My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Enfermería Global
On-line version ISSN 1695-6141
Enferm. glob. vol.22 n.71 Murcia Jul. 2023 Epub Nov 13, 2023
https://dx.doi.org/10.6018/eglobal.553591
Originals
Knowledge and self-efficacy in individuals with type 2 Diabetes Mellitus
1Federal University of Pernambuco. Recife. Brazil
Methodology:
A cross-sectional and quantitative study was conducted in a public hospital in Recife, PE, with 86 individuals with diabetes. Sociodemographic, clinical, and laboratory variables were analyzed, in addition to knowledge and self-efficacy in diabetes, using the Diabetes Knowledge Scale and the Diabetes Management Self-Efficacy Scale, respectively. Descriptive statistics and Student's t-test for independent samples were used to verify homogeneity and compare means.
Results:
Most patients were female, under 60, with low education, low income, and inadequate diabetes control. Insufficient knowledge and low self-efficacy prevailed. Sufficient knowledge positively interfered with self-efficacy regarding physical exercise, and insufficient knowledge interfered with self-efficacy for blood glucose control. Individuals were self-efficacious regardless of age.
Conclusion:
Individuals with diabetes have insufficient knowledge and low self-efficacy, and nurses need to consider these aspects when planning nursing interventions aimed at these persons to promote self-care.
Keywords: Type 2 Diabetes Mellitus; Knowledge; Self-efficacy; Health Promotion
INTRODUCTION
Diabetes Mellitus (DM) is a heterogeneous set of metabolic disorders whose pathogenic mechanism is related to hyperglycemia, resulting from the lack of insulin or inability to perform its functions adequately(1).
In 2021, 536.6 million people with diabetes were reported worldwide, totaling 10.5% of the global population. The total number of people with the disease is estimated to increase to 642.7 million in 2030 and to 783.2 million in 2045. Brazil ranks 6th among the 10 countries with the highest number of people with diabetes (aged 20 to 79 years), accounting for 15.7 million individuals with the disease in 2021 and projections of 23.2 million for 2045(2).
The increase in the prevalence of DM worldwide is mainly linked to the interaction of socioeconomic, demographic, environmental, and genetic factors. Unhealthy diets, increased consumption of processed foods, sedentary lifestyles, obesity, and urbanization are important risk factors for this exponential growth. Thus, measures such as lifestyle changes, including adequate diet, the practice of physical exercises, weight control, and healthy lifestyles, are essential for the prevention and control of the disease, becoming fundamental actions for the therapeutic planning for self-care(3).
The construct of self-efficacy (SE) was introduced by the Social Cognitive Theory (SCT), according to which the term refers to the individual's belief about his/her abilities to perform specific activities or deal with critical situations in order to generate an outcome, determining how he/she thinks, feels, get motivated, and behaves(4).
Regarding the context of DM, particularly type 2 Diabetes Mellitus (T2DM), self-care behaviors include dietary control, regular physical activity, blood glucose and weight monitoring and control, foot care, and medication adherence(5).
As self-efficacy is considered the greatest self-care predictor, its concept has been widely used in studies of self-care behavior in individuals with diabetes, and low self-efficacy is considered an extreme disadvantage in controlling the disease.(6) Knowledge is also fundamental for diabetes control, as it enables increased self-efficacy and self-care skills, resulting in greater satisfaction with the prescribed therapy and improved quality of life(7)).
Poor knowledge is a factor that impacts self-efficacy related to DM, impairing the individual's ability to perform self-care, in addition to interfering with treatment adherence, making it difficult to understand the importance of treatment and glycemic regulation, which may predispose the patient to complications(8). In addition, the relationship between knowledge and self-efficacy in individuals with diabetes is still scarce in the literature, making it necessary to deepen research on the subject(9).
Therefore, investigating the knowledge and self-efficacy of individuals with T2DM can support the planning of healthcare actions and the redirection of assistance to the needs of diabetic patients, in addition to providing self-knowledge and improvements in self-care practices, favoring equiTable, comprehensive, and high-quality care. Given the above, the study aimed to analyze the knowledge and self-efficacy of individuals with type 2 diabetes mellitus.
MATERIALS AND METHODS
A cross-sectional study with a quantitative approach was conducted at the Endocrinology Outpatient Clinic of a public hospital in Recife, Pernambuco, Brazil. The research data consisted of information from the health records of individuals with a medical diagnosis of T2DM assisted at the service's endocrinology outpatient clinic.
The convenience sample included individuals of both sexes diagnosed with T2DM, whose health records were available from August 2019 to March 2020. Subjects who had impaired communication or cognition documented in the health record were excluded due to the possible interference in the collection of research data. Besides, people with chronic complications in advanced stages, including heart failure, hemodialysis, stroke sequelae, amaurosis, previous amputations, or active ulcers in the lower limbs, were excluded. In a preliminary search, we found 550 individuals with the disease in March 2019, but only 385 met the eligibility criteria.
Sample calculation was performed using the formula [z2σ2N/d2(N-1)+z2σ2], adopting the number of individuals with type 2 diabetes assisted at the outpatient clinic HC/UFPE, N = 385, a 95% confidence level, z = 1.96, an expected variance of the self-efficacy score (σ) of 0.6,(10) and a margin of error in the mean estimate (d) of 0.146. The resulting sample size was 86 participants.
For data collection, a structured instrument was used, consisting of identification data, sociodemographic variables, clinical conditions, and the Brazilian versions of the Diabetes Knowledge Scale (DKN-A)(11), which assesses diabetes knowledge, and Diabetes Management Self-Efficacy Scale (DMSES), which measures diabetes-related self-efficacy.(12)
Knowledge about diabetes was measured using the DKN-A questionnaire consisting of five categories (basic physiology, hypoglycemia, diet and nutrition, sick day management, and general care) and 15 (fifteen) multi-item items on different aspects related to general knowledge about the disease. The assigned value consists of 1 (one) for correct answer and 0 (zero) for the wrong answer. In questions 1 to 12, a single correct answer is required; items 13 to 15, on the other hand, require two responses, and both must be checked to obtain a score of 1 (one). The final score ranges from 0 to 15 points, and a value greater than or equal to 8 (eight) indicates good knowledge of DM.
Self-efficacy was assessed using the DMSES scale, translated, adapted, and validated for Brazilian Portuguese, obtaining 0.78 as Cronbach's alpha for the total scale. The DMSES is a Likert-type scale with 20 items divided into four factors (specific nutrition and weight, general nutrition and medical treatment, exercise, and blood glucose management) assessing the ability of individuals with T2DM to perform diabetes self-care behaviors. The scale includes three types of activities: (1) diabetes-specific activities (taking oral antidiabetic medications or insulin, following a diet plan, and engaging in physical activities), (2) self-observation activities (monitoring/observing and recording blood or urine glucose levels, body weight, foot skin conditions, and general health conditions), and (3) self-regulation activities (correction of hypo and hyperglycemia, vacation planning, changes in diet, and self-regulation in situations of weight gain, acute illness, and stress). The overall mean of the instrument determines the self-efficacy score, and the higher means indicate better self-efficacy.
Individuals with T2DM were recruited while waiting for an appointment at the endocrinology outpatient clinic, with a subsequent invitation to participate in the study. Data were collected after acceptance and consent, and the individual interviews were conducted by a duly trained team, in a reserved room, through the application of a structured instrument, in addition to the knowledge and self-efficacy scales.
The data obtained were analyzed using the Statistical Package for the Social Sciences (SPSS) version 21.0 (SPSS Inc., Chicago, IL, USA) through descriptive data analysis to characterize the sample regarding sociodemographic and clinical variables. Simple, absolute, and percentage frequencies were obtained for categorical variables, in addition to central tendency measures (mean, median, and mode) and dispersion measures (standard deviation, interquartile range, minimum and maximum) for quantitative variables, after testing for normal distribution.
