Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Enfermería Global
versión On-line ISSN 1695-6141
Enferm. glob. vol.22 no.71 Murcia jul. 2023 Epub 13-Nov-2023
https://dx.doi.org/10.6018/eglobal.551471
Originals
Knowledge, risk level and prevalence of hepatitis B and C among commercial mini-bus drivers in Ado-Ekiti, Ekiti State, Nigeria
1PhD in Nursing Science. Professor at the Faculty of Nursing Sciences, Afe Babalola University, PMB 5454, Ado-Ekiti, Ekiti State, Nigeria
2Master in Nursing Science. Faculty of Nursing Sciences, Afe Babalola University, PMB 5454, Ado-Ekiti, Ekiti State, Nigeria
3PhD in Microbiology. Professor at the Department of Biological Sciences, Afe Babalola University, PMB 5454, Ado-Ekiti, Ekiti State, Nigeria
Background:
Hepatitis B and C are potentially life-threatening liver infections and major public health challenge affecting 350 million people with approximately annual deaths of 1.4 million.
Objective:
Determine the knowledge and investigate the prevalence of HBV and HCV among commercial mini-bus drivers in Ado- Ekiti, Ekiti State, Nigeria.
Methodology:
Descriptive, cross-sectional design using quantitative strategy. Multistage sampling technique was used to recruit 110 respondents. An adapted questionnaire from two previous studies was used for participants’ sociodemographic characteristics, knowledge level of Hepatitis B and C, risk factors and vaccination hesitancy while laboratory investigations were used for HBV and HCV prevalence. Descriptive and inferential statistics were used for data analysis.
Results:
Findings revealed that one-third (32.7%) of the respondents were between 39-48 years. Majority (73.6%) were married with 39.1% having at least two sexual partners. Majority (80%) have heard of HBV while 75% have never heard of HCV, 43.6% and 59.1% have poor knowledge level of hepatitis B and C. The prevalence of HBV and anti-HCV among the respondents were 7.3% and 1% respectively. Major risk factors identified were tattooing, multiple sexual partners, and unprotected sex. There was a significant relationship between respondents’ knowledge of hepatitis B and age (X2 =21.39, p=0.006) and number of sexual partners (X2=21.25, p= 0.002) while only educational background (X2=13.58, p= 0.035) was significantly associated with the knowledge level of hepatitis C.
Conclusion:
Hence, purposeful efforts on awareness and prevention programs for HBV and HCV should be made by nurses, other healthcare professionals and all other stakeholders.
Key words: Knowledge; prevalence; hepatitis B and C; hesitancy; risk factors; vaccination
INTRODUCTION
Hepatitis virus are grouped into five main strains, these are type A, B, C, D and E which if not promptly of well managed can result into liver diseases (1),(2). Though, they are different in methods of transmission, severity of illness, geographical distribution as well as the method of prevention and control (1). Hepatitis B and C diseases are potentially life-threatening liver infections and a silent killer that has become a major public health challenge that affect 350 and 170 million people globally and has led to an annual death of 1.4 million (1). Most of the deaths are as a result of untreated chronic hepatitis infections that are related to liver cirrhosis and liver cancer (3).
Hepatitis B and C can often lead to chronic hepatic diseases such as liver cirrhosis, hepatocellular cancer, hepatitis related deaths, psychological and occupational diseases. Hepatitis B and C are responsible for a large proportion of hepatitis morbidity and mortality as more than 90% of infected persons are unaware of their conditions and as such do not bother to seek treatment (4). It is estimated that about 350 and 170 million people worldwide are infected with hepatitis B and C respectively (5). Hepatitis B and C are separate viruses with entirely different life cycles, but co-infection of both is common as a result of their similar route of transmission particularly in countries where both viruses are endemic (6). While HBV affect almost two billion people, the cost of treatment is very expensive for individuals in developing countries and the infection can be very difficult to clear following its progression to chronicity (7).
Globally, there are variations in the knowledge level of hepatitis B virus (HBV) and hepatitis C virus (HCV). Awareness of chronic viral hepatitis in the United State of America remains suboptimal (8). Rajamoorthy et al. (9) reported a relatively low awareness level of hepatitis B among households in Malaysia. Also, low knowledge level of hepatitis B and C was reported by Ayele et al. (10) in Ethiopia. Whereas, a high level of awareness and average knowledge level about hepatitis B was reported by Eni et al. (5) in Abia State Nigeria. According to a study by Kim et al. (8), high level of awareness of HBV infection was noted among individuals with higher education. The Nigerian Ministry of Health developed the National Viral Hepatitis Strategic Plan that spanned from 2016 to 2020, with strategic actions mapped out to place Nigeria on the path of eliminating hepatitis. Conversely, despite the program about 15 million Nigerians are still ignorant of the virus and its mode of transmission thus, encouraging it spread. The reasons for the high prevalence may be due to lack of proper health facilities; poor economic status and less public awareness about the transmission of major communicable diseases (11).
In the United States, an estimated 0.8 -1.4 million people are being chronically infected with HBV, while 2.7 -3.9 are chronically infected with HCV (12). Africa and Western pacific region are the highest endemic regions for HBV with prevalence of 6.1% and 6.2% respectively, although HCV is epidemic in all regions across the globe (13). In Nigeria the prevalence of hepatitis B and C in 2018 is indicated to be 8.1% and 1.1% of the population respectively. This indicates that about 16 million Nigerians have hepatitis B or C whereas about 11% of Nigerian patients with hepatitis B also had hepatitis C. Nigeria with an estimated population of 190 million has about 16 million and 2.2 million people to be living with HBV and HCV, this represents about 8.1% and 1.1% of estimated population respectively (11).
Khan et al., (14), identified various occupations that are at higher risk of contracting HBV and HCV such as health workers, barbers, armed forces, sewage workers and drivers. Some identified risky behaviours that are common among commercial drivers as most long-distance drivers live apart from their families and may practice high level of unsafe sexual activities. Mini-buses are use as commercial means of transport in Nigeria and they are commonly used in the western part of the country. Commercial mini-bus drivers are licensed and under the control and protection of Road Transport Unions (15). In Nigeria, several studies such as Ijeoma et al. (16), Yusuf et al. (17), and Lawal et al. (18) have been conducted on people at high risk of HBV and HCV such as health workers, scavengers, prisoners to mention but a few with little considerations on commercial drivers.
OBJECTIVE
The objective of the study was to assess the knowledge and prevalence of hepatitis B and C among commercial mini-bus drivers in Ado Ekiti.
MATERIAL AND METHODS
Research design and setting
Descriptive and cross-sectional research designs using quantitative strategy was employed in the study. The descriptive research design was considered appropriate because it ascertains the prevailing condition and better description of respondent’s disposition about hepatitis B and C using questionnaire. The cross-sectional design offered the opportunities to get good representatives of the sample for the study and a better generalization can be made possible.
The study was conducted in Ado Ekiti, the state capital of Ekiti State, southwestern Nigeria. Ekiti State is located 92 miles (148km) east of Ibadan. Yoruba, Hausa, Igbo and Egbira are the major inhabitants in Ado Ekiti with projected population at 2016 to be 427,700 (NPCN, 2015). Major occupations include farming, trading, public services, self-employment such as commercial drivers. The study population comprised of all registered commercial mini-bus drivers in Ado-Ekiti metropolis which consists of 259 mini-bus drivers. The study was conducted from December 2021 to February, 2022.
Sample technique and data collection
Sample size was calculated as described by Cochran (19). Using prevalence of 10.7% as reported by Sanni and Amoran (20) and 7.0% by Lawal et al., (18) a total of 110 commercial mini-bus drivers was calculated as sample size for the study, after factoring 10% anticipated non-response.
The multistage sampling technique involving four stages was adopted for this study. In stage one, simple random sampling technique was used to select two out of the four commercial mini buses zones in Ado Ekiti. In stage two, two units each were selected from the two zones using purposive sampling method due to the capacity of the units. The third stage involve the use of simple random sampling technique to select two parks from the four units making a total of eight parks. In the fourth and last stage, convenience sampling method was used to select the first thirteen commercial mini-bus drivers met at each park who met the study inclusion criteria. The inclusion criteria for this study include, being a registered commercial mini-bus drivers in the selected parks; must be licensed and driving a mini bus for at least a year and willingness to participate in the study.
The instruments for data collection for this study a standardized questionnaire adapted from Balegha et al. (21) and Ayele et al. (10). The questionnaire comprised of two parts. Part 1 comprises of 4 sections, A to D, in which Section A consists of 11 questions that centered on participants’ socio demographic characteristics. Section B covers eight variables to assess participants’ knowledge level of hepatitis B and C using 56 questions which elicited ‘yes and no’ responses. Correct response was given 1-mark, total scores was grouped into three categories. Scores less than 50% were classified as poor knowledge, above 50% but less than 70% were moderate knowledge while 70% and above were classified as good knowledge. Section C consists of 13 questions that assessed the risk behaviours among the respondents using four- point rating scale of 1-4 marks. Section D consisted of 9 questions on hepatitis B vaccination hesitancy using five- point Likert scale responses that is graded from 1-5 marks.
Part 2 of the questionnaire consists of laboratory investigations. The collected blood samples were screened for hepatitis B surface antigen (HBsAg) and anti-HCV. The questionnaire was referred to as questionnaire on knowledge, prevalence, risk factors and vaccination hesitancy termed QKPRVH.
For the blood sample collection, aseptic technique was observed and 5mls of venous blood was collected from each participant into a plain specimen bottle after consent was sought and obtained at the motor park. The participant’s code, time, and date of collection were labeled on the bottle for proper identification. Sample collected were transported daily to Ekiti State Teaching Hospital’s laboratory. Each of the samples was centrifuged at 3000 r/min for 5 minutes and the serum portion was used on the test strip for antigen or antibody detection. Sera samples were stored at −25°C in line with the manufacturer’s instruction until screened for HBsAg and anti-HCV antibodies. Screening was conducted using Diastop Rapid Diagnostic Test and reported as positive or negative.
The researcher visited two selected parks in a unit each day at exactly 9am for six days a week to distribute the questionnaire and take the respondents’ blood sample. The questionnaire was made simple and clear as much as possible while the illiterates were given the translated version. They were guided and assisted to fill the questionnaire. Laboratory investigations were carried out. The selected respondents were informed on benefits of the study in Yoruba and English, and reasons for carrying out laboratory investigations were explicitly made known to them. The respondents were motivated for active and full participation. Interested nurses and laboratory technicians in Ekiti State University Teaching Hospital were trained as research assistants.
Data analysis
Descriptive statistics which include frequency and proportions were used summarize of the respondents’ socio demographic characteristics. Mean and standard deviation of respondents’ knowledge and hepatitis B vaccination hesitancy were calculated. Inferential analysis was done using chi-square test to test the significance of the relationship of respondents’ socio-demographic characteristics (age, educational level and number of sexual partners) and their knowledge of hepatitis B and C while logistic regression analysis was used to determine the risk factors’ prediction of HBV and HCV among commercial mini-bus drivers. The probability p≤ 0.05 was taken as the minimum level of significance
Ethical consideration
Approval to conduct the study was obtained from the Ekiti State Ministry of Health with approval number MOH/EKHREC/EA/P/23 which was taken to the headquarters of NURTW in Ekiti State to obtain permission to make use of their members after a proper briefing of the executives. All participants consented and their rights were protected. They were adequately informed of the process, purposes and objectives of the study. The physical, mental, and social well-being of the research respondents were ensured. This study did not cause any psychological/mental or social harm to the respondents and the physical discomfort that occurred when blood samples were being taken was minimized by ensuring that blood samples were taken once and aseptic technique maintained to prevent the risk of infection. Participants’ confidentiality and anonymity were ensured by handling all information carefully during and after data collection.
RESULTS
Socio-demographic profile of the study respondentes
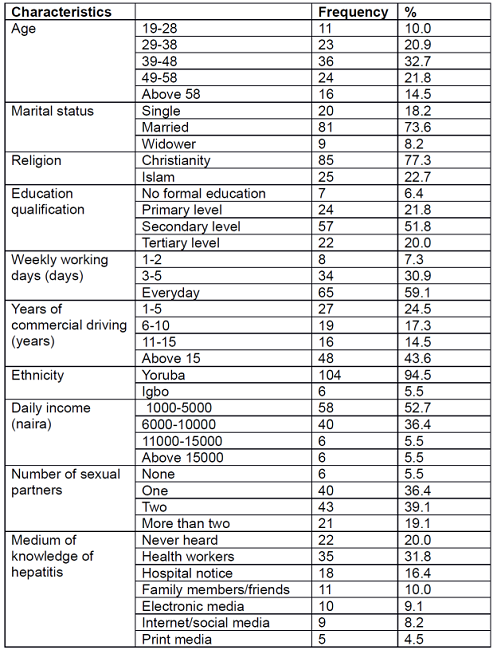
Demographic profile of the study respondents showed that 32.7% of them were within the age range of 39-48 years and 73.6% of them were married. In addition, the majority of them were Christians (77.3%) while 51.8% of them were educated up to secondary school level. Also, 59.1% of them have driven commercially on a daily basis while 43.6% of them have been driving commercially for over 15 years. Furthermore, 39.1% of the them indicated they had at least two sexual partners while 31.8% of them heard about hepatitis through health workers (Table 1).
Respondents’ knowledge of hepatitis B and C
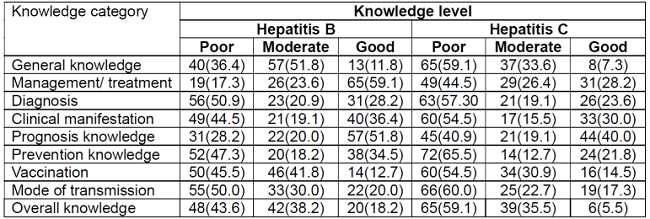
With respect to general knowledge, majority of the study respondents had moderate (51.8%) and poor (59.1) of hepatitis B and C, respectively. In the case management/treatment knowledge level, the majority (59.1%) of them had good knowledge of hepatitis B while only 28.2% for Hepatitis C. The majority of the respondents had poor knowledge level of hepatitis B diagnosis (50.9%), clinical manifestation (44.5%), prevention (47.3%), vaccination (45.5%) and mode of transmission (50%). In the case of hepatitis C, the majority of the respondents had poor knowledge of all the categories of knowledge measured. Generally, overall knowledge of hepatitis was observed to be poor 43.6% and 59.1% of the respondents, for B and C, respectively (Table 2).
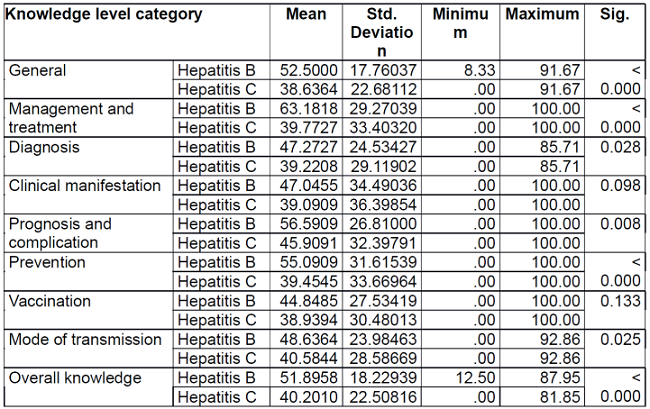
A comparison of the mean scores between the respondents’ knowledge of hepatitis B and C revealed significantly higher knowledge scores for hepatitis B than C (p= 0.001). In all the knowledge categories tested, hepatitis B knowledge among the respondents were significantly higher than that of C. However, knowledge of hepatitis with respect to clinical manifestation and vaccination did not differ significantly between B and C (Table 3).
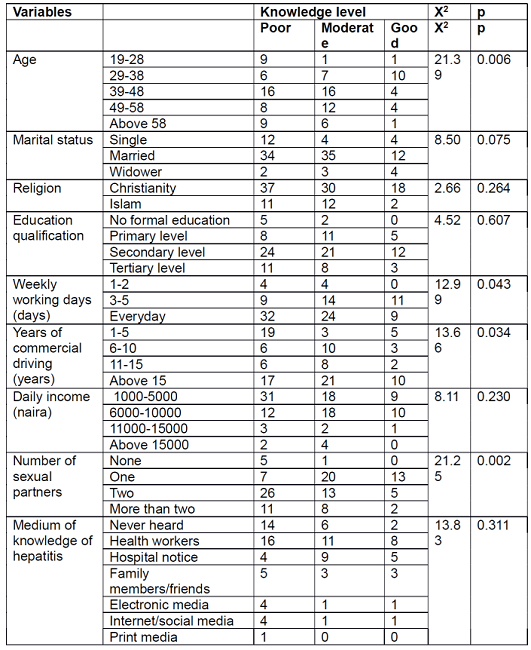
With respect to hepatitis B, respondents’ overall knowledge level was observed to be significantly associated with age (X2= 21.39, p= 0.006, weekly working days (X2= 12.99, p= 0.043, years of commercial driving (X2= 13.66, p= 0.034) and number of sexual partners (X2= 21.25, p= 0.02). In the case of hepatitis C, only educational qualification (X2= 13.58, p = 0.035) and years of commercial driving (X2= 14.44, p= 0.025) were observed to be significantly associated with overall knowledge level (Tables 4 and 5).
