Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Enfermería Global
versión On-line ISSN 1695-6141
Enferm. glob. vol.22 no.71 Murcia jul. 2023 Epub 13-Nov-2023
https://dx.doi.org/10.6018/eglobal.554661
Reviews
Bioethical perspective of the limitation of therapeutic effort in adult terminal patients. Systematic review
1Primary Care Nurse of Mallorca. PhD student in Applied Clinical Bioethics from the University of Murcia. Professor at the Faculty of Nursing at the University of the Balearic Islands (Mallorca). Spain
2PhD from the University of Murcia. UMU academic associate professor
Nurse in Resuscitation, anesthesia and pain therapy, Hospital General Universitario Reina Sofía in Murcia. Murcia. Spain
3PhD in Philosophy from the University of Murcia. Associate Professor at the Faculty of Philosophy at the University of Murcia
Doctor of the Murcian Health Service. Murcia. Spain
Introduction:
Faced with the ability to maintenance vital functions artificially, new ethical concerns arise among health professionals regarding death. It is been questioned from ethics if the care team should always do everything necessary and possible to prevent the death of a patient.
Objective:
to analyze the bioethical aspects of limiting therapeutic effort in end-of-life patients, encourage reflection and contribute to improving end-of-life care.
Method:
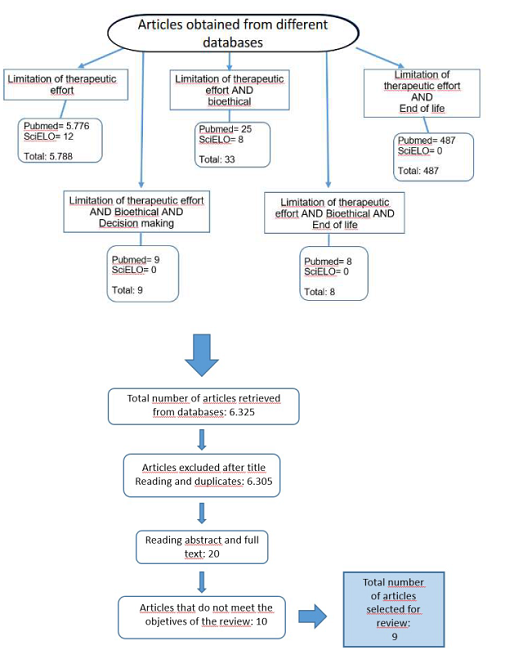
a narrative and integrative review of the scientific literature was performed by searching for publications in meta-search engines and databases of PubMed, SciELO and the journal of Nursing Ethics. A total of 6,325 studies published since 2018 were identified and a total of 9 articles were included.
Results/Discussion:
Issues presented by professionals regarding making-decisions at the end of life, the need to improve training in ethics and aspects related to patients in their last days, palliative care and the limitation of therapeutic effort are described. Only a minority of studies are focused on nursing.
Conclusions:
professional's decisions are influenced by values, emotions, beliefs and experiences, which, together with the difficulty that sometimes exists to establish an accurate clinical diagnosis, makes it difficult to limit therapeutic effort. It is therefore necessary to improve training in ethics and knowledge about end-of-life processes from professionals.
Key words: end of life; limitation of therapeutic effort; bioethical; palliative care; decision making; terminal patient
INTRODUCTION
Faced the ability to maintain vital functions artificially, new ethical concerns arise in healthcare professionals in relation to death. It is been questioned that the task of the care team should always do everything necessary and possible to prevent and postpone the death of a patient(1).
It is in these situations that the so-called Limitation of Therapeutic Effort (hereinafter LTE) arises, defined as the decision to withdraw or not to initiate therapeutic measures (including life support treatments) considered futile in the patient's specific situation, i.e., they are futile since all they do is maintain biological life without any possibility of improvement or functional recovery of the patient with a minimum quality of life. From an ethical and deontological point of view, LTE is a correct action, prevailing the principle of non-maleficence in healthcare, being considered as a good clinical practice(2) (3) (4) (5).
Although decisions to adjust therapeutic effort are frequent and ethically accepted as good clinical practice, there is no clearly defined consensus detailing how such decisions should be carried out at the professional and individual level(4) (5) (6). Research conducted in Latin America (Chile, Colombia and Cuba)(7),(8) shows a lack of familiarity and disagreement on the subject, its concepts and practice(7).
The study by García Caballero et al.(9) based on finding out whether Spanish internists were familiar with LTE and whether their training in palliative care conditioned their knowledge, yielded results in which only 25% of internists were familiar with the definition of LTE(9). There are few studies on the types of conflicts that clinicians encounter most frequently and those that generate most concern. However, the study by Blanco Portillo et al.(10) reveals that end-of-life management, management of the incompetent patient and those arising from the clinical relationship are the most frequent ethical conflicts, making it essential and a priority to design training programs that allow these problems to be addressed and better understood(10).