Bivariate analyses of the association between knowledge about diabetes and self-efficacy were conducted. As the variables were normal, the Student's t-test was used for independent samples to verify homogeneity and mean comparison, adopting p<0.05 as the significance level.
The research followed the basic bioethics principles (autonomy, non-maleficence, beneficence, and justice) under Brazilian Resolution nº 466/12. The study is part of a larger project entitled "EDUCATION IN DIABETES: knowledge, self-efficacy, and self-care practices", which was approved by the Research Ethics Committee of the Health Sciences Center of the Federal University of Pernambuco (CEP/UFPE) under the Certificate of Presentation of Ethical Appreciation (CAEE) number 12615619.0.0000.5208, approving the use of research data.
RESULTS
Of the 86 individuals with T2DM, the majority were female (74.4%), aged below 60 years (52.3%), with a mean age of 58.50 (±10.04), with a partner (54.7%), with less than or equal to 8 years education (59.2%), and with a monthly income equal to or less than 1 minimum wage (82.9%). As for the clinical characteristics, 55.8% had the diagnosis of DM for more than 10 years (14.28±10.83), and 66.3% reported diabetes-related complications, especially ophthalmological (56.1%), neurological (56.1%), and cardiovascular (21.1%) complications. Of the total, 81.4% reported the presence of comorbidities, including hypertension (91.4%), dyslipidemia (47.1%), and obesity (31.4%). As for the glycated hemoglobin (A1c) levels, 70.0% had values greater than 7% (8.64%±2.46%).
Knowledge about diabetes was insufficient (52.3%) among respondents (7.55±2.77). The average self-efficacy was 2.19 (±0.79), and when categorized into two strata, 55.8% (n=48) of participants had low self-efficacy, with emphasis on the domains of general nutrition and medical treatment (1.82±0.60) and blood glucose (1.97±1.21). On the other hand, they were more self-efficient in activities related to specific nutrition and weight (2.57±1.21).
Table 1. Distribution of central tendency measures of self-efficacy of individuals with type 2 diabetes mellitus. Recife/PE, 2019-2020.

Sufficient knowledge positively interfered with self-efficacy regarding physical exercise (2.68±1.36). On the other hand, insufficient knowledge interfered with self-efficacy regarding blood glucose correction (2.24±1.33). Concerning the specific items of each domain of the scale, sufficient knowledge interfered positively with the item "I am able to do more physical activity if the doctor advises me to do so" (2.88±1.76), and insufficient knowledge interfered with the item "I am able to maintain my eating plan when I am ill (with flu, cold or infection)" (2.58 ± 1.59) and "I am able to increase my blood sugar when the sugar level is too low" (2.47±1.69) (Table 2).
Table 2. Assessment of self-efficacy items according to the knowledge of individuals with diabetes about the disease. Recife/PE, 2019-2020.

*Student T-test p-value for independent samples
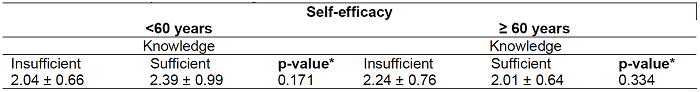
It is observed that individuals were self-efficacious regardless of age. However, knowledge of diabetes was inversely proportional to advancing years. However, the evaluated factors’ average comparison test was not significant (Table 3).
DISCUSSION
Insufficient knowledge and low self-efficacy were prevalent among the participants. These results may indicate difficulties coping with the disease and compromised self-care, as mentioned in other studies(13).
Concerning the participants' profile, there was a predominance of females in our study, which confirm the results of other studies(5,14). This result can be explained because women have greater longevity and a greater tendency to attend health services, being more attentive to changes in their body physiology, leading to a greater probability of being diagnosed(15).