Table 4: Relationship of demographic characteristics of the respondent with knowledge level of hepatitis B.
Hepatitis B and C prevalence, risk factors and vaccination hesitancy
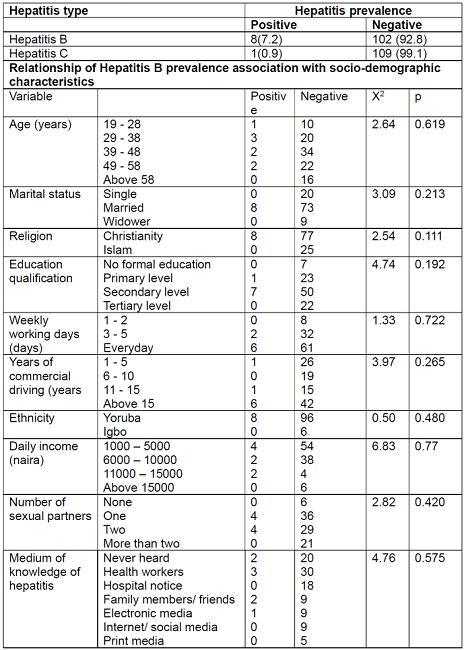
Hepatitis B and C prevalence among the study respondents revealed 7.2 % and 0.9% positive cases, respectively. For hepatitis B, none of the respondents’ socio-demographic characteristics was observed to be significantly associated with prevalence (Table 6).
The respondents’ risk of contracting hepatitis B or C based on their risk behaviours revealed that none was at high risk. The majority (70.9%) of them were observed to be at low risk while 29.1% were at moderate risk with none of them at high risk.
Religion (X2= 11.36, p= 0.001), educational level (X2= 13.90, p= 0.003), daily income (X2= 8.94, p= 0.030), number of sexual partners (X2= 20.62, p= < 0.001) and medium of knowledge of hepatitis (X2= 20.99, p= 0.002) were significantly associated with respondents’ risk of contracting hepatitis (Table 7).
Table 7: Relationship of demographic characteristics of respondent with risk level of hepatitis B and C.

In the case of hepatitis vaccination hesitancy, 30.9% of them showed low hesitancy and 54.5% and 14.5% of them showed moderate and high hesitancy, respectively. Of all the respondents’ socio-demographic characteristics, only medium of knowledge of hepatitis (X2= 30.48, p= 0.002) was observed to be significantly associated with hesitancy level to vaccination (Table 8).
DISCUSSION
One-third of the respondents were within 39-48 years old, about half attained secondary school education and more than half drive on daily basis with over 15 years’ experience as commercial drivers. Also, more than one-third have at least two sexual partners and have heard about hepatitis through health workers. These characteristics were similar to the findings of studies conducted by Ayele et al. (10).
The overall knowledge level of the study participants was poor with 43.6% and 59.1% for both hepatitis B and C respectively. Poor knowledge level was observed to be more with hepatitis C as greater number of participants had no prior knowledge of it. This finding is similar to the findings of Freeland et al. ((22) where most participants showed low knowledge level of hepatitis B. This is also in agreement with another study conducted by Dehghani et al. ((23) where 95% and 26.6% of the respondents have not heard of hepatitis B and C.
The prevalence of hepatitis B and C in the study was 7.3% and 1.0% which is within the range of 2-7% (intermediate prevalence) and 0-<2.0 (low prevalence) (CDC, 2020). The possible reasons for intermediate prevalence in this study might be due to poor knowledge of mode of transmission and prevention of hepatitis B and C, having multiple sexual partners and majority of the participants were not vaccinated. The prevalence of hepatitis B and C among the study participants is similar to the studies of Ayele et al. (10) with 7.3% prevalence rate, 8.4% by Khan et al. (14). Although, the study findings are slightly higher than the 6.3% and 6.5% reported by Lingani et al. (24). Also, 5.9% prevalence rate was also reported by Gibney et al. (25). However, a similar study conducted by Nkup et al. (15) in Jos, Plateau State Nigeria recorded a higher rate of 16.8%. while another study conducted in Ekiti State, Nigeria, the same setting with the current study a decade ago but among adolescent recorded 11.5% (26).
The prevalence of hepatitis C among commercial mini-bus drivers in Ado Ekiti as obtained in the study was 1.0%. Similar studies by Ayele et al. (10) and Lingani et al. (24) also obtained low prevalence of 2.0 and 2.1% respectively. Another similar study conducted by Freitas et al. ((27) among long - distance truck drivers obtained a prevalence rate of 1.4%. The difference observed in the prevalence rates could be connected to the knowledge level of the study population, their geographical locations as well as the method of hepatitis screening such as rapid test that was used in this study.
The identified risk factors of hepatitis B and C among respondents were tattooing (22), multiple sexual partners and unprotected sexual intercourse. The identified risk factors were similar to the findings of Lawal et al. (18), where scarification/ tattoo and sexual exposure were identified as risk factors for hepatitis B and C. Also, previous studies by Nkup et al. (15) and Fretaitas et al. (27) reported unprotected sex with multiple sexual partners including commercial sex workers and sharing of personal items as risk factors of hepatitis B and C. da Motta et al., (28) also mentioned inconsistent condom use as a risk factor. Multiple sexual partners were one of the risk factors confirmed in the study.
Majority of the respondents had not been vaccinated against hepatitis B. Major factors for hepatitis B vaccination were; ‘precautionary measures such as hand washing and good sanitation are enough to protect someone from being infected. Medium of knowledge of hepatitis and educational qualification were the predictors of vaccination hesitancy. Identified factors for vaccination hesitancy by Guzman-Holst et al. (29) include participants’ low level of education and lack of awareness of disease which served as obstacle to vaccination acceptance were similar to the findings of this study. There is link between participants’ level of education as well as their employment status which can influence their knowledge about vaccinations, encourage information seeking and sharing among the colleagues and this might consequently change their perceptions about the vaccination.
The test of hypothesis showed that there was a significant relationship between respondents’ social-demographic factor (age, number of sexual partners) and knowledge level of hepatitis B. The younger respondents between the age 29-38 years have a greater percentage of good knowledge of hepatitis B and this might be due to their level of education as majority attained at least secondary level of education where they could have heard of hepatitis B. Also, there was increase in knowledge of hepatitis B among those that have one sexual partner. The increase in their knowledge level might affect their actions positively. However, there was no significant relationship between participants ‘educational level and their knowledge of hepatitis B. This finding was at variance with previous studies by Gebrecherkos et al. ((30) where educational level was significantly related to the knowledge level of hepatitis B. Also, the relationship between age and knowledge level was at variance with the study of Eni et al. ((5) where no difference was observed in knowledge across the age groups
Limitations
The limitation of the study was the convenience sampling of the participants and the use of a smaller sample may serve as limitations thus, the findings may not be generalised to other areas.
CONCLUSION
The study assessed the knowledge level, investigate the prevalence, and determine the risk factors of hepatitis (B and C) and vaccination hesitancy among commercial mini-bus drivers in Ado Ekiti. Poor knowledge of hepatitis B and C was observed with low prevalence and vaccination among the study participants. Multiple sex partners and tattooing were the major risk factors that significantly predicted prevalence of hepatitis B. The study concluded that the prevalence of HBsAg is intermediate and that of anti-HCV is low, multiple sex partners and tattoo were the predictors of HBV and none predicted HCV among the studied population.
It is believed that the study has sensitized and provided relevant information to the study participants on hepatitis B and C and how it can be prevented and effectively managed if diagnosed. It is believed that participation in the study has improved participants’ sense of risk, knowledge as well as their health seeking behaviours and consequently may encourage positive lifestyles that may reduce future infections.
