Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Enfermería Global
versión On-line ISSN 1695-6141
Enferm. glob. vol.22 no.71 Murcia jul. 2023 Epub 13-Nov-2023
https://dx.doi.org/10.6018/eglobal.555501
Reviews
Nursing care for people undergoing bariatric surgery: integrative review
1State University of Maringá, Graduate Program in Nursing. Paranavaí, Paraná, Brazil
2State University of Paraná. Paranavaí, Paraná, Brazil
3Federal University of Mato Grosso do Sul, Post Graduation Program in Nursing. Campo Grande, Mato Grosso do Sul, Brazil
Objective:
To identify from the scientific literature the Nursing care provided to people with obesity undergoing bariatric surgery.
Method:
Integrative literature review, searches were carried out from July to August/2021 in four databases: MEDLINE, LILACS, BDENF and EMBASE. The research question was delimited through the PICo strategy, considering P - Patients with obesity; I - Nursing care; Co - Obese patients undergoing bariatric surgery. The following question was elaborated: "What are the main Nursing care in patients with obesity who underwent bariatric surgery?". Inclusion criteria primary articles that met the guiding question; available in full; during the period from 2016 to 2021; Portuguese, English and Spanish languages. Exclusion criteria gray literature, studies that did not respond to the guiding question. Search results were analyzed and interpreted.
Results:
14 articles were included in the research synthesis. Analysis of the results showed that the Nursing care provided to people undergoing bariatric surgery was identified in the preoperative period: health education regarding the surgical procedure and possible complications; and in the postoperative period: guidelines for relieving anxiety. In the intraoperative period, care procedures were not mentioned.
Conclusion:
Considering, therefore, the presentation of results, the findings demonstrate the unequivocal need for and importance of incorporating new technologies in Nursing care; promote the training of skills and abilities of team members, in addition to carrying out new research that allows expanding the performance of the Nursing team in the care of patients undergoing bariatric surgery.
Keywords: Bariatric Surgery; Nursing care; Obesity
INTRODUCTION
Obesity represents a worldwide public health problem and is the second most important factor for the global burden of Chronic Noncommunicable Diseases (NCDs). The prevalence of obesity has nearly tripled in recent decades, and it may be responsible for the loss of approximately 4 million people a year (1).
Due to this high mortality rate, most of the world's population lives in countries where more obese people die than those with low weight, reiterating the magnitude of this problem, especially when analyzing the cutoff point that characterizes the severely obese (BMI > 40.0 kg/m2) (1).
In Brazil, annual obesity prevalence indicators show a statistically significant temporal variation for the adult population (≥18 years old), of both gender, which in 2006 was 11.8% and in 2019, 20.3%. If this trend is maintained, it is estimated that the prevalence will reach 30% of the adult population by 2030. Along the same lines, the prevalence of overweight in adults would increase from the current 60% to 70% in 2030 (2).
In this scenario, bariatric surgery (BS) has been considered an important strategy in the treatment of severely obese patients and, currently, it is the most effective and long-lasting treatment in the control of associated diseases since it provides improvements in several vital functions of the individual (3),(4).
As of March 2013, surgical interventions for severe obesity began to be performed by the Sistema Único de Saúde [Unified Health System] - SUS, with Brazil being the second country to perform BS (5).
The postoperative period requires highly complex care for individuals with obesity, in accordance with the rules and criteria defined in Ordinance No. 425/19-03-2013 MG/MS, which institutes the surgical treatment of obesity and pre- and post-bariatric surgery follow-up at an outpatient clinic (6). In view of this, Nursing care, considering the specificity in the areas of surgical hospitalization, surgical center, and anesthetic recovery, must provide the patient with individualized and continuous assistance in the pre, trans and postoperative periods (7).
In this context, it should be noted that the Nursing team plays a crucial role in achieving the overall quality of care, with a concern to offer surgical patients qualified, humanized care, consistent with the precepts of the SUS and aimed at preventing complications, from surgical anesthesia to full recovery, in addition to contributing to ensuring safety, stress reduction and patient well-being (7).
It is perfectly accepted that the concept of perioperative practice is related both to the activities developed during the care phases, preoperative, intraoperative, and postoperative, as well as to more advanced ones, such as patient education, counseling, data collection, planning and assessment, fundamental for patients after bariatric surgery in the process of recovery and resumption of daily life, skills inherent in Nursing care (7),(8).
Given this, it is possible to ask: what is the main Nursing care offered to people undergoing bariatric surgery? Thus, the identification of Nursing care offered to people undergoing bariatric surgery may offer subsidies for the construction and implementation of consultation protocols by the rehabilitation Nursing team, in addition to elucidating the need for systematization of the care provided.
The present study seeks to advance in the construction of knowledge regarding the theme, since it proposes to identify in the scientific literature the Nursing care provided to people with obesity undergoing bariatric surgery.
MATERIAL AND METHOD
This is an integrative literature review (ILR) that provides comprehensive reviews, offers an opportunity to formulate global conclusions based on the analyzed research, reflections on future research and the implications for practices of the identified knowledge (9). To carry out this review, six steps were developed: 1. Identification of the theme and selection of the guiding question; 2. Establishment of inclusion and exclusion criteria; 3. Definition of extraction and categorization of studies; 4. Evaluation; 5. Interpretation of results; 6. Presentation of the summary of the content.
The research question was delimited through the PICo strategy, being P - Population, I - Phenomenon of Interest and Co - Context. Thus, the following structure was considered: P - Patients with obesity; I - Nursing care; Co - Obese patients undergoing bariatric surgery. Thus, the following question was elaborated: "What are the main Nursing care in patients with obesity who underwent bariatric surgery?".
In the second step, the inclusion and exclusion criteria of the study and the use of databases for search, extraction and selection of studies were defined. The inclusion criteria adopted were primary articles that met the guiding question; available in full; published in journals during the period from 2016 to 2021; in Portuguese, English, and Spanish. As far as you are concerned, the exclusion criteria were case reports; abstracts presented at conferences; clinical cases; dissertations; theses and studies already selected in the search in another database and that did not answer the guiding question.
Data were searched from July 20 to August 20, 2021, in the following databases: Medical Literature Analysis and Retrieval System Online (MEDLINE) via PubMed, Latin American and Caribbean Literature in Health Sciences (LILACS) and Nursing Database (BDENF) via VHL and Embase (Excerpta Medica database) by two reviewers independently. For the search in the VHL, the following Health Descriptors (DeCs) were used: ((Patients) AND ("biomarkers") OR ("patient") AND ("obesity") OR ("excess weight") AND ("nursing care") OR ("nursing care") AND ("bariatric surgery"). In the databases (MEDLINE) via PubMed and Embase, Medical SubjectHeadings (MeSH) descriptors were used: (("Patients") AND ("Biomarkers") OR ("patient") AND ("Obesity") OR ("overweight") AND ("Nursing care") AND ("Bariatric surgery"), using Boolean operators (AND and OR). Table 1 presents the search strategies in the databases.
Table 1. Search strategies in databases and identified results. Paranavai, Paraná, Brazil, 2021.
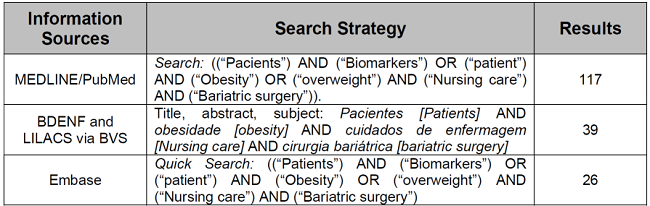
Source: study authors, 2021.
In the third step, the identification of pre-selected studies was carried out by reading the abstracts and titles of publications and organizing the studies. It is worth noting that the search strategy was developed independently by two researchers and blindly. The fourth step consisted of the studies selected by reading them in full.
In the fifth step, the results were analyzed and interpreted. In order to assess the methodological quality of the eligible articles, as well as to carry out a critical analysis of these studies, the evaluation instrument that classifies the articles in levels of scientific evidence from the Agency for Healthcare Research and Quality (AHRQ) was applied, which covers six levels: (I) evidence resulting from meta-analysis and systematic review; (II) evidence obtained from randomized clinical trials; (III) evidence obtained from clinical trials without randomization; (IV) evidence from cohort and case-control studies; (V) evidence from a systematic review of descriptive and qualitative studies; (VI) evidence based on a descriptive or qualitative study; (VII) evidence from the opinion of authorities and/or report of specialty committees (10).
The review and synthesis of knowledge were presented in the sixth step of the research. As for the studies, they were identified by an alphanumeric code and analyzed by two independent reviewers, consisting of the letter E for study and numbering from 1 to 14. E1, E2 and so on sequentially.
RESULTS
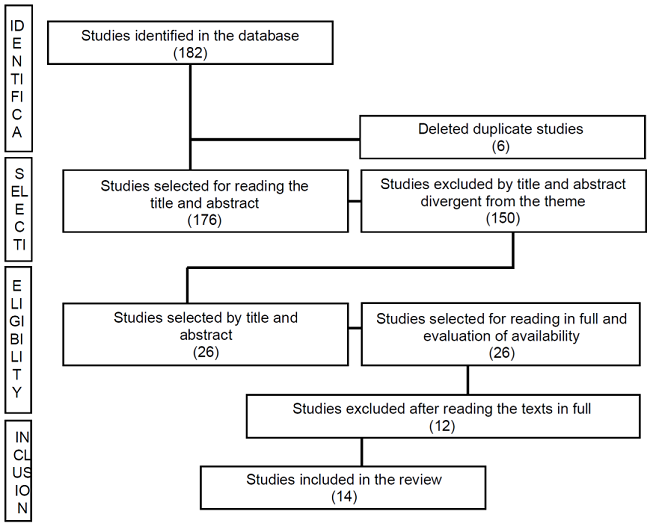
A total of 182 references were identified in the four databases, distributed as follows: 39 (21.43%) LILACS and BDENF via VHL; 117(64.29%) on PubMed; and 26(14.28%) at Embase. After the detailed analysis and application of the eligibility criteria, 150 (82.42%) publications were excluded, six (3.3%) due to duplicity and 150 (96.2%) for not addressing the topic after reading title and abstract. After excluding duplicate publications and selecting by title and abstract, 26 (14.3%) references were analyzed in full and 12 (46.15%) were excluded for not responding to the guiding question. Therefore, of the studies found in the database, 14 (7.69%) met the requirements of the established criteria, answered the guiding question, included in this review. The search process for identification, selection, eligibility, inclusion of the study was systematized using the flowchart recommended by the Preferred Reporting of Systematic Reviews and Meta-Analyses (PRISMA). It is represented in Figure 1.
The study consisted of 14 primary articles and the qualitative approach predominated in 42.85%. Of these, 21.43% were characterized as descriptive; 14.29% as a retrospective cohort; and 7.14% as a randomized clinical trial.
Regarding the location of the studies included in this review, four (28.57%) were produced in the USA, the others in Brazil, Spain, Canada, China, France; and 71.43% in Turkey. All selected studies were available in English and being published in journals, from 2016 to 2020.
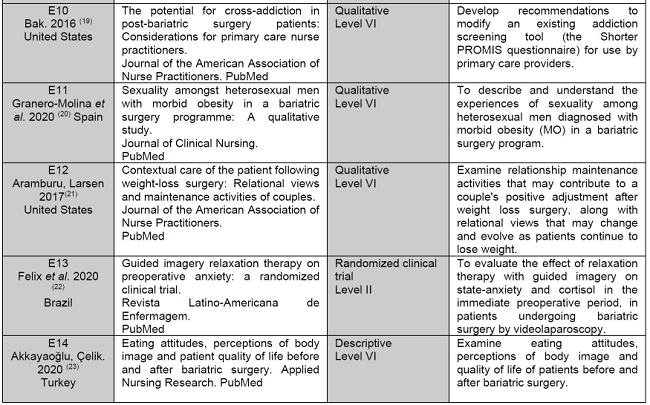
It is observed, based on the AHRQ categories, that 64.29% of the articles were classified as evidence level VI. Table 2 presents a summary of the characteristics of the included studies (10) (11) (12) (13) (14) (15) (16) (17) (18) (19) (20) (21) (22) (23).
Table 2. Descriptive analysis according to authors, country, year of publication, titles, journals, databases, type of study, level of evidence and objectives. Paranavaí, Paraná, Brazil. 2021.
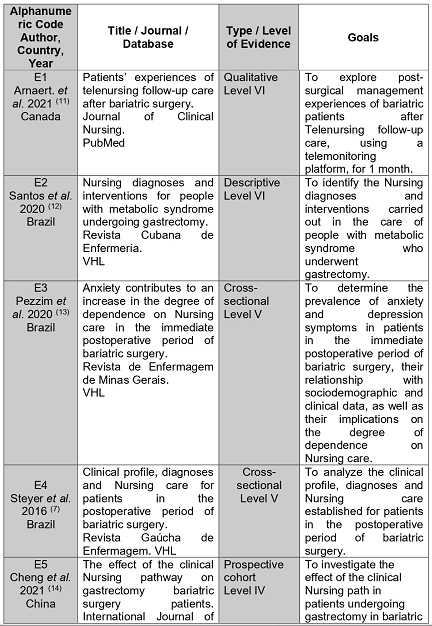
Table 2 (cont.). Descriptive analysis according to authors, country, year of publication, titles, journals, databases, type of study, level of evidence and objectives. Paranavaí, Paraná, Brazil. 2021.

Table 2 (cont.). Descriptive analysis according to authors, country, year of publication, titles, journals, databases, type of study, level of evidence and objectives. Paranavaí, Paraná, Brazil. 2021.
Source: Elaboration of the authors by the result of the Databases, 2021
Among the studies included in the search, it is observed that studies E2, E3 and E4 were the ones that evidence Nursing Care (NC), and E2 reports EC both preoperatively and postoperatively, in EC intraoperatively -operative refers that there were guidelines, but does not mention which ones (12) (13) (7). Study E3 refers to FB in the immediate postoperative period and E4 shows FB in the postoperative period (12),(7). Studies E5, E6, E9 and E14 generally mention it, while the other studies: E7, E8, E10, E11, E12 and E13 do not mention EC (14) (15) (16) (17) (18) (19) (22) (23).
Among the tools used in the different Studies, the highlight is the use of Telenursing in studies E1 and E6; in articles E2 and E4, the tool used was the Nursing Diagnosis of Nanda-I, while E3 presents a patient classification instrument - Fugulin- as a tool used (11) (12) (7) (15). Chart 3 presents a summary of Nursing care in the selected studies.
Chart 3: Descriptive summary of nursing care in the pre, intra and postoperative periods of bariatric surgery and tools. 2021.
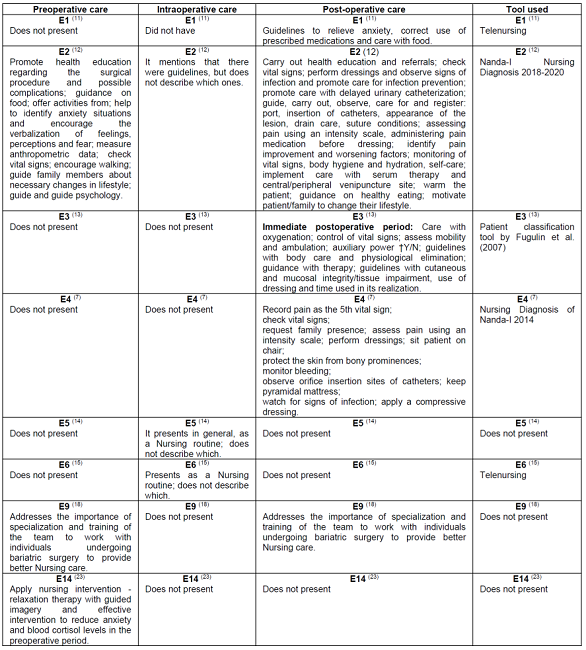
Source: Elaboration of the authors by the results of the Databases, 2021
After a careful analysis of the Nursing care and the tool used, the data were categorized and separated so that they were arranged in periods, being preoperative, intraoperative and postoperative of the BC (11) (12) (13) (14) (15) (23).
In three studies, characterizing (21.43%), in Nursing care for people undergoing BS, in the preoperative period, it was possible to highlight: health education regarding the surgical procedure and possible complications; feeding guidelines; offer fun activities aimed at reducing tension, helping to identify anxiety situations and encouraging the verbalization of feelings, perceptions and fear; check weight, measure abdominal circumference; check vital signs; encourage walking; guide the family about changes in lifestyle; guide and refer to the psychologist (11) (12) (13). In another study, the importance of specialization and training of the team to work with individuals undergoing bariatric surgery is addressed, to provide better Nursing care and apply Nursing intervention, relaxation therapy with guided imagery and effective intervention, aiming at reducing anxiety and blood cortisol levels, in the preoperative period (18),(23).
Compared with the other operative periods, Nursing care related to the intraoperative period appears in three articles, that is, in 21.43%. During this period, Nursing care is mentioned in a generalized way, as a Nursing routine, but the articles do not specifically describe what these cares are (12) (14) (15).
Regarding Nursing care in the postoperative period, it is important to highlight that, of the selected studies, those with the highest prevalence were E1; E2; E3; E4; E9, characterizing 35.71% of the articles (11) (12) (13) (7) (18). Therefore, in line with the importance of care, the most cited were guidelines and care to relieve anxiety; use of prescription drugs; use of correct, healthy and auxiliary food if necessary; care with hygiene, body hydration and skin integrity; observe physiological eliminations (11) (12) (13). In addition to these, other precautions were also identified, referring to the monitoring and control of vital signs, and the use of oxygen; pain assessment, using the intensity scale, improvement and worsening factors, in addition to registration as the fifth vital sign(12) (13) (7).
Among the five articles specifically related to Nursing care, it was possible to verify the emphasis on care with dressings, insertion of catheters, drains and conditions of sutures, in addition to their execution, observation to prevent signs of infection; the use of urinary catheters, care with serum therapy and the central/peripheral venipuncture site; the patient's and family's motivation to change their lifestyle and encourage their family's presence; assessment of mobility and ambulation; sit the patient in the chair; protect the skin from bony prominences; monitor bleeding; keep pyramidal mattress(12,13.7). Still regarding the articles, it was noticed in them the concern with the search for the improvement of Nursing care, thus emphasizing the importance of specialization and training of the members of the team in charge of working with individuals undergoing bariatric surgery (18).
DISCUSSION
It is observed that, in the selected studies, Nursing care focused on the preoperative and postoperative periods, showing a gap in the intraoperative phase. It is also noteworthy that the care identified addressed the need for a biopsychosocial dimension in Nursing care and the benefits of this type of care for obese patients undergoing bariatric surgery.
It should be noted that most of the findings were of a qualitative nature, which can be justified by the intention of the research to focus on understanding the nuances of Nursing care for people undergoing bariatric surgery. Thus understood, the care provided requires a holistic view, considering that it is of great importance to understand the biopsychosocial dimension of these individuals, aiming at qualified Nursing care.
Thus, it was verified that in the studies there was the option for the adoption of technological support, through Telenursing, as presented in articles E1 and E6 (11),(15). Do you know that this tool favors patient follow-up after bariatric surgery; and this enables consultations, assessments, guidance and Nursing prescriptions. In the scope of technology adoption, Telenursing is characterized by the association between telehealth and technology to offer remote Nursing monitoring, transposing the geographic barriers of efficient and safe care (24),(25).
In this context, many patients live far from the hospitals where the surgery was performed, so that visits to postoperative evaluations become costly and difficult for the patient to attend appointments. In this way, virtual care should be seen as an efficient tool for the continuity of care at home, in addition to enabling the reduction of care costs and allowing the patient some autonomy and capacity to be responsible for their care and post-operative recovery (26).
It should be noted that the advent of the COVID-19 pandemic promoted visibility to the use of technology to monitor the health of the population, reinforcing the efficiency of digital tools for the health area. In this regard, some studies highlight the usefulness of this technology in the remote mode for carrying out Nursing consultations, promoting health and preventing injuries. Therefore, through evidence-based guidelines passed on to people by Nursing professionals, allowing the follow-up of the necessary care at home (24),(27).
Qualitative research carried out in Brazil confirms the contribution of telehealth to Nursing care; however, he admitted difficulties in the communication process in the digital environment, stating that it is necessary to introduce disciplines that address communication skills in Nursing education to train future nurses in this type of care (28).
In another form of care for patients undergoing BS, two studies E2 and E4 focused attention on Nursing care, with the most cited being acute pain, risk of infection and impaired tissue integrity (12),(7). In these same studies, it was possible to verify that among the prescribed Nursing care, the most used were the use of protection mechanisms in the surgical positioning of the patient, recording pain as the fifth vital sign and checking vital signs. In this regard, another study mentions that pain assessment could be introduced, or not, in practice, as the fifth vital sign, while the collected data could serve as a guide for pain-related Nursing practice (29).
Therefore, pain management can be part of daily life, in providing care to patients in the postoperative period, emphasizing, therefore, that professionals should base their care practices on scientific evidence, always seeking to improve the quality of Nursing care (30).
It was also observed that, in addition to the biological aspects, other Nursing care involving changes of an emotional and/or psychiatric nature were performed, both in the preoperative period and in the postoperative period. In this sense, one of the studies E3 emphasizes the importance of Nursing research in mental health, in bariatric surgery patients, in the postoperative period, in order to diagnose anxiety and plan interventions (13).
These, therefore, are based on the identification of anxiety-causing factors, to determine and identify the level of knowledge about the procedure performed and its misconceptions; help the individual to deal with the situation, using attentive listening and respecting the desire; express hope, considering the limits of the client's situation; helping them to engage in activities that provide them with spiritual growth, in order to offer the best care for these individuals, considering that patients with anxiety symptoms require more complex Nursing care.
Some studies E7, E8, E11, E12 and E14 highlighted the importance of multidimensional assessment of the individual to identify disorders with the perception of body image in the postoperative period. Thus, these studies concluded the need for a more complete assessment by the Nursing team, with appropriate research instruments and open questions to allow the patient to share their feelings in relation to their new body and provide advice and guidance (16) (17) (20) (21).
All studies highlighted the importance of a holistic Nursing approach to improving care, such as fear and anxiety. Still in this perspective, a randomized clinical trial E14 evaluated the application of a Nursing intervention called "guided image relaxation therapy" and demonstrated that the intervention was effective in reducing anxiety and blood cortisol levels in the preoperative period, in patients submitted to bariatric surgery (23).
Studies E5 and E9 addressed the importance of specialization and training of the health team to work in the care of individuals submitted to BS, in order to provide better Nursing care (14),(18). One of the studies, E5, showed the difference between specialized and non-specialized nurses, demonstrating that the specialized team was responsible for accelerating recovery, reducing complications and pain, improving postoperative quality of life and increasing patient satisfaction with the Nursing team (14),(18). In view of this, the need is reiterated throughout the Nursing training process, as well as in continuing education actions developed with professionals, to provide opportunities for discussion and construction of specific Nursing actions that meet the needs of these individuals.
However, after analyzing all the studies included in this review, what is perceived is a lack of knowledge regarding intraoperative and postoperative Nursing care, considering that few provide Nursing care in these phases. Thus, the limitations in the scientific literature on this topic indicate the need for further research that demonstrates the importance of Nursing for care in the aforementioned statements.
May this study provoke reflections, influence new perceptions, habits, behaviors of nurses about the need to formulate Nursing care during the intraoperative and postoperative period, which may rebuild new practices in the care of surgical patients in institutions, where patients can receive assistance of Nursing with quality of life.
CONCLUSION
After carrying out the research that supported this article, it was concluded that in the selected studies, Nursing care highlighted the following situations: health education, regarding the surgical procedure and possible complications corresponding to the preoperative period; already in the postoperative phase, the presence of guidelines to relieve anxiety was evidenced. As for the intraoperative period, a gap was identified in the performance of the Nursing team, which was limited to complying with care routines, without mentioning Nursing care during this period.
Considering, therefore, the presentation of results, the findings demonstrate the unequivocal need for and importance of incorporating new technologies in Nursing care; promote the training of skills and abilities of team members, in addition to carrying out new research that allows expanding the performance of the Nursing team in the care of patients undergoing bariatric surgery. Thus, the adoption of these procedures can avoid possible failures in the performance of the Nursing team during the periods of bariatric surgery.
Acknowledgment
Professor Ana Carolina Pereira Simões from the State University of Paraná, for her encouragement and methodological support for this review research, which were fundamental.
REFERENCES
1. World Health Organization (WHO). Obesity and overweight, 2021.[acessado 2021 Jul 24]. Disponível em: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight. [ Links ]
2. Brasil - Ministério da Saúde. Secretaria de Vigilância em Saúde Departamento de Análise em Saúde e Vigilância de Doenças Não Transmissíveis, 2020. [acessado 2021 Jul 24]. Disponível:https://abeso.org.br/wp-content/uploads/2021/07/vigitel_brasil_2019_vigilancia_fatores_risco-1-2.pdf. [ Links ]
3. Chaim EA, Pareja JC, Gestic MA, Utrini MP, Cazzo E. Preoperative multidisciplinary program for bariatric surgery: a proposal for the Brazilian Public Health System. Arq Gastroenterol. 2017;54(1):70-74.[acessado 2021 Jul 24]. Disponível em: https://doi.org/10.1590/S0004-2803.2017v54n1-14. [ Links ]
4. Pereira RB, Rivera IR, Brito ZCT, Silva MAM. Effect of obesity on lung physiology and disturbances before and after bariatric surgery. Cienc. Cuid. Saúde. 2018;17(1). [acessado 2021 Jul 24]. Disponível em: https://periodicos.uem.br/ojs/index.php/CiencCuidSaude/article/view/34368. [ Links ]
5. Pereira LMC, Aidar FJ, Matos DG, Neto JPF, Souza RF, Sousa ACS et al. Assessment of Cardiometabolic Risk Factors, Physical Activity Levels, and Quality of Life in Stratified Groups up to 10 Years after Bariatric Surgery. International journal of environmental research and public health.2019;16(11):1975. [acessado 2021 Jul 24]. Disponível em:https://doi.org/10.3390. [ Links ]
6. Brasil - Ministério da Saúde. Estabelece regulamento técnico, normas e critérios para o Serviço de Assistência de Alta Complexidade ao Indivíduo com Obesidade, 2013. [acessado 2021 jul 31]. Disponível em: https://www.coffito.gov.br/nsite/?p=3355. [ Links ]
7. Steyer NH, Oliveira MC, Gouvêa MRF, Echer IC, Lucena AF. Clinical profile, nursing diagnoses and nursing care for postop- erative bariatric surgery patients. Rev Gaúcha Enferm. 2016 mar;37(1):e50170.doi: https://doi.org/10.1590/1983-1447.2016.01.50170 [ Links ]
8. Dolne F, Souza JSM de, Matte J. Nursing performance in observative patient care in the positive surgery of bariatric surgery. RBONE [Internet]. 2020 Nov.3 [cited 2022 May 10];14(87):550-9. Available from: http://www.rbone.com.br/index.php/rbone/article/view/1317 [ Links ]
9. Neves E, Ferreira KA, Melo TBA, Almeida A, Bezerra PVV, Bezerra FF, Bacelar LFF. The relevance of nurse in the follow-up of post-operative patients submitted to bariatric surgery: literature review. Braz. J. Surg. Clin. Res. 2018;28(3):07-92. [acessado 2021 jul 31]. Disponível em:https://www.mastereditora.com.br/periodico/20181006_152122.pdf. [ Links ]
10. Stillwell S, Melnyk BM, Fineout-Overholt E, Williamson K. Evidence-Based Practice: Step by step. Am J Nurs. 2010; 110(5):41-47. [acessado 2021 Ago 01]. Disponível em: https://journals.lww.com/ajnonline/Fulltext/2010/05000/Evidence_Based_Practice, Step_by_Step__Searching.24.aspx. [ Links ]
11. Arnaert A, Girard A, Craciunas S, Shang Z, Ahmad H, Debe Z, et al. Patients' experiences of telenursing follow-up care after bariatric surgery. Journal of Clinical Nursing. 09 July 2021. https://doi.org/10.1111/jocn.15955 [ Links ]
12. Santos I, Boery R, Fernandes J, Souza-Júnior E, Souza A. Diagnósticos e intervenciones de enfermería a la persona con síndrome metabólico sometida a gastrectomía. Revista Cubana de Enfermería [Internet]. 2020 [citado 10 Ene 2022]; 36 (4) Disponible en: http://revenfermeria.sld.cu/index.php/enf/article/view/3269 [ Links ]
13. Pezzim IM, Firmino APO, Carvalho R, Romero WG, Wandekoken KD, Fiorin BH et al. Ansiedade contribui para o aumento do grau de dependência da assistência de Enfermagem no pós-operatório imediato de cirurgia bariátrica. Reme : Rev. Min. Enferm. [Internet]. 2020 [citado 2022 Jan 09]; 24: e1321. Disponível em: http://www.revenf.bvs.br/scielo.php?script=sci_arttext&pid=S1415-27622020000100245&lng=pt. Epub 17-Ago-2020. http://dx.doi.org/10.5935/1415-2762.20200058. [ Links ]
14. Cheng C, Haiyan H, Xing N. The effect of the clinical nursing pathway on gastrectomy bariatric surgery patients. Int J Clin Exp Med 2021;14(2):1359-1365. Disponível: http://www.ijcem.com/files/ijcem0123435.pdf. [ Links ]
15. Neuberg M, Blanchet MC, Gignoux B, Frering V. Connected Surveillance for Detection of Complications After Early Discharge from Bariatric Surgery. Obes Surg. 2020;30(11):4669-4674. doi: https://doi.org/10.1007/s11695-020-04817-5. [ Links ]
16. Torrente-Sánchez MJ, Ferrer-Márquez M, Estébanez-Ferrero B, Jiménez-Lasserrotte MDM, Ruiz-Muelle A, Ventura-Miranda MI, Dobarrio-Sanz I, Granero-Molina J. Social Support for People with Morbid Obesity in a Bariatric Surgery Programme: A Qualitative Descriptive Study. Int J Environ Res Public Health. 2021 Jun 17;18(12):6530. doi: https://doi.org/10.3390/ijerph18126530. PMID: 34204427; PMCID: PMC8297395. [ Links ]
17. Perdue TO, Schreier A, Neil J, Carels R, Swanson M. A Concept Analysis of Disturbed Body Image in Bariatric Surgery Patients. Int J Nurs Knowl. 2020 Jan;31(1):74-81. doi: https://doi.org/10.1111/2047-3095.12220. Epub 2018 Jul 24. PMID: 30040231. [ Links ]
18. Holsworth C, Gallagher S. Managing Care of Critically Ill Bariatric Patients. AACN Adv Crit Care. 2017 Fall;28(3):275-283. doi: https://doi.org/10.4037/aacnacc2017342. PMID: 28847862. [ Links ]
19. Bak M, Seibold-Simpson SM, Darling R. The potential for cross-addiction in post-bariatric surgery patients: Considerations for primary care nurse practitioners. J Am Assoc Nurse Pract. 2016 Dec;28(12):675-682. doi: https://doi.org/10.1002/2327-6924.12390. Epub 2016 Jul 11. PMID: 27400415. [ Links ]
20. Granero-Molina J, