Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Enfermería Global
versión On-line ISSN 1695-6141
Enferm. glob. vol.22 no.71 Murcia jul. 2023 Epub 13-Nov-2023
https://dx.doi.org/10.6018/eglobal.550611
Originals
Quality of life and self-perceived health of patients subjected to radical prostatectomy and the social determinants of health
1Federal University of São Carlos. São Carlos. Brazil
2Pequeno Príncipe Hospital. Curitiba. Brazil
Introduction:
The self-perception of health and quality of life in men subjected to radical prostatectomy can be influenced by the Social Determinants of Health (SDHs); therefore, exploring this relationship contributes to the development of health care measures.
Objective:
To identify associations between the SDHs and quality of life and self-perceived health in men subjected to radical prostatectomy.
Method:
A cross-sectional study with quantitative analysis, which had men subjected to radical prostatectomy as participants, interviewed using instruments to characterize the SDHs, Quality of Life (QoL) and self-perceived health. The data were analyzed using descriptive and correlational statistics. The study was approved by the Research Ethics Committee.
Results:
The participants were 33 men with a mean age of 66.8 years old, mostly white-skinned, with a spouse, professing some religion and with complete or incomplete Elementary School. They presented preserved levels of QoL and self-perception of health. Self-perceived health was associated with religion and with owning a house; QoL was associated with religion, type of surgical approach, marital status, having someone in the family with prostate cancer and schooling.
Conclusion:
There was an association between the SDHs and QoL and self-perceived health in men subjected to radical prostatectomy.
Keywords: quality of life; self-perception of health; social determinants of health; prostatectomy; nursing
INTRODUCTION
The estimate on cancer points out that prostate tumors represent the most common type among men in all regions of the country; nevertheless, it is the second most recurrent type of cancer in the world, being more frequent in Australia, New Zealand and European countries and ranking fifth among the causes of death due to cancer(1).
Diagnostic suspicion of prostate cancer is based on the elevation of the prostate-specific antigen (PSA) serum levels and, clinically, by detecting changes in consistency or nodules in the prostate gland by digital rectal examination(2). Evolution is silent and, when present, the symptoms are dysuria, urinary hesitation, urinary urgency, incontinence, reduced urinary stream, sensation of incomplete emptying of the bladder and hematuria(2).
In relation to the treatment, it must be individualized and the tumor stage should be taken into account. This can vary between radical prostatectomy, radiotherapy, brachytherapy, active surveillance and hormone therapy(2). Radical prostatectomy is considered the gold standard for the treatment of prostate cancer; however, there are reports of complications from this surgery capable of compromising functional results, responsible for affecting quality of life, health and satisfaction with the surgery. The functional results of radical prostatectomy are related to changes in the neurovascular bundles during surgery associated with the occurrence of urinary incontinence and erectile dysfunction(3).
The World Health Organization (WHO) defines Quality of Life (QoL) as “an individual's perception of their position in life, in the context of the culture and value systems in which they live, and in relation to their objectives, expectations, criteria and concerns”, as a broad concept affected in a complex way by physical health, social relationships, personal beliefs and their relationship with characteristics of their environment(4).
The impact of radical prostatectomy on men's QoL was documented by a systematic review of 18 studies, which found that, when comparing the different treatment modalities for prostate cancer (active surveillance, surgery, radiotherapy and brachytherapy), surgery was the modality that most compromised men's QoL, mainly due to the occurrence of complications, while active surveillance exerted the least negative impact on QoL(5).
However, it is important for comprehensive and better quality care for men to acknowledge that radical prostatectomy and its functional results can be associated with other outcomes that require professional identification and intervention, such as satisfaction with the surgery, self-perception of health, self-esteem, anxiety and depression(3).
Self-perception of health is the way in which people perceive and understand their own health, and can be influenced both by individual behaviors (related to lifestyles) and by collective behaviors in a given community. It depends on economic conditions, availability of preventive information related to basic health care and availability or ease of access to a health care unit; in addition, its interference is well-known in adherence to disease prevention measures, in the search for care health appointments, and in difficulty performing usual activities(6,7).
A study carried out in southern Brazil showed that people with high schooling levels evaluated their own health as negative, in opposition to those with lower schooling levels, who considered themselves to be in good health. In this way, the relationship between health self-perception and the degree of individual knowledge is reinforced(6). In addition, another study highlighted that men self-assessed their health as positive when compared to women, which was pointed out by the authors as a reason for men to seek fewer care appointments in health services(8).
Based on all this evidence, it is possible to consider that self-perception of health and quality of life can be influenced by social characteristics within which life takes place, such as the Social Determinants of Health(9) and, therefore, knowing this relationship contributes to the development of disease prevention measures and interventions more targeted to individual needs or to those of specific groups.
The Social Determinants of Health (SDHs) consist of the social conditions in which people live and work, a fact with repercussions on health(10). The SDHs care models seek to know such conditions in populations and to implement measures capable of promoting equality in health, which is the “absence of unfair and avoidable or remediable differences between socially, economically, demographically and geographically defined population groups”(11).
In Brazil, the Dahlgren and Whitehead model was chosen by the National Commission on Social Determinants of Health to explore relationships and mediations between the health social determination levels and the genesis of inequalities. This model groups the SDHs into different layers, according to the coverage level: (1) the micro-layer is linked to the individual, considered the center of the model, comprising age, gender and hereditary factors; (2) the second layer concentrates the individual characteristics, such as behavior and lifestyle; (3) the third layer concentrates support social networks and community networks; (4) the fourth layer presents factors related to the living and working conditions; and (5) the fifth layer groups macro-determinants that influence all other layers and groups factors related to economic, cultural and environmental conditions of society, including globalization(11).
Considering the knowledge about the impact of radical prostatectomy on men's quality of life and health self-perception, this study sought to answer the following question: Are the SDHs associated with QoL and self-perceived health of men subjected to radical prostatectomy? Therefore, its objective was to identify the associations of the SDHs with the quality of life and self-perceived health of men subjected to radical prostatectomy.
MATERIAL AND METHOD
An observational, cross-sectional and quantitative analysis study was carried out in a municipality located in the inland of the state of São Paulo, in its central region. Data collection was performed at the municipal Oncology Outpatient Clinic, which exclusively serves Unified Health System users. This research was approved by the Research Ethics Committee (CAAE: 81194217.3.0000.5504).
The study population consisted of men subjected to radical prostatectomy and convenience sampling was used to comprise the sample. The participants were selected according to the following inclusion criteria: age greater than or equal to 18 years old; verbal communication skills; and possessing a minimum cognitive level to understand the items that make up the data collection instrument. The exclusion criterion was having undergone the surgery more than 10 years ago.
The subjects that met the inclusion criteria were invited to participate in the study when they returned to the outpatient consultation with the urologist at the service, while awaiting their appointment in the waiting room. After expressing their consent by signing the Free and Informed Consent Form (FICF), they were included and interviewed for data collection. During the interview, a sociodemographic characterization form, an instrument for analyzing self-perception of health and an instrument for assessing quality of life were completed.
The sociodemographic characterization form was prepared according to the model of the Social Determinants of Health(11), and comprised the determinants from four layers of this model, which were grouped into four parts. The first part included the identification and individual factors, such as age and skin color; the second part represented the investigation of hereditary factors, such as having a diagnosis of cancer or prostate cancer in the family. The third part comprised individual characteristics and lifestyle, such as marital status, religion, schooling, habits (smoking, drinking and physical activity), hospitalization history, history of other surgeries, presence of comorbidities and prostatectomy complications (stress urinary incontinence and sexual dysfunction). The fourth and last part of the instrument involved an investigation into the social support networks and community networks through the following variables: number of children, who they live with, characteristics of the house, transportation means used, garbage collection, basic sanitation, occupation and family monthly income.
To establish the occurrences of stress urinary incontinence and sexual dysfunction, the defining characteristics of both NANDA International Nursing diagnoses(12) were analyzed together with the participants, supporting the establishment of diagnoses by the authors.
The analysis of health self-perception was performed by answering the following question: “How do you consider your health status?” and had the following descriptors as answer options: Very bad, Bad, Fair, Good and Excellent. To complement the health self-perception assessment, a Visual Analog Scale was used, with a 100 mm line and descriptors at the ends, on the left: “I notice that my health is very bad” and on the right: “I notice that my health is excellent”. The participants marked along the line how they perceived their health at that moment and, later on, the point indicated was measured using a ruler. To interpret the result it was considered that the higher the score, the better the participant's self-perception of health. These self-perceived health analysis strategies were followed considering the approach taken in other studies(6-8).
Quality of Life was assessed by means of WHOQOL-bref, an instrument developed by the World Health Organization (WHO) and validated for use in the Brazilian population(13), consisting of 26 questions, two of which are general questions, and 24 questions comprising fundamental facets of this construct. The WHOQOL-bref items are organized into four domains: Physical (seven items), Psychological (six items), Social Relationships (three items) and Environment (eight items). Each item is answered by means of a five-point Likert scale, adding up the values to obtain a total score. Higher scores represent a better Quality of Life assessment.
The data obtained were organized in Microsoft Excel 2010® and processed in the Software Statistical Package for Social Sciences (SPSS)®, version 23. The variables were analyzed using descriptive statistics resorting to absolute and relative frequency, mean, standard deviation, median, and minimum and maximum values. Inferential analyses of the associations between the social and health determinants and self-perceived health and quality of life were investigated using Fisher's Exact test for the categorical variables, Wilcoxon or Kruskall-Wallis test between the numerical and categorical variables, and Spearman's correlation coefficient between the numeric variables. The statistical analyses used non-parametric tests, as normal distribution was not observed for all the variables investigated, according to the Shapiro-Wilk normality test. A 5% significance level was adopted for the statistical analyses employed.
RESULTS
During the data collection period, 36 patients were eligible for the study, although three of them did not agree to participate in the study; therefore, the final sample consisted of 33 participants. As for the individual factors, the mean age was 66.8 years old, varying from 41 to 82, and 16 participants (48.5%) declared themselves to be white-skinned. In relation to the hereditary factors, most of the participants had a family history of cancer (n=26; 78.9%). In turn, regarding the individual characteristics and lifestyle, 29 were married and were Catholics (87.9%), only 8 participants reported having completed High School (4.2%), five participants were smokers (84.8%), six reported drinking alcohol (18.2%) and 24 practiced physical activity (72.7%). Table 1 presents the sociodemographic and clinical characterization, considering the social and health determinants.
Table 1. Sociodemographic and clinical characterization of the patients subjected to prostatectomy (n=33). São Carlos, 2019.

Source: Research data, 2019.
As for the evaluation of health self-perception through the Likert scale, with five possible answers (Very bad, Bad, Fair, Good and Excellent), one participant (3.0%) evaluated his self-perception of health as Very bad, two ( 6.1%) as Bad, 11 (33.3%) as fair, 14 (42.4%) as good and five (15.1%) as excellent. The mean self-perceived health assessed by the Visual Analog Scale was 6.4 and varied from zero to 9.7, with a standard deviation of ±2.2. Values close to zero represented health perception as Very bad.
The Quality of Life mean score obtained in WHOQOL-bref was 14.3, varying between 9.6 and 17.8 points and with a standard deviation ±1.9. Values of 14.9, 14.7, 13.5 and 14.1 were obtained in the Physical, Psychological, Social Relationships and Environment domains, respectively. Table 2 shows the results obtained on Quality of Life, as assessed by WHOQOL-bref.
Table 2. Mean, standard deviation and ranges corresponding to the WHOQOL-bref total domain scores (n=33). São Carlos, SP. 2019.
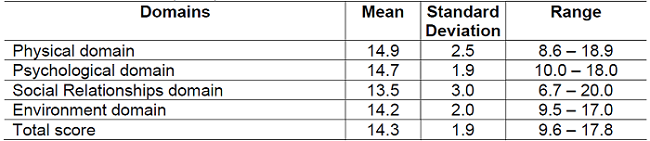
Source: Research data, 2019.
The associations of the social determinants of health, self-perceived health and quality of life (total score and domains) of men subjected to radical prostatectomy were examined and, from these investigations, it was found that self-perceived health was associated with the person professing a religion (p=0.004) and owning their own house (p=0.01); religion was also associated with the results obtained in the total Quality of Life score (p=0.024), in the Social Relationships (p=0.023) and Environment (p=0.04) domains. The type of surgical approach was associated with the total Quality of Life score (p=0.008), marital status with the Physical domain (p=0.047), having someone in the family with prostate cancer with the Psychological domain (p=0.027), and schooling was related to the Social Relationships domain (p=0.019).
DISCUSSION
This study sought to analyze the relationship between the SDHs and the quality of life and self-perceived health of men subjected to radical prostatectomy. The SDHs are aspects of people's lives considered essential for the results obtained in the continuum of cancer prevention, control and treatment, as they can be responsible for promoting barriers or assist in determining health outcomes(14).
Analyses of an American study evidenced that, in men with prostate cancer, advanced age was strongly related to death cases in shorter periods of time between discovery of the disease and death(15). Lower schooling levels and being "married” had their association with the prevalence of prostate cancer verified in a systematic review of studies about the SDHs in Caribbean countries(16). In the current study, these factors (age, schooling and marital status) were the most frequent characteristics found in the sample. This information on the SDHs and its relationship with cancer shows the importance of paying attention to social differences when designing health care programs and care plans.
In a recent systematic review, mortality was a result of prostate cancer that had its relationship with the SDHs investigated, and only the socioeconomic level showed a relationship with this result, which was possibly justified for being a factor that limited men’s access to the health services and screening policies of the countries involved(16). Factors such as disadvantaged housing conditions, being black-skinned and not being married were associated with the development of more severe cancer cases and mortality among American men(17). These data show the impact of the SDHs on the prostate cancer outcomes and on the dissimilar results of its treatment, in addition to reinforcing the importance of investigating the effects of these determinants on diseases and their outcomes.
In the current study, the sample of prostatectomized men consisted mainly in advanced age people, with low schooling levels, white-skinned, with a history of cancer in the family, with a partner, who stated professing some religion, with a family network (children and not living alone), with low monthly financial resources and access to housing, public transportation, garbage collection and basic sanitation. Somehow, the SDHs in the sample converge with what is presented in the literature with regard to individual factors, social characteristics and support networks related to prostate cancer, previously discussed.
Furthermore, important characteristics of the sample in the current study, such as the existence of support networks, conditions of access to basic services and housing, and being mostly white-skinned, may have been factors responsible for the high self-perception of health and quality of life scores. It is noted that, according to the literature, the social and economic aspects are strongly related to better quality of life levels in the patients after the prostate cancer treatment. Such aspects were responsible for improving attitudes towards the disease, emotional adjustment, coping and stress tolerance(18).
Regarding the relationship between the variables investigated in this study and quality of life, religion, type of surgical approach, marital status, schooling and family history of cancer stand out. Part of these findings find support in the literature, as the investigation of the impact of religion and schooling on quality of life was evidenced in a study with 624 American men subjected to prostatectomy. In view of this, the strength that the proper care of these SDHs produces in the health results after prostatectomy is reinforced(19).
Quality of life after radical prostatectomy is usually assessed using specific instruments that massively comprise the functional results of the surgery or by assessing quality of life resorting to more general instruments. These latter may not be sensitive enough to detect changes in quality of life in a specific way; however, when appreciating functional results, specific measures may not value important Quality of Life aspects that are related to the SDHs(20).
Thus, based on the results obtained in the current study, health self-perception was considered a substantial aspect of Quality of Life and possibly affected by the disease and treatment, in addition to being an indicator of morbidity and reduced functionality(21). In the sample of the current study, 42.2% of the participants had a negative self-perception of their health, that is, their answers varied between Very bad, Bad and Fair. In studies conducted with Brazilian aged individuals, without considering radical prostatectomy, the frequency of negative self-perception of health varied from 6.3% to 54.7%(21,22).
In these studies, the factors related to negative self-perception of health were female gender, unemployment, comorbidities, food insecurity, sedentary lifestyle and black skin color(21),(22); in turn, the factors related to positive self-perception were higher schooling levels, access to health insurance, consumption of vegeTables and fruits and physical activity(22). It is worth mentioning a study that investigated the effect of urinary incontinence in older adults on self-perception of health, as its results evidenced that incontinent individuals were four times more likely to have a negative self-perception of their health(23). No studies were identified that analyzed associations between the “religiousness” and “owning a house” factors.
Among 183 Finnish men subjected to prostatectomy one year ago, 63% of them self-perceived their health as good; the factors related to this result were advanced age, high satisfaction with the prostate cancer treatment and better urinary function(20). It is understood that knowing the factors associated with health self-perception assists in the practice, as they add qualified and comprehensive information on the health status in this context, with a view to expanding care to dimensions that are not only biological; in addition to that, it can contribute to health planning and to the success of interventions carried out by health professionals(21).
The functional results showed no relationship with the variables under study, quality of life and self-perception of health; however, the occurrence and effects of these results after radical prostatectomy are well-documented, especially their effect in relation to quality of life. Although the “erectile dysfunction” and “urinary incontinence” functional results are barely frequent after prostatectomy, a number of studies that analyzed quality of life, emotional well-being and anxiety failed to evidence long-term impairments in Quality of Life(24).
In the current study, both urinary incontinence and sexual dysfunction were present in most of the interviewees, respectively affecting 66.7% and 87.9% of the sample, with 60.6% reporting having negative feelings such as bad mood, despair, anxiety and depression with periodic frequency. In a study carried out in Finland, the authors found similar distributions of these two complications, that is, high, although with higher urinary incontinence rates(20).
Results from other studies evidenced a significant impairment in the performance and sexual function of the men surveyed and presence of urinary symptoms, corroborating the results of the current study. It is common for surgery complications to exert a direct impact on the quality of life of men subjected to prostatectomy, leading to psychological morbidities in this population group, especially when they are affected by urinary dysfunctions and sexual performance and function impairments(25,26).
Urinary function exerts a direct impact on the patients' quality of life, limiting daily and social activities, restricting family contact and leading to embarrassment or discomfort due to the odor of urine and wet clothes, which directly affects the emotional and social aspects of men affected by this condition(27).
The limitations of the current study are related to the limited number of patients, which precludes performing additional statistical analyses to assess the associations between the variables; in addition, the study was carried out in a single Oncology care center that aggregates patients with common sociodemographic characteristics. The implications for future research studies correspond to the development of more comprehensive surveys on the variables that interfered in the reported self-perception of health.
CONCLUSIONS
The study allowed characterizing men subjected to prostatectomy regarding the main social determinants of health and verified that the participants had a satisfactory health self-perception.
Self-perceived health was associated with professing a religion (p=0.004) and with owning a house (p=0.01). The "professing a religion" factor was also associated with the results obtained in the total Quality of Life score (p=0.024), in the Social Relationships (p=0.023) and Environment (p=0.04) domains. The type of surgical approach was associated with the total Quality of Life score (p=0.008), marital status with the Physical domain (p=0.047), having someone in the family with prostate cancer with the Psychological domain (p=0.027), and schooling was associated with the Social Relationships domain (p=0.019).
It is noted that Nursing can work with patients subjected to prostatectomy, providing them with better health outcomes, and it is hoped that this study will encourage reflections by health teams in this regard. It is also important to emphasize the need to leverage the available information resources to improve access and use of health services by these patients.
REFERENCIAS
1. Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. [Internet]. 2021 [acesso em 06 dez 2022]; 71(3):209-249. Disponível em: https://doi.org/10.3322/caac.21660 [ Links ]
2. Morbeck IAP, Gadia R, Chaves NR. Câncer de Prostata. In: Santos M, Corrêa TS, Faria LDBB, Siqueira GSM, Reis PED, Pinheiro RN. Diretrizes Oncológicas 2. - São Paulo: Doctor Press Ed. Científica; 2019. [ Links ]
3. Nam KH, Shim JL, Kim HY. Factors influencing self-esteem after radical prostatectomy in older adult patients. Geriatr. Nurs. [Internet]. 2022 [acesso 09 dez 2022]; 43(1):206-212. Disponível em: https://doi.org/10.1016/j.gerinurse.2021.11.023 [ Links ]
4. WHO. WHOQOL: measuring quality of life. Psychol Med. [Internet]. 1998 [acesso em 06 dez 2022]; 28(3):551-558. Disponível em: https://doi.org/10.1017/s0033291798006667. [ Links ]
5. Lardas M, Liew M, Van Der Bergh RC, De Santis M, Bellmunt J, Van Den Broeck T, et al. Quality of Life Outcomes after Primary Treatment for Clinically Localised Prostate Cancer: A Systematic Review. European Urology. [Internet]. 2017; 72(6):869-885. [ Links ]
6. Agostinho MR, Oliveira MC, Pinto MEB, Balardin GU, Harzheim E. Autopercepção da saúde entre usuários da Atenção Primária em Porto Alegre, RS. Rev Bras Med Fam Comun. [Internet]. 2010 [acesso em 06 dez 2022]; 17(5):9-15. Disponível em: http://dx.doi.org/10.5327/z1809-59092010000500003. [ Links ]
7. Porto DB, Arruda GA, Altimari LR, Cardoso Júnior CG. Autopercepção de saúde em trabalhadores de um Hospital Universitário e sua associação com indicadores de adiposidade, pressão arterial e prática de atividade física. Ciênc. Saúde Coletiva. [Internet]. 2016 [acesso em 06 dez 2022] 21(4):1113-1122. Disponível em http://dx.doi.org/10.1590/1413-81232015214.21682015. [ Links ]
8. Alves LS, Rodrigues RN. Determinantes da autopercepção de saúde entre idosos do Município de S.P, Brasil. Rev Panam Salud Publica. [Internet]. 2005 [acesso em 09 dez 2022] 17(5/6):333-341. Disponível em http://www.scielosp.org/scielo.php?script=sci_arttext&pid=S1020-49892005000500005&lng=pt&nrm=iso&tlng=pt [ Links ]
9. Rocha RS, Pinheiro LP, Oriá MOB, Ximenes LB, Pinheiro AKB, Aquino PS. Determinantes sociais da saúde e qualidade de vida de cuidadores de crianças com câncer. Rev Gaúcha Enferm. [Internet]. 2016 [acesso em 06 dez 2022]; 37(3):1-6. Disponível em: http://dx.doi.org/10.1590/1983-1447.2016.03.57954. [ Links ]
10. Cunha GH, Fiuza MLT, Gir E, Aquino PS, Pinheiro AKB, Galbão MTB. Qualidade de vida de homens com AIDS e o modelo da determinação social da saúde. Rev. Latino-Am. Enfermagem. [Internet]. 2015 [acesso em 06 dez 2022]; 23(2):183-191. Disponível em: http://dx.doi.org/10.1590/0104-1169.0120.2541. [ Links ]
11. Mendes, EV. O cuidado das condições na atenção primária à saúde: O imperativo da consolidação da Estratégia da Saúde da Família. Brasília: Organização Pan-americana de Saúde. [Internet]. 2012 [acesso em 06 dez 2022]. Disponível em: http://bvsms.saude.gov.br/bvs/publicacoes/cuidado_condicoes_atencao_primaria_saude.pdf. [ Links ]
12. Herdman TH, Kamitsuru S. Diagnósticos de Enfermagem da NANDA-I: Definições e Classificações 2018-2020. 11a. ed. Porto Alegre: Artmed, 2018. [ Links ]
13. Fleck MP, Louzada S, Xavier M, Chachamovich E, Vieira G, Santos L, Pinzon V. Aplicação da versão em português do instrumento abreviado de avaliação da qualidade de vida. Rev. Saúde Pública. [Internet]. 2000 [acesso em 06 dez 2022]; 34(2):178-183. Disponível em http://dx.doi.org/10.1590/s0034-89102000000200012. [ Links ]
14. Venkataramany BS, Sutton JM. The Importance of Social Determinants of Health for Cancer Patients in the Era of COVID-19. Cureus. [Internet]. 2022 [acesso em 06 dez 2022]; 14(8):e27993. Disponível em http://doi.org/10.7759/cureus.27993. [ Links ]
15. Cui W, Finkelstein J. Using EHR Data to Identify Social Determinants of Health Affecting Disparities in Cancer Survival. Stud Health Technol Inform. [Internet]. 2022; [acesso em 06 dez 2022]; 6(290):967-971. Disponível em: https://doi.org/10.3233/SHTI220224. [ Links ]
16. Brown CR, Hambleton I, Hercules SM, Unwin N, Murphy MM, Nigel Harris E, Wilks R, MacLeish M, Sullivan L, Sobers-Grannum N; U.S. Caribbean Alliance for Health Disparities Research Group (USCAHDR). Social determinants of prostate cancer in the Caribbean: a systematic review and meta-analysis. BMC Public Health. [Internet]. 2018 [acesso 06 dez 2022]; 18(1):900. Disponível em: https://doi.org/10.1186/s12889-018-5696-y. [ Links ]
17. Press DJ, Shariff-Marco S, Lichtensztajn DY, Lauderdale D, Murphy AB, Inamdar PP, et al. Contributions of Social Factors to Disparities in Prostate Cancer Risk Profiles among Black Men and Non-Hispanic White Men with Prostate Cancer in California. Cancer Epidemiol Biomarkers Prev. 2022; [acesso 06 dez 2022]; 31(2):404-412. Disponível em: https://doi.org/10.1158/1055-9965.EPI-21-0697. [ Links ]
18. Imm KL,Williams F, Housten AJ, Colditz GA, Drake BF, Gilbert KL, Yang L. African American prostate cancer survivorship: Exploring the role of social support in quality of life after radical prostatectomy, Journal of Psychosocial Oncology. [Internet]. 2017 [acesso 06 dez 2022]; 35(4):409-423. Disponível em: https://doi.org/10.1080/07347332.2017.1294641 [ Links ]
19. Bruce MA, Bowie JV, Barge H, Beech BM, LaVeist TA, Howard DL, Thorpe RJ Jr. Religious Coping and Quality of Life Among Black and White Men With Prostate Cancer. Cancer Control. [Internet]. 2020 [acesso 06 dez 2022]; 27(3):1073274820936288. Disponível em: https://doi.org/10.1177/1073274820936288. [ Links ]
20. Talvitie AM, Ojala H, Tammela T, Koivisto AM, Pietilä I. Factors related to self-rated health and life satisfaction one year after radical prostatectomy for localised prostate cancer: a cross-sectional survey. Scand J Caring Sci. [Internet]. 2019 [acesso 06 dez 2022]; 33(3):688-697. Disponível em: https://doi.org/10.1111/scs.12664. [ Links ]
21. Lindemmann IL, Reis NR, Mintem GC, Mendoza-Sassi RA. Autopercepção da saúde entre adultos e idosos usuários da Atenção Básica de Saúde. Ciência & Saúde Coletiva. [Internet]. 2019 [acesso 06 dez 2022]; 24(1): 45-52. Disponível em: https://doi.org/10.1590/1413-81232018241.34932016. [ Links ]
22. Jesus SR, Aguiar HJR. Autopercepção positiva de saúde entre idosos na região Nordeste do Brasil. Braz.J. Health Review. [Internet]. 2021 [acesso 06 dez 2022] 4(5):20025-20041; Disponível em: https://doi.org/10.34119/bjhrv4n5-124. [ Links ]
23. Kessler M, Volz PM, Bender JD, Nunes BP, Machado KP, Saes MO, et al. Efeito da incontinência urinária na autopercepção negativa da saúde e depressão em idosos: uma coorte de base populacional. Ciência & Saúde Coletiva. [Internet]. 2021 [acesso 06 dez 2022]; 27(6):2259-2267. Disponível em: https://doi.org/10.1590/1413-81232022276.10462021. [ Links ]
24. Kord E, Flores JP, Posielski N, Koenig H, Ho O, Porter C. Patient reported outcomes and health related quality of life in localized prostate cancer: A review of current evidence. Urol.Oncol. [Internet]. 2022 [acesso 06 dez 2022]; 40:304-314. Disponível em: https://doi.org/10.1016/j.urolonc.2022.04.008 [ Links ]
25. Izidoro LCR; Soares GB, Vieira TC, Orlandi FS, Polido Júnior A, Oliveira LMAC, Napoleão AA. Qualidade de vida relacionada à saúde e fatores psicossociais após prostatectomia radical. Acta Paul. Enferm. [Internet]. 2019 [acesso 09 dez 2022]; 32(2):169-177. Disponível em: https://doi.org/10.1590/1982-0194201900024. [ Links ]
26. Massa DC. Qualidade de vida relacionada à saúde em pacientes submetidos à prostatectomia. Minas Gerais, Uberaba. Dissertação (Mestrado em Atenção à Saúde) - Programa de Pós-Graduação Stricto Sensu em Atenção à Saúde, Uiversidade Federal do Triângulo Mineiro, 2018. [ Links ]
27. Bernardes MFVG, Chagas SC, Izidoro LCR, Veloso DFM, Chianca TCM, Mata LRFPD. Impact of urinary incontinence on the quality of life of individuals undergoing radical prostatectomy. Rev Lat Am Enfermagem. [Internet]. 2019 [acesso 09 dez 2022]; 10(27):e3131. Disponível em: https://doi.org/10.1590/1518-8345.2757.3131. [ Links ]
Received: December 12, 2022; Accepted: March 05, 2023











 texto en
texto en 