REFERENCES
1. Jefferies M., Rauff B., Rashid H., Lam T., Rafiq S. Update on global epidemiology of viral hepatitis and preventive strategies. World J. Clin. Cases, 2018, 6(13), 589. [ Links ]
2. Li T., Su S., Zhao Y., Deng R., Fan M., Wang R., Sharma M., Zeng H. Barriers to the prevention and control of hepatitis B and hepatitis C in the community of southwestern China: qualitative research. Int. J. Environ. Res. Public Health, 2019, Health, 16(2), 231. [ Links ]
3. Mustapha G.U., Ibrahim A., Balogun M.S., Umeokonkwo C.D., Mamman A.I. Seroprevalence of hepatitis B virus among antenatal clinic attendees in Gamawa Local Government Area, Bauchi State, Nigeria. BMC Infect. Dis., 2020, 20(1), 1-6. [ Links ]
4. Ochei K.C., Obeagu E.I., Ibegi B.T., Ugobo E.I., Odu M.. Prevalence of hepatitis B and C from samples received from the various wards in Niger Delta University Teaching Hospital (NDUTH), Okolobiri for Hematological analyses. Merit Res. J., 2016, 4(4), 204-209. [ Links ]
5. Eni A.O., Soluade M.G., Oshamika O.O., Efekemo O.P., Igwe T.T., Onile-Ere O.A.. Knowledge and awareness of hepatitis b virus infection in Nigeria. Ann. Glob. Health, 2019, 85(1). [ Links ]
6. Muhamad N.A., Abdul M.H., Muhammad E.N., Mohamad H., Mohd R., Abdullah N., Muhammad N.A., Abd N., Ismail N., Mhd Yusuf N.A., Othman R. Seroprevalence of hepatitis B virus and hepatitis C virus infection among Malaysian population. Sci. Rep., 2020, 10(1), 1-11. [ Links ]
7. Madihi S., Syed H., Lazar F., Zyad A., Benani A. A systematic review of the current hepatitis B viral infection and hepatocellular carcinoma situation in Mediterranean countries. Biomed. Res. Int., 2020: 7027169. [ Links ]
8. Kin K.C., Lin B., Chaung K.T., Ha N.B., Trinh H.N., Garcia R.T., Nguyen H.A., Nguyen K.K., Levitt B.S., Da Silveira E.B., Nguyen M.H. Less-established risk factors are common in Asian Americans with hepatitis C virus: a case-controlled study. Dig. Dis. Sci., 2013, 58(11), 3342-3347. [ Links ]
9. Rajamoorthy Y., Taib N.M., Munusamy S., Anwar S., Wagner A.L., Mudatsir M., Müller R., Kuch U., Groneberg D.A., Harapan H., Khin A.A. Knowledge and awareness of hepatitis B among households in Malaysia: a community-based cross-sectional survey. BMC Public Health, 2019, 19(1):.1-11. [ Links ]
10. Ayele A., Abera D., Hailu M., Birhanu M., Desta K. Prevalence and associated risk factors for Hepatitis B and C viruses among refugees in Gambella, Ethiopia. BMC Public Health, 2020, 20(1), 1-10. [ Links ]
11. Ekpenyong M., Tawari-ikeh P., Ekpenyong A. Investigation on the awareness of hepatitis B virus among health care workers in Nigeria. Nurs. Palliat. Care, 2016, 1(5), 124-129. [ Links ]
12. Centers for Disease Control and Prevention (CDC). (2012). Updated CDC recommendations for the management of hepatitis B virus-infected health-care providers and students. MMWR. Morbidity and Mortality Weekly Report., 2012, 61(RR-3):1-2. [ Links ]
13. Lakoh S., García-Tardón N., Adekanmbi O., van der Valk M., Smith S.J., Grobusch M.P. Prevalence of viral hepatitis B and C in Sierra Leone-current knowledge and knowledge gaps: a narrative review. Trans. R. Soc. Trop. Med. Hyg., 2021, 115(10): 1106-1113. [ Links ]
14. Khan A., Afzal S., Yaqoob A., Fatima R., Haq M.U., Junaid K., Nadir A. Epidemiology of viral hepatitis B and C in Punjab, Pakistan: a multicenter cross-sectional study, 2017-18. F1000Research, 2019, 8(2065), 2065. [ Links ]
15. Nkup J.Y., Ocheme J., Jesinta S., Samirah D., Nanya C., Innocent O., Anejo-Okopi J. Seroprevalence of Hepatitis B surface antigen (HBsAg) and hepatitis B antibodies among commercial motor park workers in Jos North, Nigeria. Saudi J. Pathol. Microbiol., 2019, 4(3), 240-244. [ Links ]
16. Nwokediuko S.C., Ijeoma U. Seroprevalence of antibody to HDV in Nigerians with hepatitis B virus-related liver diseases. Niger. J. Clin. Pract., 2009, 12(4). [ Links ]
17. Yusuf R.O., Sawyerr H.O., Adeolu A.T., Habeeb L.M., Abolayo T.T. Seroprevalence of Hepatitis B virus and compliance to standard safety precautions among scavengers in Ilorin Metropolis, Kwara State, Nigeria. J. Health Pollut., 2018, 8(19). [ Links ]
18. Lawal M.A., Adeniyi O.F., Akintan P.E., Salako A.O., Omotosho O.S., Temiye E.O. Prevalence of and risk factors for hepatitis B and C viral co-infections in HIV infected children in Lagos, Nigeria. PLOS One, 2020, 15(12), p.e0243656. [ Links ]
19. Cochran W.G. Sampling Techniques, 2nd ed., New York: John Wiley and Sons, Inc, 1963. [ Links ]
20. Sanni T.A., Amoran O.E. Prevalence and risky health behaviours associated with hepatitis B and C infection among blood donors in Ogun State, Southwest, Nigeria. Texila Int. J. Clin. Res., 2019, 003, 1-8. [ Links ]
21. Balegha A.N., Yidana A., Abiiro G.A. (2021). Knowledge, attitude and practice of hepatitis B infection prevention among nursing students in the Upper West Region of Ghana: A cross-sectional study. PLOS One, 2021, 16(10), p.e0258757. [ Links ]
22. Freeland C. Bodor S. Perera U. and Cohen C. (2020). Barriers to hepatitis b screening and prevention for african immigrant populations in the United States: A qualitative study. Viruses, 12(3): 305. [ Links ]
23. Dehghani B., Dehghani A., Sarvari J. (2020). Knowledge and awareness regarding hepatitis B, hepatitis C, and human immunodeficiency viruses among college students: A report from Iran. Int. Q. Community Health Educ., 2020, 41(1): 15-23. [ Links ]
24. Lingani M., Akita T., Ouoba S., Nagashima S., Boua P.R., Takahashi K., Kam B., Sugiyama A., Nikiema T., Yamamoto C., Somé A. The changing epidemiology of hepatitis B and C infections in Nanoro, rural Burkina Faso: a random sampling survey. BMC Infect. Dis., 2020, 20(1), 1-14. [ Links ]
25. Gibney L., Saquib N., Metzger J., Choudhury P., Siddiqui M.A., Hassan M.S.. Human immunodeficiency virus, hepatitis B, C and D in Bangladesh's trucking industry: prevalzx ence and risk factors. Int. J. Epidemiol., 2001, 30(4), 878-884. [ Links ]
26. David O.M., Oluduro A.O., Ariyo A.B., Ayeni D., Famurewa O. Sero-epidemiological survey of hepatitis B surface antigenemia in children and adolescents in Ekiti State, Nigeria. J. Public Health Epidemiol., 2012, 5(1), 11-14. [ Links ]
27. Freitas N.R., Teles S.A., Matos M.A., Lopes C.L., Reis N.R., Espírito-Santo M.P., Lampe E., Martins R. (2010). Hepatitis C virus infection in Brazilian long-distance truck drivers. Virol. J., 2010, 7(1): 1-6. [ Links ]
28. da Motta L.R., Sperhacke R.D., de Gregori Adami A., Kato S.K., Vanni A.C., Paganella M.P., de Oliveira M.C.P., Giozza S.P., da Cunha A.R.C., Pereira G.F.M., Benzaken A.S.. Syphilis prevalence and risk factors among young men presenting to the Brazilian Army in 2016: results from a national survey. Medicine, 2018, 97(47). [ Links ]
29. Guzman-Holst A., DeAntonio R., Prado-Cohrs D., Juliao P. Barriers to vaccination in Latin America: A systematic literature review. Vaccine, 2020, 38(3), 470-481. [ Links ]
30. Gebremeskel T., Beshah T., Tesfaye M., Beletew B., Mengesha A., Getie A. Assessment of knowledge and practice on hepatitis B infection prevention and associated factors among health science students in Woldia University, Northeast Ethiopia. Adv. Prev. Med., 2020, 9421964. [ Links ]
Received: December 15, 2022; Accepted: March 27, 2023











 texto en
texto en