The introduction of the language of human rights has made it possible to emphasise respect for human dignity also in end-of-life processes. It is therefore fundamental to understand dignified death as a continuation of a dignified life. The concept of human dignity is based on the idea that every human being, by the fact of being born, has the right, among others, to freedom and this is what confers dignity. It is precisely on this innate right that respect for patient autonomy is based, which, together with others, forms the framework for decision-making in complex situations such as not initiating/withdrawing life-sustaining treatment(5),(6).
However, there is a medical, philosophical, anthropological, sociological and political debate surrounding the end of life that makes clinical work difficult. A number of difficulties then arise when it comes to establishing criteria for LTE because the factors taken into account are not exclusively clinical. If in clinical practice it is difficult to achieve certainty, in clinical ethics, where there are conflicts between values, it is even more complex. For this reason, the criteria for making decisions on the limitation fof life-sustaining treatment at the end of life must be rational and cannot be set by a clinician at his or her discretion. The proposal must have been carefully evaluated and well argued.(5) We must understand that the limitation of therapeutic effort is not comparable to euthanasia, to the omission of the duty to assist, to the abandonment of the health service or to the denial of assistance(11.
The emergence and academic rise of bioethics allows and facilitates reflection on the importance of considering science and medical practice in their moral and evaluative aspects. Thus, the responsibility of professionals will increase at the same time as scientific knowledge and technological power increase(1). There is a moral obligation to protect and preserve life, but life is not an absolute value; it has never been considered the fundamental or most important value; often other values of a religious, social, family, etc. type prevail over it, and in the event of conflict with other values in clinical care, these may prevail over the duration of a person's life(12).
In relation to the role of the nurse and her role as the patient's advocate (nurse advocacy) in possible situations of therapeutic obstinacy, it is really important. It has the function of acting by undertaking actions that seek consensus and acceptance of the parties involved in the process regarding the need to adapt and redirect care towards palliative care once the poor response to treatment and the progressive deterioration of the patient has been perceived. In order to act as advocates, reflection, training in ethics and end-of-life processes, and personal analysis are essential to avoid influencing decisions as much as possible. It is therefore considered essential to know the patient, to know the disease and its course, to have training in ethics and palliative care, to have information from the parties involved and to make use of clinical practice guidelines.(13),(14) However, according to the study by Yáñez-Dabdoub et al.(14) and Velarde-García et al.(15) nurses report that decisions are made exclusively by physicians and the patient's relatives and they do not feel included in the decision making about LTE, which causes discontent in the profession as they are one of the professionals who spend most time with the patient(14),(15).
METHOD
Search procedure
A narrative and integrative review of the sources was carried out to describe and show the recent state of research in this particular area. To identify the articles included in the review, the following databases were consulted: SciELO, PubMED and the journal Nursing ethics. The following descriptors were used: end of life, limitation of therapeutic effort, bioethics, decision-making, terminally ill, ethical dilemmas.
Inclusion and exclusion criteria
Articles describing and evaluating healthcare professionals' perceptions on the adequacy of therapeutic effort in different patients at the end of life were considered of interest. We included articles that met the following criteria: available in Spanish and/or English, published in academic scientific journals and whose publication was after 2018. Articles with quantitative design studies, qualitative studies, systematic reviews were selected. Epidemiology articles, those focused on paediatric patients and those dealing directly with euthanasia were excluded. Regarding the format of the articles, articles presenting only abstracts, letters, editorials, reviews, accounts of experiences, theses and monographs were excluded for the review.
Data extraction and analysis
The literature review was conducted from November 2022 to December 2022 in meta-search engines such as SciELO (Scientific Electronic Library Online), in the PubMED open access and specialised health sciences database. To complete the search, the journal Nursing ethics was consulted in order to cover a bioethical point of view of the subject. The search was carried out using the descriptor "limitation of therapeutic effort" as a strategy, but duplicate articles were obtained.
We searched for studies dealing with bioethical aspects related to the end of life and the adequacy of therapeutic effort, as well as the dilemmas faced by professionals in their daily clinical practice. The descriptors used were: "palliative care", "end of life care", "decision making", "limitation of therapeutic effort", "bioethical", "end of life". For the combination of descriptors, the following strategy was developed with the Boolean operator "AND": limitation of therapeutic effort AND bioethical; limitation of therapeutic effort AND end of life; limitation of therapeutic effort AND bioethical AND decision making; limitation of therapeutic effort AND bioethical AND end of life.
In a first reading phase, studies were selected that included the subject of the review in their title and abstract. For the reaing of these abstracts, a strategy of ordering and degree of concordance of the articles in relation to the reviewed topic was elaborated. The process of study identification, selection and inclusion was carried out in several phases. Of the 6,325 articles found and after eliminating the studies that were duplicated and had a low degree of concordance with the review topic, 20 articles were selected for analysis. The title and abstract of the selected articles were read and a total of 3 were excluded because they did not address the subject of the review with sufficient specificity. Subsequently, an exhaustive reading of each of the remaining 17 articles was carried out.
Subsequently, in order to obtain a bioethical perspective, the journal Nursing ethics was consulted. A search was made for articles less than 5 years old and using the descriptor "limitation of therapeutic effort" with 102 results. After reading the title, 13 studies were selected, 3 of which coincided with this review and its objectives. However, it was observed that duplicates were found with the searches performed in the aforementioned databases. Ultimately, then, 9 articles were included for the review as they were the ones that most closely matched the objectives of this review.
A summary graph of the selection of articles from the databases used is shown below:
RESULTS
In the last five years, a large number of studies were found that dealing with aspects concerning the limitation or adequacy of therapeutic effort (n= 6,325). Of this total, after the filtering, reading and exhaustive analysis phases, onlya total of 9 studies were selected as relevant for this review. The main reasons for the exclusion of the studies were: a) they did not deal with the limitation or adequacy of therapeutic effort from the perspective of the health professional, b) there was no description of a bioethical approach to the study, c) it dealt directly and implicitly with euthanasia, d) it was not focused on adult patients at the end of their lives, d) the publications did not meet the inclusion criteria.
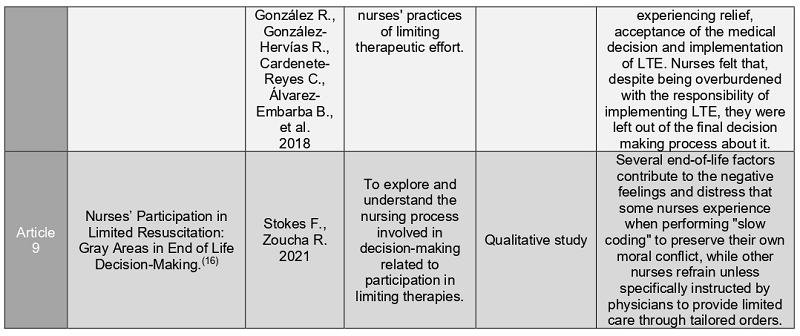
Due to the characteristics of the selected studies, 3 articles are qualitative studies of a phenomenological and evaluative type: Bárzaga Morell et al.(8), Velarde-García et al.(15), Sokes et al.(16);3 others are cross-sectional descriptive quantitative studies aimed at health professionals: Vallejo LI et al. (7), Blanco Portillo et al.(10) and García Caballero et al.(9); 1 literature review: Yáñez-Dabdoub et al.(14); 1 topical article: Alcaraz Brítez, A.G(11); and 1 short communication: Mansilla-Olivares et al.(5) The aforementioned studies come from several countries such as: Mexico (n=1), Colombia (n=1), Paraguay (n=1), Madrid (n=3), Cuba (n=1), USA (n=1), Chile (n=1).
The literature review focused on the search for articles in which, from a bioethical point of view, the ethical dilemmas and difficulties encountered by healthcare professionals in their daily clinical practice in making decisions related to the end of life and the appropriateness of the therapeutic effort could be observed. Only 2 of the selected articles evaluate and integrate the nursing profession in this type of study.
In the literature review by Yáñez-Dabdoub et al.(14), 23 articles were selected where nursing involvement in LTE decision making in the ICU was analysed and discussed, as well as the recognition of the importance of nurses' involvement in LTE decision making. A 2015 study in Turkey showed that 55.6% of nurses refer not to be consulted at the time of LTE decision making, and 75% of nurses were not directly involved in end-of-life care with indication for LTE in ICU. The results of the review show the importance of nursing and its role in the care of patients with LTE, to ensure that their dignity is preserved at all times and to maintain an integrated approach to the patient. Mention is made of the lack of inclusion of the nursing professional in LTE decision making, either because the physician does not consider other professionals in this process or because the nursing profession believes that it is not part of their competencies. The authors, from the results, affirm that there are a series of obstacles (such as the scarce participation in LTE decision-making of nurses, the scarce training in ethics of health professionals, the lack of institutional support and the biomedical conception of care that propitiates the dehumanisation of care for patients with LTE). The authors conclude on the need to reinforce the theoretical knowledge of future nursing professionals in bioethical aspects associated with clinical practice as well as a restructuring of the ICU services so that there is more space for the family to meet with the patient and the health professional(14).
In the article by Adriana Guadalupe Alcaraz Brítez(11), a descriptive literature search is carried out on the concept of dysthanasia, understood as the prolongation of a patient's dying process by disproportionate means, on bioethical approaches and possible solutions such as learning about bioethics, palliative medicine and improving communication between doctor and patient. The author describes that the population of Paraguay has a high level of misinformation that causes obstacles in the area of doctor-patient communication. The author emphasises that the definition of palliative care should be implemented for those patients who do not respond to treatment and prioritise pain control and symptom relief. She suggests an improvement in the medical school's approach to "giving bad news", improving ethical training and educating patients and their families about pathologies to facilitate decision-making. He concludes that ethical and humanistic training of the health care team is essential, as well as understanding that LTE is not equivalent to euthanasia, omission of the duty to assist, refusal of assistance or abandonment of the health care service(11).
The article by Mansilla-Olivares et al.(5) analyses the position of the National Academy of Medicine of Mexico on end of life decisions including LTE, refusal of treatment, advance directives and palliative sedation. It describes the great confusion generated by the use of incorrect or confusing terms with ideological origins, making it important for professionals to be able to manage a common language through clear and fluent communication. The authors argue that the informed consent process is the product of a healthy patient-physician relationship and not just a mere legal formality. They conclude with the importance of clearly managing the following concepts: a) refusal of treatment, b) therapeutic futility, c) Limitation of Therapeutic Effort, d) advance directives, e) palliative care and f) palliative sedation. The National Academy of Medicine of Mexico concludes with its position on the ethical right of health care to promote a peaceful death, that medical care at the end-of-life requires a special strengthening of the patient-physician relationship, on the existence of medical actions and concepts at the end of life that are inherent to the daily work and rise the duty of the Academy to promote an open and honest discourse on end of life decisions and medically assisted termination of life.
Three quantitative cross-sectional descriptive studies were also selected. The study by Vallejo LI et al.(7) analysed the LTE knowledge of healthcare personnel in Medellín through a descriptive cross-sectional study with non-probabilistic sampling for oncology patients. The total sample consisted of 23 professionals (nursing, medicine, nursing assistants and pharmaceutical chemists). The results of the study show that 95.5% were believers in some religion, 52.2% reported having more than 5 years of work experience and 69.5% reported having more than 5 years of experience with oncology patients. Regarding the term LTE, 56.5% said reported knowing it (4 nursing assistants, 3 subspecialist doctors, 2 pharmaceutical chemists and 1 nurse reported that they did not know it). Of those who said they knew the term LTE, 61.5% defined it correctly. In relation to the therapeutic measures to be implemented in clinically unrecoverable patients, 76.9% considered the hygiene of the patient, 76.9% agreed with postural changes, 92.3% considered analgesia and 84.6% responded positively to sedation. Mechanical ventilation in this type of patient was rejected by 92.3%. The study further describes that only 30% reported difficulties in making decisions to limit therapeutic effort. The measures that should always be performed in a medically unrecoverable patient were analgesia and supplemental oxygen. The authors conclude that LTE is a subject of great controversy from a bioethical, religious and legal point of view due to the lack of clinical practice guidelines and literature that goes beyond the critically ill patient(7).
The study by Blanco Portillo et al.(10) a cross-sectional observational study using a survey distributed by the platform of the Spanish Society of Internal Medicine, aims to describe the most frequent ethical conflicts encountered by Spanish internists and the importance attributed to each of the conflicts. The total sample was 261 participants and evaluated several aspects such as the frequency with which internists identified ethical conflicts and the relevance for their clinical practice. They asked about 19 types of ethical conflicts adapted to the country and its legislation and used Likert scales with scores from 1 to 4 to explore whether ethical problems were frequent and the degree of difficulty they generated. The authors concluded that 70.1% of the respondents encountered ethical conflicts and their clinical practice frequently and 29.9% rarely. A total of 60.1% reported that conflicts rarely made their clinical practice difficult, while 39.9% reported that they made it difficult frequently. The ethical conflicts most frequently encountered by internists in Spain and those considered most relevant are, in order of frequency: the order not to perform CPR, LTE, palliative treatment, those related to physician-patient communication and conflicts with family members. The authors conclude that the most frequent ethical problems for Spanish internists are those related to the end of life, conflicts within clinical relationships and decision-making with incompetent patients, which are similar to the results obtained in other Anglo-Saxon countries and on the European continent. In the American and Croatian studies described in this article, it can be seen that ethical problems related to the end of life were also the most frequent, while in a European multicentre study they ranked third. They therefore conclude that, in view of the similarities between their results and those previously published, it does not seem that the different Mediterranean ethical tradition influences the way ethical problems are perceived in clinical practice. The authors mention a recent study by the SEMI Bioethics Working Group which shows that, despite the fact that most internists consider that conflicts around LTE are frequent, only a minority are familiar with the term and often use this term in a general and unspecific way(10).
García Caballero et al.(9) in their study aimed to find out whether internists knew what LTE was and whether training in palliative care conditioned this knowledge. They conducted a survey of Spanish internists, obtaining a total sample of 273 surveys. More than half had 11 or more years of work experience and most of them worked in public centres. The results of the study described that 85% identified LTE as not initiating active treatment, 65.9% identified it as withdrawal of active treatment and 53.1% with not performing CPR, 21.2% with palliative sedation and 0.4% with euthanasia. None considered that LTE entailed abandonment of the patient. A total of 23.8% indicated the 3 correct options in the definition of LTE, compared with 76.2% who chose only one or two of the correct options. 43% lacked training in palliative care and 68.5% considered the training of internists in this field to be very good or good. 62.3% were anxious or uncomforTable with end-of-life care planning and 81.3% felt that they had some conflict with their LTE decisions. 98.9% felt that these difficulties could be alleviated by increasing training in palliative care. The authors conclude that, although LTE decisions are part of the daily work of Spanish internists, only 1 in 4 is able to properly identify the assumptions that make up LTE. Furthermore, 4 out of 5 recognised conflicts around LTE decisions and 2 out of 3 faced them with anxiety or discomfort. In a previous study by this working group, one of the most frequent LTE measures is the formula "not amenable to aggressive measures", a term that is not very specific as the same measure seen by different professionals may or may not be considered aggressive. The authors conclude that this use of muLTEs results in not using correct and concrete terms and ending up delegating the decision to another time or another professional. Increased training in palliative care could reduce the use of the phrase "aggressive measures" and reduce the anguish generated by LTE(9).
In the evaluative qualitative research of Bárzaga Morell et al.(8) evaluates the knowledge of physicians about LTE in physicians of a university hospital in Cuba and used qualitative variables and techniques to collect information. A total of 124 medical professionals were surveyed, where most of them (77%) were aware of the term LTE and 24.2% were not in favour of the application of this procedure. The authors argue from an ethical analysis that not everything that is technically possible is ethically accepTable and hence there are reasons to limit therapeutic effort. However, many physicians are not sufficiently clear about this, which led the authors to conduct this study. The authors proceeded to construct a scale with three categories (low knowledge, accepTable knowledge and adequate knowledge). The results of the study show that of the 77% of respondents who were aware of the term LTE, only 58.1% did not confuse the term with other types of medical attitudes and behaviours. Interestingly, 24.2% of the respondents are not in favour of the application of LTE. 93.5% felt that adequate bioethics training would help in decision-making on these issues. The authors conclude that they are concerned that only 21% classified with adequate knowledge, indicating the need for improvement in this area and demonstrating that there are significant limitations. The authors discuss the factors that influence LTE decision making, as prior personal or family experience with this type of situations becomes a crucial element that cross-cuts attitudes and practices around the issue(8).
There are few studies that approach LTE from the nursing perspective. One of them is Velarde García et al.(15), whose qualitative phenomenological study aims to describe the experience of intensive care nurses in the Madrid Health Service. The study uses purposive and snowball sampling methods and data collection methods include a semi-structured and unstructured face-to-face interview, field notesfrom the researchers and personal letters from the participants. The data analysis used the approach of Giorgi A. The survey obtained a total of 22 nurse participants and identified 3 themes related to their experiences about LTE: a) experiencing relief, b) acceptance of the medical decision, c) implementation of LTE. The study particularly emphasises that the decision to implement LTE is one of the most relevant clinical situations for health professionals as it can generate a high level of psychological conflict and anxiety. The International Nursing Research Group "End of Life Decision-Making in Intensive Care Research Group analysed nurses" compared decision-making practices in intensive care units in 5 countries with different contexts: Brazil, England, Germany, Ireland and Palestine. The group reported that nurses did not make "last" decisions at the end of life, but sought consensus and provision of comfort care. In addition, the group described differences in relation to power dynamics in nurse-physician relationships, particularly in relation to cultural perspectives on dying and the development of palliative care. This is paradoxical especially when the Worldwide End of Life Practice for Patients in Intensive Care Units (WELPICUS) reported that decision making regarding end-of-life care takes place by consensus of medical and nursing staff and should be done by a multidisciplinary team. The results describe that nurses felt excluded from the decision-making process despite being burdened with the responsibility of implement limitation of therapeutic effort and maintain patient comfort, as well as to advocate for the patient's best interests. Nurses sometimes felt that physicians gave a false image of recovery or blocked any end-of-life discussion. The authors conclude that interprofessional collaboration has proven to be a tool that improves ICU patient care, decreasing complications and improving communication, trust and the nurse-physician relationship(15).
Finally, the qualitative study conducted in the USA (Pennsylvania) by Stokes et al.(16) aimed to explore and understand the factors influencing intensive care unit nurses' involvement in LTE decision-making or slow codes. The authors used the grounded theory of Strauss and Corbin's(17) to collect, analyse and code the data. The authors describe in their article the lack of meaningful input from nurses in end of life decision making despite being a fundamental part of patient care, which generates negative feelings and moral conflicts when they are forced to provide aggressive patient care to patients at the end of life. The authors obtained 5 categories: 1) recognition of patient and family values at the end of life; 2) procrastination and reluctance in decision making; 3) harm and suffering caused by the physical components of CPR; 4) emotional and moral response of the patient to aggressive delivery; 5) choosing limited resuscitation without a physician's order. There were several factors that influence the negative feelings and moral distress that some nurses exhibit when performing slow codes to preserve their own moral conflict, while other nurses refrain unless there is a specific physician order to provide limited care. The authors conclude that moral values have a strong influence when treating patients with aggressive measures at the end of life. Nurses empathise and consider cultural, religious and spiritual factors in end-of-life processes, and some of them consider participation in LTE an ethical obligation to minimise harm during the end of life process. Nurses present feelings of hopelessness and lack of autonomy and control over decisions surrounding the end of life(16).
Data were then extracted from each article and organised in a matrix (Table 1) for the purpose of synthesis. These extracted data include the title of the study, authors, year of publication, objective of the study, research design and results of the studies and articles. A content analysis was conducted to identify the theme among the extracted data and had the following characteristics:
DISCUSSION
In recent years, there has been a significant growth in scientific interest in end of life care. However, most of the publications on the subject are focused on caregivers in paediatric and/or adult intensive care units, which differs from the main characteristics of the patients in this systematic review. Decision making and adequacy of therapeutic effort may have different approaches between critically ill and terminally ill patients(7).
Illness, suffering and death are inherent to the human condition, which makes it consistent to understand that progress in medical sciences, biotechnology, as well as the growing human needs and increased in life expectancy have generated the need to rethink the purpose and scope of medicine. Personal experience is a determining factor in the type of attention and care provided to the patient, since previous personal or family experience of LTE situations is one of the factors that influence decision making and attitudes in clinical practices(8). The exercise of autonomy enables individuals to take responsibility for their own lives and take control of it. Decision making while respecting patient autonomy requires reciprocal recognition and a relationship of trust between patient and professional and, on the other hand, the initiative of the professional to share decisions(18).
Interprofessional collaboration has been shown to be the most effective method used as a tool for complex end of life decisions because it decreases complications and improves trust, communication and the relationship between nurses and physicians. For nurses, end of life may involve significant ethical conflicts because the withdrawal of therapeutic measures may sometimes involve the withdrawal of measures that could be related to maintaining patient comfort.(15) In addition, a common sense of dissatisfaction on the part of nurses about end of life can be extracted from most studies because in most cases, decisions are made by physicians without involving nurses even though nurses are the professionals who spend the most time with the patient. Nurses describe having feelings of hopelessness and lack of autonomy in these end of life processes(16).
In relation to the concept of LTE, we must bear in mind that it presents small conceptual nuances that are being raised in different forums in the field of clinical ethics. We suggest the need to adjust the nomenclature in order to adequacy of therapeutic effort and thus avoid misuse of the concept and favor transparency and understanding between patients and professionals. Given that the ethical implications are the same if it is decided not to initiate or to withdraw treatment, the second term is considered more appropriate, as the use of certain drugs is not limited, but rather the means are adapted to the patient's condition. The term appropriateness of therapeutic effort allows a broader use of the concept towards patients who are not necessarily facing the end of life in the short term, although it is true that the use of the LTE concept is the most widespread in clinical practice. Furthermore, the adequacy of therapeutic effort reinforces the principle of justice as it may not require a greater input of pharmacological resources, but perhaps more human resources.(19) A recent study by the SEMI (Spanish Society of Internal Medicine) Bioethics Working Group shows that only a minority is familiar with the definition of LTE and uses the term clearly and appropriately despite the fact that most professionals consider conflicts around end of life and adequacy of therapeutic effort to be frequent and relevant(10).
In summary, the most frequent ethical problems encountered in clinical practice are those related to the end of life, such as decisions to limit therapeutic effort, the use of palliative treatments, the establishment of non-CPR orders, decision making in incompetent patients and conflicts that arise within the clinical relationship. These results are very similar to those obtained in Anglo-Saxon and European studies. In an American study by McCarthy et al., conflicts arising from goal-of-care setting were identified as particularly problematic, resulting in discrepancies in the appropriateness of therapeutic measures(10).
In Latin America, research has been carried out on the knowledge and practice of LTE, in which the lack of familiarity and discordance of health professionals with the concepts is evident. It can also be observed that most of the studies found are limited to intensive care services and do not address the role of nurses in almost any of them(7),(8).
The formula "not amenable to aggressive measures" is frequently used in patients at the end of life as one of the LTE measures. This ambiguous terminology gives rise to conflicts in care because, depending on the clinical situation, the same measure may or may not be considered aggressive. The use of the so-called "aggressive measures" leads to the decision on the adequacy of the therapeutic effort to another time or to other professionals.(9) Allowing the patient to choose between various options, including the option of no treatment, will help to avoid offloading all the responsibility in to the physician and will ensure that decisions are more prudent, that the patient can be considered as a whole (his biography, biology, values and environment) and that a deliberative process is established which is essential for teamwork(12),(20).
Many authors conclude that LTE is a subject of great controversy from a bioethical, religious and legal point of view due to the lack of clinical practice guidelines and literature that goes beyond the patient in critical conditions.(7) On the other hand, there is a great incapacity to identify ethical problems in daily clinical practice, which has been called "axiological blindness", and is one of the main difficulties to be overcome in the ethical training of health professionals(10).
Numerous studies emphasise the great role of nursing not only for its technical qualifications, but also for its humanising vision of care and the ethics of care; numerous studies also denounce "that vital decisions regarding terminal patients admitted to the ICU are taken without the opinion of nurses, and often without their being informed of the reasons for such decisions, when, however, it is the nurse who carries out the actions of withdrawing life-sustaining treatments". In this respect, see the multicentre study carried out in 133 French ICUs by Ferrand E, Lemaire F, Regnier B, Kuteifan K, et al.(21)
We consider that this review may have some limitations in relation to the diversity of evidence, as this Scoping Review is limited to articles that were available with freely available full text and coverage of a larger number of databases could have provided other important contributions to the analysis of the results.
CONCLUSIONS
The results found have allowed us to respond to the initial objectives of this review, although there have been difficulties in finding specific studies focused on adult patients at the end of life who are not in critical care units, in addition to the difficulties felt by nurses and their feelings of lack of authority and participation in the decision-making process at the end of life and care focused on the good death. Generally speaking, in their daily clinical care, health professionals report obstacles in defining the term LTE accurately, some conflict with their LTE decisions, difficulties in end-of-life decision-making, the use of palliative treatments, the implementation of non-CPR orders, and anxiety about end of life care planning.
During the analysis of the contents extracted from the articles, it has been possible to infer that these difficulties were constituted as precursors to promote and prioritise the design of training programmes in ethics, in communication strategies and skills, in end-of-life and palliative care to enable a more precise approach and recognition of those processes and patients that require the adequacy of the therapeutic effort.
In summary, current recommendations for end-of-life decision-making are focused on joint decision-making involving the care team and involving the patient-family in the participatory deliberation process. In complex end of life situations, moral principles have achieved a unique significance in clinical practice. A framework of shared decision-making based on the best scientific knowledge and mutual respect of all parties involved is recommended, which is achieved through the development of comprehensive strategies and training programs.
In view of the above, we consider this review as a basis for future research, leaving the challenge for the elaboration of primary studies aimed at the study of the patient not only in critical conditions, the involvement of nursing in decision making at the end of life and the implementation and improvement of processes and care at end of life, being an important phenomenon for the nursing profession and, however, little studied.
REFERENCIAS
1. Betancourt Reyes GL. Un dilema ético actual: ¿Ensañamiento terapéutico o adecuación del esfuerzo terapéutico? Rev medica electron. 2017;39(4):975-86. [ Links ]
2. García Caballero R, Herreros B, Real De Asúa D, Alonso R, Barrera MM, Castilla V. Limitación del esfuerzo terapéutico en pacientes hospitalizados en el Servicio de Medicina Interna. Rev Calid Asist [Internet]. 2016;31(2):70-5. [ Links ]
3. Lantigua IF. Eutanasia, muerte digna, suicidio asistido ¿cuál es la diferencia? El mundo. 2019. En línea: https://www.elmundo.es/sociedad/2015/10/01/560d2c93ca4741da2a8b4579.html [ Links ]
4. Francisco Fernández Dorado Pau Garro Martínez. LA ATENCIÓN AL FINAL DE LA VIDA XI Conferencia de Expertos de la SOCMIC 2016. [ Links ]
5. Mansilla Olivares A, López-Bárcena J, Valenzuela-Gómez-Gallardo F, Rojo-Medina J, Meneses-González F, Vázquez-De Anda GF, et al. National Academy of Medicine of Mexico posture with regard to end-of-life decisions. Gac Mexico. 2019;154(6):628-31. [ Links ]
6. Sanchiz OR, Pascual LV. Revista de Bioética y Derecho Perspectivas Bioéticas Limitation of life support. Palliative care and end of life in ICU. 2020;(c):81-93. [ Links ]
7. Vallejo LI, Palacio AM, Marulanda V, Restrepo A, Yepes LA, Valencia NL, et al. Evaluación del conocimiento y práctica de la limitación del esfuerzo terapéutico en personal asistencial de una institución prestadora de servicios de salud para pacientes oncológicos de Medellín, 2018. Pers y Bioética. 2020;24(2):177-87. [ Links ]
8. Bárzaga Morell S, Estrada García CB, Sánchez Vila HJ, Berdú Saumell Y. Conocimiento y actitudes de los médicos sobre limitación de esfuerzo terapéutico TT - Knowledge and attitudes of physicians about limitation of therapeutic effort. Multimed (Granma) [Internet]. 2019;23(1):131-46. [ Links ]
9. García Caballero R, Real de Asúa D, García Olmos L, Herreros B. Do internists know what limitation of therapeutic effort means? Rev Clin Esp [Internet]. 2021;221(5):274-8. [ Links ]
10. Blanco Portillo A, García-Caballero R, Real de Asúa D, Herreros Ruíz-Valdepeñas B. Which are the most prevalent ethical conflicts for Spanish internists? Rev Clínica Española (English Ed. 2021;221(7):393-9. [ Links ]
11. Alcaraz A. Distanasia, un dilema del personal médico. Rev científica ciencias la salud. 2022;4(2):108-11. [ Links ]
12. González R. Documento Sobre La Adecuación Del Esfuerzo Terapéutico Área De Salud De León. 2017. [ Links ]
13. González-Rincón M, Díaz de Herrera-Marchal P, Martínez-Martín ML. The role of the nurse at the end of the life of a critically ill patient. Enferm Intensiva [Internet]. 2019;30(2):78-91. [ Links ]
14. Yañez-Dabdoub M, Vargas-Celis I. Cuidado humanizado en pacientes con limitación del esfuerzo terapéutico en cuidados intensivos: desafíos para enfermería. Pers y Bioética. 2018;22(1):55-68. [ Links ]
15. Velarde-García JF, Luengo-González R, González-Hervías R, Cardenete-Reyes C, Álvarez-Embarba B, Palacios-Ceña D. Limitation of therapeutic effort experienced by intensive care nurses. Nurs Ethics. 2018;25(7):867-79. [ Links ]
16. Stokes F, Zoucha R. Nurses' Participation in Limited Resuscitation: Gray Areas in End of Life Decision-Making. AJOB Empir Bioeth [Internet]. 2021;12(4):239-52. [ Links ]
17. Corbin JM, Strauss A. Grounded theory research: Procedures, canons, and evaluative criteria. Qual Sociol. 1990;13(1):3-21. [ Links ]
18. Reyes B, Betancourt B. Adecuación del esfuerzo terapéutico: aspectos éticos y legales relacionados con su práctica. Rev Cub Med Int Emerg. 2017;16(1):12-24. [ Links ]
19. Yuguero O, Esquerda M, Pifarre J. To limit or to adapt the therapeutical effort? Med Clin (Barc) [Internet]. 2019;152(5):e27. [ Links ]
20. Hernández-Tejedor A, Martín Delgado MC, Cabré Pericas L, Algora Weber A. Limitación del tratamiento de soporte vital en pacientes con ingreso prolongado en UCI. Situación actual en España a la vista del Estudio EPIPUSE. Med Intensiva. 2015;39(7):395-404. [ Links ]
21. Ferrand E, Lemaire F, Regnier B, Kuteifan K, Badet M, Asfar P, et al. Discrepancies between perceptions by physicians and nursing staff of intensive care unit end-of-life decisions. Am J Respir Crit Care Med. 2003;167(10):1310-5. [ Links ]
Received: January 20, 2023; Accepted: March 05, 2023











 texto en
texto en