater accuracy to cover issues related to LTBI. Thus, it is important to build an instrument to identify the factors associated with latent TB infection in health professionals. Thus, the instrument must have internal validity, that is, the instrument really measures what it proposes to measure, ensuring that the data obtained effectively reflect valid and reliable information.
Based on the above, the present study aims to perform validation of content and appearance of an instrument on the evaluation of risk factors of LTBI in health professionals.
METHODS
Methodological study conducted from May to November 2021 and developed in three stages.
The first stage consisted of the adjustment of the 1st version of the instrument previously constructed, which occurred from the adaptation of questions of instruments on TB and LTBI already applied previously, but not validated and, predominantly, from information contained in the Clinical Protocols and Therapeutic Guidelines (PCDT) related to TB and website of the Department of Neglected Diseases/TB, of the Ministry of Health (MH).
The second stage was the validation of the instrument, in which the Delphi technique was used in order to reach the consensus. Thus, every return to the researcher, the answers were organized and analyzed and, if necessary, changes were made to the instrument, with forwarding to the experts, starting a new cycle until achieving the consensus 9.
The selection of specialists was carried out through evaluation of the curriculum registered in the Lattes/CNPq Platform, with the contact being carried out by e-mail. The criteria used were: to be a higher education health professional working in the care or management area related to TB control or teaching with research on the TB/LTBI theme. The exclusion criterion was incomplete collection instrument and failure to obtain a minimum score of five points in the profile of specialists, whose score is as follows: Doctorate (4) Master (3) Specialization in the area or related areas (2) Scientific production in the area or related (2) Time working in the area per full year (1)10.
There is no consensus in the literature regarding the number of judges to be invited, nor the number of judges to integrate the final sample. Authors recommend that the instrument be evaluated by a committee composed of five to ten judges for its validation in the health area11. This study had the participation of nine judges in this validation stage, although 13 judges were invited. The experts evaluated the instrument according to a form that addressed: I - Content of the questions, according to the relevance of the content, objectivity and simplicity; II - Appearance and comprehension of the instrument, which also had an open field carrying out extra comments, as well as suggestions for the inclusion or exclusion of questions, as suggested in the literature12,13.
In the third stage, the pre-test of the instrument was carried out, being the semantic evaluation with the target population, that is, with the professionals of the problems perceived by them concerning the understanding of each item and detection of difficult to understand terms. The inclusion criterion was to work in PHC, in a basic health unit with TB care for at least six months. The exclusion criterion was returning the evaluation script of the research instrument not completed. The contact was made in person, obeying all COVID-19 prevention measures, in previously selected Basic Health Units (BHU).
Thus, ten participants were selected by convenience, female, aged 22 to 26 years, five nursing technicians, three nurses, a doctor and a dentist surgeon. As the literature suggests, these professionals were subdivided into two strata, including professionals with lower education level (technical level) and professionals with higher education level (higher level) to verify if there were different levels of understanding of the instrument according to schooling. Subsequently, they completed an evaluation form of the data collection instrument considering clarity (objectivity and simplicity), relevance (relevance of the question) and appearance (adequacy of language and order of questions) 12,13.
Both in the form for specialists, and for health professionals counted the option of assigning values from 1 to 5 for each issue, where the value 1 means the worst grade and the value 5, the best, where the value equal to or greater than 4 means that the evaluated question met the objectives proposed in the study14.
At the end of each round of evaluation with the experts, the Content Validity Index (CVI) and the Global Content Validity Index (gCVI) were calculated by item and domain aiming measure the proportion of agreement on certain aspects of the instrument and its items, considering valid those that obtained a minimum percentage of 80% agreement among experts15. The Reliability Index or Inter-validator Agreement, through the IRA (Interrater Agreement), was also calculated by item and by domain in order to evaluate the extent to which judges are reliable in the evaluations of the items against the context studied16.
For analysis of the pre-tests, considering the domains of the scale, the Positivity Index was calculated, where those domains and items with a rate greater than or equal to 75% of positive responses were considered adequate and those with a rate below 75% of positive responses were considered inadequate and passive for improvement17.
Figure 1 presents the synthesis of all steps taken to validate the study.
This study is part of a macro project approved by the Research Ethics Committee (REC) under opinion n. 4.659.100 (CAAE: 41550620.4.0000.5214), respecting all ethical precepts contained in Resolution n. 446/12 of the National Health Council (CNS) such as using the Informed Consent Form (ICF) and explaining the risks and benefits to participants.
RESULTS
The study included nine specialists, 6 female and three male, aged 42 to 69 years, graduation from 1980 to 2011, with working time from 17 to 41 years, with three being from the medical area and six from the nursing area, with all having experience in teaching, working in the area, participating in events and publishing in the area, of these: three with master's level and six with doctorate.
The initial instrument submitted to the first evaluation of the judges contained six domains, these being dismembered as follows: 1. Identification data - five items; 2. Socioeconomic characterization - seven items; 3. Behaviors/vices - six items; 4. Knowledge about tuberculosis - 15 items; 5. Previous exposure to tuberculosis - 10 items; 6. Domain related to latent tuberculosis - five items, totaling 48 items. Thus, in Table 1, it is possible to observe the initial instrument with the CVI and IRA resulting from the first round of evaluation by the judges.
Table 1. First round of instrument evaluation according to relevance, appearance and understanding of domains and items. Teresina, PI, Brazil, 2021:
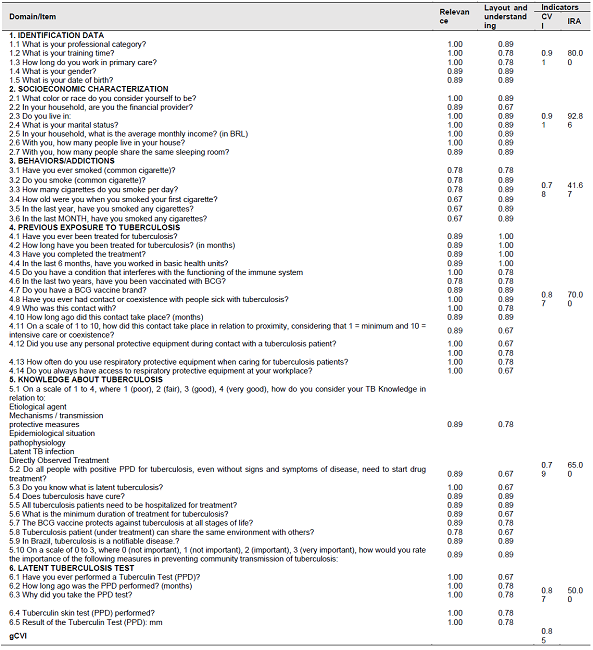
Source: Direct research.
In the first round, it was suggested in domain 1 (identification) the reallocation of items within the domain itself; there was also the suggestion of reallocation of two questions from domain 2 (racial declaration and marital status) to 1. In domain 2 (socioeconomic characterization) recommendations were to exclude item 2.2 related to the financial head of the household and the addition of room quantification of the interviewee's residence.
In domain 3 (behavior/addictions), the 6 items were maintained, but there was a change of position to improve understanding, in addition, it was suggested the inclusion of 4 items, these being: use of electronic cigarettes, alcohol, frequency of alcohol intake and drug use. In domain 4 (previous exposure to tuberculosis), it was recommended the replacement after the knowledge domain, as well as the addition of an item on the type of mask used by professionals and the exclusion of items on the occurrence of vaccination in the last two years (item 4.6) and the presence of vaccine brand (item 4.7).
In domain 5 (knowledge about tuberculosis), all questions were maintained, but there was the inclusion of alternatives with the definition of LTBI in item 5.3, as well as the exchange of the PPD nomenclature in item 5.2 by tuberculin proof. It is worth mentioning that one of the judges considered this domain insignificant, especially when applied to professionals of technical level, due to the complexity of the questions, but the researchers chose not to accept this suggestion, whereas there was no agreement of the others.
Regarding domain 6 (latent tuberculosis test) the opinions were summarized to the exclusion of item 6.4, regarding the tuberculin test, since all respondents, in theory, should go through this procedure. The other items were maintained as they were constructed. In Chart 1, it is possible to observe all changes, exclusions and suggested additions.
Table 1. Changes, exclusions and additions of items suggested by the judges performed in the instrument's items. Teresina/PI, Brazil, 2021:

Source: Direct research.
After the changes, a second round was held to consolidate these changes suggested by the judges in the first round, when only seven judges returned with the evaluation. gCVI reached 0.98 and IRA reached 1.00 in all domains according to Chart 2.
Table 2. Content Validity Index (CVI) and Inter-evaluator Agreement (IRA) in the second evaluation round of the Instrument on LTBI in Health Professionals, according to domains and items. Teresina, PI, Brazil, 2021:

Source: Direct research.
Chart 3 shows that the participants of this pre-test stage considered that all domains of the instrument presented clarity, objectivity, good appearance and easy understanding, thus obtaining the positivity index necessary for validation.
DISCUSSION
In order for an instrument to provide accurate, valid and interpreTable data, it must undergo testing, especially regarding its validity15. Considering that the final instrument reached a gCVI higher than the minimum of 80% as recommended in the literature, it is indicative that the adequacy to the original text was fundamental both for the validation of each item and for the general evaluation of the instrument, which was finished keeping the six dimensions, but 49 items.
In domain 1 (Identification), one of the judges called attention to the fact that the item that originally questioned financial leadership of the family is an outdated topic and that adds nothing to the study, since the family income should be analyzed, that is, of all people who contribute economically to the income of the family, regardless of leadership. Therefore, the exclusion of topic 2.2 from the final instrument was justified. In addition, low family income is associated with greater vulnerability to tuberculosis infection18.
The addition of the item that quantifies the number of rooms in the house (excluding bathrooms) is necessary to calculate the number of people living in the same residence by the number of rooms, because there is an association between the incidence of TB with overcrowded households because it is a respiratory infection19.
In domain 3 (Behavior), an item was added, which addresses the electronic cigarette justified by the adverse effects that smoking has on respiratory immune function, associated with an increased risk of respiratory tract infections, including TB. Electronic cigarettes expose the body to a variety of chemical elements including metal nanoparticles (generated by the device itself), and known carcinogens and cytotoxic substances such as nicotine. Moreover, the use of this new type of cigarette increases by more than three times the risk of experimentation with common cigarettes among those who have never smoked. Thus, the greatest impact of smoking in terms of public health problems related to infection is probably the increased risk of TB20,21.
Items referring to alcohol consumption were also added. The harmful use of alcohol is classified among the five main risk factors for the development of diseases, disabilities and death, since the use of alcohol significantly changes the immune response, increasing the susceptibility to respiratory diseases, which include TB22.
Closing the changes in domain 3, there is the suggestion of the judges to add a topic regarding the use of illicit drugs. Epidemiological data suggest that the relationship between TB and illicit drug use is increasing, being considered as a public health problem. Among illicit drug users, M. tuberculosis infection and progression to active disease are promoted by several factors, including the risky lifestyle of these users; overcrowded housing conditions; the accumulation and isolation of people indoors for illicit drug use; the sharing of materials such as pipes; malnutrition and severe cough by many users; the spread of HIV infection among illicit drug users; and the large number of inmates22.
In domain 4, only one judge disagreed with some questions about knowledge related to TB and LTBI and suggested exclusion, claiming that, among the target population, professionals with different levels of education and those with lower education may not be able to answer the questions. However, this suggestion was not accepted, considering that, regardless of the level of training of the professional, if they deal with TB daily, they must have a minimum understanding of its forms of transmission and prevention. This is an assumption of epidemiological surveillance: knowledge about diseases favors the application of preventive and curative measures23.
Health education is an important tool that involves theoretical and philosophical aspects, which should guide the practice of all health professionals, both higher and technical level professionals. Teams should be guided and trained to carry out health promotion and health surveillance actions, not only aimed at the patient, family and community, but also at work and the environment, since health professionals, including those in primary health care, have a high prevalence of LTBI24,25. Given this, it was decided to maintain the Knowledge about Tuberculosis domain for all professionals, regardless of the level of study.
In domain 5, the addition of the item on the type of mask used by the health professional during contact with patients with TB was of great contribution to the instrument, since the recommendation for use of the professional is the mask type PFF2/N95, which prevents inhalation of aerosols expelled by the patient, if used correctly. It is noteworthy that, until 2019, the year before the pandemic produced by the coronavirus (COVID-19), this practice was being neglected by health professionals, even when there was availability of adequate Personal Protective Equipment (PPE)5. Possibly, the COVID-19 pandemic leaves this legacy related to the use of masks. Health professionals, as well as the general population, have come to value this important mechanical protection more, after coping with this pandemic so prolonged and has demonstrated the effectiveness of masks in protecting against respiratory diseases26.
One of the items in domain 5 addresses the issue of BCG vaccination. The WHO, in 2018, released a note in which it no longer recommends the revaccination of children with BCG in case of non-development of the vaccine scar, as there are no indications of absence of protection. Following this line, the Ministry of Health, in 2019, launched the Information Note N. 10/2019, no longer recommending revaccination in these cases. Moreover, adult revaccination is indicated when living with leprosy patients27.
The project faced limitations related to the difficulty of participation of some expert professionals. However, it was possible to count on the participation of a larger quantity than initially expected, so as not to bring losses to the study. Furthermore, in view of being a multiphase process in which each judge had to participate more than once in the evaluations, the difficulties were even greater, but repeating the contact was a way to circumvent them.
CONCLUSION
Content validation was performed by a panel of nine experts from the areas of Pneumology and public health nursing, using the Delphi technique, obtaining a global content validity index (gCVI) of 0.85 and 0.98 in the first and second round, respectively. The original instrument contained 48 items distributed in six domains, and after validation, remained with the same quantitative domains, but with 49 items.
The semantic evaluation of the instrument or pre-test conducted with the target population consisted of PHC professionals, with professionals in the medical, dental, nursing areas and nursing technicians, obtaining a positivity index of 100%, which indicated understanding of the instrument, with no need for further changes. Concluding the theoretical pole adopted in this study.
This research is considered relevant, since it presents the first instrument validated on LTBI in health professionals in Brazil, which in addition to enabling a better understanding of the factors related to LTBI in these professional categories, field with research gaps, can be used in the screening of LTBI, on the occasion of admission and periodic examinations of professionals inserted in TB programs, with a view to detection, monitoring and early treatment of infection, and can be used in other research. In this perspective, this study is an achievement for the area of research in tuberculosis.
REFERENCIAS
1. Ministério da Saúde (BR); Secretaria de Vigilância em Saúde; Coordenação-Geral de Desenvolvimento da Epidemiologia em Serviços. Guia de Vigilância em Saúde. Brasília, DF: Ministério da Saúde; 2019. [ Links ]
2. World Health Organization. Tuberculosis. 2021. [citado 22 dez 2021]. Disponível em: https://www.who.int/health-topics/tuberculosis#tab=tab_1 [ Links ]
3. Ministério da Saúde (BR). Secretaria de Vigilância em Saúde. Departamento de Vigilância das DoençasTransmissíveis. Protocolo de vigilância da infecção latente pelo Mycobacterium tuberculosis no Brasil. Brasília, DF: Ministério da Saúde; 2018. [ Links ]
4. WHO. Relatório global sobre tuberculose 2018. Organização Mundial da Saúde; 2019. 231 pp. [ Links ]
5. Araújo MRS, Silva HP, Silva AKLS. Avaliação situacional de biossegurança em tuberculose em Unidades Básicas de Saúde na Amazônia. Rev Bras Saúde Ocup. 2016; 41:e21. https://doi.org/10.1590/2317-6369000125115 [ Links ]
6. Protocolo de vigilância da infecção latente pelo Mycobacterium tuberculosis no Brasil. Brasília, DF: Ministério da Saúde; 2018. [ Links ]
7. Borges TS, Sonda EC, Daronco A, Battisti F, Santos MMB, Valim ARM, et al. Prevalência de infecção latente por mycobacterium tuberculosis em profissionais da rede básica de saúde. Rev Bras Promoc Saúde. 2014; 27(2): 269-275. https://doi.org/10.5020/2459 [ Links ]
8. Lima OC, Souza FM, Prado TN, Andrade RLM, Maciel ELN. Analysis of the incidence of latent Mycobacterium tuberculosis infection among primary health care professionals in two Brazilian capitals. J Bras Pneumol. 2020;46(2):e20190201. [ Links ]
9. Marques JBV, Freitas D. Método DELPHI: caracterização e potencialidades na pesquisa em Educação. Pro-Posições. 2018; 29(2):389-415. https://doi.org/10.1590/1980-6248-2015-0140. [ Links ]
10. Melo RP, Moreira RP, Fontenele FC, Aguiar ASC, Joventino ES, Carvalho EC. Critérios de seleção de experts para estudos de validação de fenômenos de enfermagem. Rev Rene. 2011; 12(2):424-431. http://periodicos.ufc.br/rene/article/view/4254 [ Links ]
11. Coluci MZO, Alexandre NMC, Milani D. Construção de instrumentos de medida na área da saúde. Ciênc Saúde Coletiva. 2015; 20(3):925-936. https://doi.org/10.1590/1413-81232015203.04332013 [ Links ]
12. Pasquali L. Psychometrics. Rev Esc Enferm USP. 2009; 43(Esp):992-999. https://doi.org/10.1590/S0080-62342009000500002 [ Links ]
13. Cunha CM, De Almeida Neto OP, Stackfleth R. Principais métodos de avaliação psicométrica da confiabilidade de instrumentos de medida. Rev. Aten. Saúde. 2016;14(49):98-103. [ Links ]
14. Joshi A, Kale S, Chandel S, Pal DK. Likert Scale: Explored and Explained. Curr J Appl Sci Technol. 2015; 7(4):396-403. https://doi.org/10.9734/BJAST/2015/14975 [ Links ]
15. Souza AC, Alexandre NMC, Guirardello EB. Propriedades psicométricas na avaliação de instrumentos: avaliação da confiabilidade e da validade. Epidemiol Serv Saúde. 2017; 26(3): 649-659. https://doi.org/10.5123/S1679-49742017000300022 [ Links ]
16. O'Neill TA. An Overview of Interrater Agreement on Likert Scales for Researchers and Practitioners. Front Psychol. 2017, 8:777. https://doi.org/10.3389/fpsyg.2017.00777 [ Links ]
17. Paulino RG. Validação de instrumento para avaliação da assistência de enfermagem em serviços obstétricos. [Dissertação]. [Brasília]; Universidade de Brasília, 2019. 149p. [ Links ]
18. Pedro AS, Oliveira RM. Tuberculose e indicadores socioeconômicos: revisão sistemática da literatura. Rev Panam Salud Publica. 2013; 33(4):294-301. https://doi.org/10.1590/S1020-49892013000400009 [ Links ]
19. Hino P, Villa TCS, Cunha TN, Santos CB. Padrões espaciais da tuberculose e sua associação à condição de vida no município de Ribeirão Preto. Ciênc Saúde Coletiva; 2011; 16(12):4795-4802. https://doi.org/10.1590/S1413-81232011001300028 [ Links ]
20. Prado TN, Riley LW, Sanchez M, Fregona G, Nóbrega RLP, Possuelo LG, et al. Prevalence and risk factors for latent tuberculosis infection among primary health care workers in Brazil. Cad Saúde Pública. 2017; 33(12):e00154916. https://doi.org/10.1590/0102-311x00154916 [ Links ]
21. Barufaldi LA, Guerra RL, Albuquerque RCR, Nascimento A, Chança RD, Souza MC, et al. Risco de iniciação ao tabagismo com o uso de cigarros eletrônicos: revisão sistemática e meta-análise. Ciênc Saúde Coletiva. 2021; 26(12):6089-6103. https://doi.org/10.1590/1413-812320212612.35032020 [ Links ]
22. Silva DR, Torrico MM, Duarte R, Galvão T, Bonini EH, Arbex FF, et al. Fatores de risco para tuberculose: diabetes, tabagismo, álcool e uso de outras drogas. J Bras Pneumol. 2018; 44(2):145-152. https://doi.org/10.1590/S1806-37562017000000443. [ Links ]
23. Maleta CHM. Epidemiologia e saúde pública. 3. ed. Belo Horizonte: Coopmed, 2014. [ Links ]
24. Ferreira NFR, Rocha GA, Silva ICM, Loureiro LH. Capacitação em saúde: estratégia assistencial aos portadores de tuberculose. Pesquisa em Foco. 2019; 24(2):41-60. https://doi.org/10.18817/pef.v24i2.2114. [ Links ]
25. Santos AP, Silva DR, Mello FCQ. Em época de estratégia pelo fim da tuberculose, é melhor prevenir do que tratar. J Bras Pneumol. 2020;46(2):e20200017. https://doi.org/10.36416/1806-3756/e20200017. [ Links ]
26. Garcia LP. Uso de máscara facial para limitar a transmissão da COVID-19. Epidemiol Serv Saúde. 2020; 29(2):e2020023. https://doi.org/10.5123/S1679-49742020000200021. [ Links ]
27. Ministério da Saúde (BR); Secretaria de Vigilância em Saúde; Departamento de Vigilância das Doenças Transmissíveis; Coordenação-Geral do Programa Nacional de Imunizações. Nota informativa nº 10/2019 CGPNI/DEVIT/SVS/MS. Atualização da recomendação sobre revacinação com BCG em crianças vacinadas que não desenvolveram cicatriz vacinal. Brasília: Ministério da Saúde, 24 jan 2019. [ Links ]
Received: March 31, 2022; Accepted: September 21, 2022











 texto en
texto en 