The predominance of persons younger than 60 years of age has also been demonstrated in previous publications.(5 10 14 16. The literature suggests that the diagnosis of diabetes has been increasingly frequent in young people, which makes it clear that health services need to develop strategies for self-care that include different age groups, with emphasis on the prevention and control of modifiable risk factors such as sedentary lifestyle, obesity, and dietary factors, in addition to the use of alcohol and tobacco(17).
The characteristics of low education and low income were also found in patients with diabetes in other regions of Brazil, confirming the basic characteristics of this population in a large part of the country(10,18)). Low education is associated with insufficient knowledge about diabetes and can make diabetes self-management difficult, contributing to inadequate self-care in managing the disease.(19) Inadequate diabetes control prevailed, one of the main problems among individuals with diabetes, which can lead to several complications, including neuropathy and retinopathy, prevalent in the study participants(17).
Insufficient knowledge about diabetes was predominant, a result similar to that found in the study by Vietta et al.(20), in which insufficient knowledge was found in 81.3% of the participants. Knowledge is essential for preventing diabetes and its complications, as it provides subsidies for disease control.(14) Insufficient knowledge favors the aggravation of the disease, resulting in complications(17) and compromised quality of life. Effective individual and collective educational actions with adequate information and a multi and interdisciplinary approach are necessary to facilitate recognizing unhealthy behaviors and changing lifestyles(1).
Participants in this study had a low self-efficacy score. A similar result was found in a study in northeastern Brazil(10), in which 50.9% of participants had low self-efficacy. Low self-efficacy is related to declining quality of life because it reduces diabetes control, leading to complications(20). Individuals with poor self-efficacy do not believe in their ability to care for themselves and tend to abandon treatment in the face of difficulties and adverse experiences that they may experience(13).
The participants were less self-efficacious concerning the general nutrition and medical treatment domains, diverging from Reisi et al.'s findings, which showed that most participants were more self-efficacious concerning medical treatment(16). The lower self-efficacy for medication intake can be explained because it requires persistence and commitment despite being a simple task.
Low self-efficacy concerning glycemic control may be related to the lack of access to the glucometer and reagent strips due to low family income and insufficient knowledge since subjects often do not value the instructions given on glycemic control because they do not understand the reasons why they are important(10.13). Thus, the need to educate patients about self-monitoring blood glucose and glycemic control is highlighted to increase their self-efficacy to perform this task.
The specific nutrition and weight domain had the highest self-efficacy scores, indicating that individuals were more self-efficacious in these aspects, which differs from Medina et al.'s findings that this domain had the lowest average(14). Saad et al. found that patients who followed specific diet-related behaviors had significantly lower glycated hemoglobin than those who did not adopt these behaviors, generating greater glycemic control(22), which suggests that individuals with high self-efficacy in diet control are more likely to practice it.
In the present study, individuals with sufficient knowledge about diabetes had a greater self-efficacy than those with insufficient knowledge, confirming the findings of a prior study which showed that people with a better knowledge of diabetes have better self-efficacy(23).
Sufficient knowledge positively interfered with self-efficacy regarding the practice of physical exercise. Thus, it is clear that the individuals who want to perform this type of activity have sufficient knowledge about diabetes and, therefore, understand the importance of doing so. Despite having an important impact on glycemic control and reducing the risk of complications related to diabetes(24), physical exercise represents one of the pillars of the treatment with low adherence, mainly due to the difficulty in implementing lifestyle changes. Santos et al.(25) observed that adherence to non-drug treatment, including physical exercise, is usually inferior to adherence to drug treatment.
High self-efficacy scores are associated with lower glycated hemoglobin levels, as it improves individuals' understanding of their condition and increases their motivation to manage the disease.(21) The greater the self-efficacy, the more vigorous and persistent the efforts and the greater the visualization of success scenarios and the expectation of favorable results by individuals concerning disease control(4).
Insufficient knowledge in the general nutrition and drug treatment domain influenced the item "I am able to maintain my eating plan when I am ill (with flu, cold or infection)". It is important to highlight the importance of glycemic control in these situations because, in most cases, the therapeutic goal is difficult to achieve and maintain, not only because it is difficult to maintain a healthy diet but also because even patients who believe that they can control their glucose levels in these situations have insufficient knowledge, limiting their ability to perform glycemic control correctly(1,13).
In addition, self-efficacy is associated with eating habits since people with diabetes who perceive high self-efficacy are more motivated and feel confident to follow dietary recommendations.(26) Thus, both knowledge and self-efficacy support patterns of healthy eating behavior, becoming important tools for the treatment, as they can impact the management of eating behavior with improved disease control and quality of life(27).
In the physical exercise domain, emphasis was placed on the item "I am able to do more physical activity if the doctor advises me to do so". Sufficient knowledge makes expanding the universe of exercises possible, allowing the patient to perform other types of physical activities besides walking, considering his preferences, availability, and physical conditioning. It can be inferred that although the individual knows the disease, the necessary treatment, and the possible complications, he may not follow the dietary and physical activity recommendations for diabetic patients, thus impairing weight reduction and glycemic control(13).
As for the blood glucose domain, the assessment of the item "I am able to increase my blood sugar when the sugar level is too low" showed that individuals with insufficient knowledge had greater belief in their ability to correct hypoglycemia. However, their knowledge is insufficient, which may affect glycemic control. The finding above can be correlated with the study by Borba et al.(28), which found that most respondents could not identify the causes of hypoglycemia and did not know how to manage it.
Hypoglycemia is the main barrier in patients with DM and a limiting factor to achieving euglycemia, becoming one of the main complications of T2DM, and favoring a greater risk of fainting, falls, seizures, and cognitive decline in the elderly(29). Acquiring knowledge about diabetes plays a key role in optimizing glycemic control in patients with T2DM.
Individuals with diabetes deal with issues that can interfere with glycemic control, such as financial difficulties, insatiable cravings for sweet foods, overeating, and easy access to carbohydrate-rich foods. Adapting to a new lifestyle is challenging for these people, mainly because it requires motivation and confidence to acquire new eating habits and resist consuming unhealthy foods. In this way, people with a high self-efficacy score are motivated by the situation experienced and maintain enthusiasm, even when in a difficult phase of treatment(14).
We observed that elderly people with insufficient knowledge about diabetes had greater self-efficacy, but this finding was not statistically significant. A long time of diagnosis and educational level influence time and access to information. With the technological revolution, many elderly people now have more access to information, but the sources are not always reliable. Due to the context of the COVID-19 pandemic, several negative implications were generated due to social isolation, such as the impairment of health monitoring and the limitations of access to professional guidance and glycemic control(2,5).
The assumption prevails that as the duration of diabetes diagnosis extends, the patients may experience a decline in blood glucose control as the disease progresses, although they might possess a more comprehensive comprehension of the disease.(30) Nevertheless, a prior study conducted in Recife with a sample of 202 older adults has demonstrated that 77.7% of the participants had inadequate knowledge regarding their illness and treatment.(28) It has also been highlighted that insufficient knowledge about diabetes is a risk factor for patients with low education levels, besides indicating a positive association between older age, lower education, lower socioeconomic status, and inadequate knowledge scores. Consequently, patients with diabetes, especially older adults, must augment their knowledge about diabetes to enhance their self-care.
Although knowledge is crucial, it alone cannot instigate behavior modification and self-efficacy. Individuals with inadequate knowledge and skills, particularly in tasks related to glycemic control, tend to encounter challenges in adopting favorable diabetes self-care behaviors(13, 28) Consequently, to foster self-efficacy, it is imperative to possess knowledge concerning the self-care actions necessary for managing diabetes.
Therefore, knowledge and self-efficacy become important tools to be used by health professionals to promote self-care practices among individuals with T2DM and must be based on educational actions, with active methodologies that focus on promoting knowledge, autonomy, self-efficacy, and self-care, leading to adherence to the pillars of disease treatment.(30) For this, subjects must participate in treatment planning, actively learn about the disease, expose their feelings, and acquire the necessary skills.
The assessment of knowledge and self-efficacy is essential, as it allows the identification of beliefs and resources involved and enables the elaboration of a unique and effective treatment plan, in addition to guiding health professionals regarding the approaches to be adopted in the health promotion actions and during consultations, involving existing knowledge and offering new information and learning opportunities(14,28).
The current study encountered limitations, including a reduced sample size, resulting from the need to halt the research due to the COVID-19 pandemic. The studied population, a high-risk group for the severity of COVID-19 infection, also contributed to the reduced sample size. Additionally, the study was conducted in a single center. Furthermore, the limited number of studies that investigate the various domains of the self-efficacy scale and their association with knowledge about diabetes pose a challenge to this field of research.
CONCLUSION
Study participants had insufficient knowledge about diabetes and low self-efficacy in controlling the disease. Sufficient knowledge positively interfered with self-efficacy regarding physical exercise, and insufficient knowledge interfered with self-efficacy for blood glucose control. Individuals were self-efficacious regardless of age, and diabetes knowledge was inversely proportional to advancing age, but the correlations involving these factors were not statistically significant.
Evaluating the correlation between knowledge about diabetes and self-efficacy constitutes a valuable source of information to guide the design of tailored interventions aimed at enhancing these domains and, consequently, promoting a positive impact on the quality of life of individuals with diabetes, as well as fostering glycemic control.
REFERENCIAS
1. Sociedade brasileira de diabetes. Diretrizes da Sociedade Brasileira de Diabetes. [Internet]. São Paulo: Editora Clannad, 2019. [citado 2022 Jan 03]. Disponível em: https://www.diabetes.org.br/publico/diabetes/diagnostico-e-tratamento [ Links ]
2. International diabetes federation. IDF Diabetes Atlas. [Internet] 10. ed.; 2021. [citado 2022 Jan 03]. Disponível em: https://diabetesatlas.org/idfawp/resource-files/2021/07/IDF_Atlas_10th_Edition_2021.pdf. [ Links ]
3. Muzy J, Campos MR, Raulino IE, da Silva R, Schramm JMA. Prevalência de diabetes mellitus e suas complicações e caracterização das lacunas na atenção à saúde a partir da triangulação de pesquisas. Cad. Saúde Pública. 2021; 37(5):e00076120. https://doi.org/10.1590/0102-311X00076120 [ Links ]
4. Bandura A. Applying Theory for Human Betterment. Perspectives on Psychological Science. 2019; 14(1):12-15. https://doi.org/10.1177/1745691618815165 [ Links ]
5. Tharek Z, Ramli AS, Whitford DL, Ismail Z, Mohd Zulkifli M, Ahmad Sharoni SK, et al. Relationship between self-efficacy, self-care behaviour and glycaemic control among patients with type 2 diabetes mellitus in the Malaysian primary care setting. BMC Fam Pract. 2018 Mar 9;19(1):39. https://doi.org/10.1186/s12875-018-0725-6 [ Links ]
6. Qin W, Blanchette JE, Yoon M. Self-Efficacy and Diabetes Self-Management in Middle-Aged and Older Adults in the United States: A Systematic Review. Diabetes Spectrum, 2020; 33(4):315-323. https://doi.org/10.2337/ds19-0051 [ Links ]
7. Nouwen A, Speight J, Pouwer F, Holt RIG. How psychosocial and behavioural research has shaped our understanding of diabetes. Diabet Med. 2020 Mar;37(3):377-379. https://doi.org/10.1111/dme.14254 [ Links ]
8. Mazzuchello FR, Tuon L, Simões PW, Mazon J, Dagostin VS, Tomasi CD, et al. Knowledge, attitudes and adherence to treatment in individuals with hypertension and diabetes mellitus. O mundo da saúde, 2016 dez 30; 40(4):418-432. https://doi.org/10.15343/0104-7809.20164004418432 [ Links ]
9. Figueira ALG, Gomes-Villas Boas LC, Coelho ACM, Foss-Freitas MC, Pace AE. Educational interventions for knowledge on the disease, treatment adherence and control of diabetes mellitus. Rev. Latino-Am. Enfermagem. 2017;25:e2863. https://doi.org/10.1590/1518-8345.1648.2863 [ Links ]
10. Santos CMJ, Faro A. Autoeficácia, lócus de controle e adesão ao tratamento em pacientes com diabetes tipo 2. Rev. SBPH [Internet]. 2018 Jun [citado 2022 Jan 16];21(1):74-91. Disponível em: http://pepsic.bvsalud.org/scielo.php?script=sci_arttext&pid=S1516-08582018000100005&lng=pt. [ Links ]
11. Torres HC, Hortale VA, Schall VT. Validação dos questionários de conhecimento (DKN-A) e atitude (ATT-19). RevSaude Publica. 2005; 39(6):906-11. https://doi.org/10.1590/S0034-89102005000600006 [ Links ]
12. Pace AE, Gomes LC, Bertolin DC, Loureiro HMAML, Van der Bijl JJ, Shortridge-Baggett L. Adaptation and validation of the Diabetes Management Self-Efficacy Scale to Brazilian Portuguese. Rev. Latino-Am. Enfermagem. 2017;25:e2861. https://doi.org/10.1590/1518-8345.1543.2861. [ Links ]
13. Sousa MC, Malaquias BSS, Chavaglia SRR, Ohl RIB, Paula FFS, Silva KS, et al. Self-efficacy in elderly with type 2 Diabetes Mellitus. Rev Bras Enferm. 2020;73(Suppl 3):e20180980. http://dx.doi.org/10.1590/0034-7167-2018-0980 [ Links ]
14. Medina LAC, Silva RA, de Sousa Lima MM, Barros LM, Lopes ROP, Melo GAA, et al. Correlation Between Functional Health Literacy and Self-efficacy in People with Type 2 Diabetes Mellitus: Cross-sectional Study. Clin Nurs Res. 2022 Jan;31(1):20-28. https://doi.org/10.1177/10547738211006841 [ Links ]
15. Batista IB, Pascoal LM, Gontijo PVC, Brito PS, Sousa MA, Santos Neto M, et al. Association between knowledge and adherence to foot self-care practices performed by diabetics. Rev Bras Enferm. 2020; 73(5):e20190430. http://dx.doi.org/10.1590/0034-7167-2019-0430 [ Links ]
16. Reisi M, Mostafavi F, Javadzade H, Mahaki B, Tavassoli E, Sharifirad G. Impact of Health Literacy, Self-efficacy, and Outcome Expectations on Adherence to Self-care Behaviors in Iranians with Type 2 Diabetes. Oman Med J. 2016 Jan;31(1):52-9. https://doi.org/10.5001/omj.2016.10. [ Links ]
17. Lima AP, Benedetti TRB, Rech CR, Cardoso FB, Portella M. Conhecimento e atitude sobre a diabetes tipo 2 em idosos: Estudo de base populacional.. Cien Saude Colet. 2020; 25(2). https://doi.org/10.1590/1413-81232020252.14662018. [ Links ]
18. Teston EF, Serafim D, Cubas MR, Haddad MCL, Marcon SS. Fatores associados ao conhecimento e à atitude em relação ao diabetes mellitus. Cogitare Enfermagem. 2017; 22(4). http://dx.doi.org/10.5380/ce.v22i4.50850 [ Links ]
19. Amaral VRS, Ribeiro IJS, Rocha RM. Factors associated with knowledge of the disease in people with type 2 Diabetes Mellitus. Invest. Educ. Enferm. 2021; 39(1):e02. https://doi.org/10.17533/udea.iee.v39n1e02. [ Links ]
20. Vietta G, Volpato G, Kretzer M, da-Gama F, Nazário N, Pereira E. Impacto do conhecimento nas atitudes, no sofrimento e qualidade de vida do paciente diabético. Arquivos Catarinenses de Medicina [Internet]. 2019 Dez 26; [Citado em 2022 Jan 03]; 48(4): 51-61. Disponível em: http://www.acm.org.br/acm/seer/index.php/arquivos/article/view/520 [ Links ]
21. Hartono D, Salam A, Prasetyanto D, Handayani E, Hasina S. The Correlation Between Self Efficacy and the Stability of Blood Sugar Levels on Type II Diabetes Mellitus Patients. Jurnal Keperawatan. 2021; 13(2), 589-596. https://doi.org/10.32583/keperawatan.v13i2.1730 [ Links ]
22. Saad AMJ, Younes ZMH, Ahmed H, Brown JA, Al Owesie RM, Hassoun AAK. Self-efficacy, self-care and glycemic control in Saudi Arabian patients with type 2 diabetes mellitus: A cross-sectional survey. Diabetes Res Clin Pract. 2018 Mar;137:28-36. https://doi.org/10.1016/j.diabres.2017.12.014. [ Links ]
23. Lee SK, Shin DH, Kim YH, Lee KS. Effect of Diabetes Education Through Pattern Management on Self-Care and Self-Efficacy in Patients with Type 2 Diabetes. Int J Environ Res Public Health. 2019 Sep 9;16(18):3323. https://doi.org/10.3390/ijerph16183323 [ Links ]
24. Mirtha LT, Permatahati V. The effectiveness of aerobic exercise in improving peripheral nerve functions in Type 2 diabetes Mellitus: an evidence-based case report. [Internet] Acta Med Indones. 2018 [citado 2022 Jan 03]50(1):82-7. Disponível em: https://www.ncbi.nlm.nih.gov/pubmed/29686181 [ Links ]
25. Santos AL, Marcon SS, Teston EF, Back IR, Lino IGT, Batista VC, et al. Adesão ao tratamento de diabetes Mellitus e relação com a assistência na Atenção Primária. REME - Rev Min Enferm. 2020 [citado em 2022 Jan 03];24:e-1279. https://doi.org/10.5935/1415-2762.20200008 [ Links ]
26. Winahyu KM, Anggita R, Widakdo G. Characteristics of Patients, Self-Efficacy and Quality of Life among Patients with Type 2 Diabetes Mellitus Jurnal Keperawatan Padjadjaran. 2019; 7(3). https://doi.org/10.24198/jkp [ Links ]
27. Bano A, Afzal M, Sarwar H, Waqas A, Kousar S, Gulzar S. Dietary knowledge, Attitude and Practices of Diabetes Patients at Services Hospital Lahore. International Journal of Applied Sciences and Biotechnology. 2017; 5(2), 227-236. https://doi.org/10.3126/ijasbt.v5i2.17625 [ Links ]
28. Borba AKOT, Arruda IKG, Marques APO, Leal MCC, Diniz AS. Conhecimento sobre o diabetes e atitude para o autocuidado de idosos na atenção primária à saúde. Ciência & Saúde Coletiva. 2019; 24(1):125-136. https://doi.org/10.1590/1413-81232018241.35052016 [ Links ]
29. Romero I, Sousa R, de Oliveira IF, Pedro AB, Urza J. Hipoglicemia em doentes diabéticos idosos: experiência de uma unidade de diabetes. [Internet] Rev Clin Hosp Prof Dr Fernando Fonseca. 2017[ Citado 2022 Jan 03]; 5 (1/2): 11-18. Disponível em: https://revistaclinica.hff.min-saude.pt/index.php/rhff/article/view/234/129 [ Links ]
30. Hurst CP, Rakkapao N, Hay K. Impact of diabetes self-management, diabetes management self-efficacy and diabetes knowledge on glycemic control in people with Type 2 Diabetes (T2D): A multi-center study in Thailand. PLoS One. 2020 Dec 31;15(12):e0244692. https://doi.org/10.1371/journal.pone.0244692 [ Links ]
Received: January 11, 2023; Accepted: March 05, 2023











 text in
text in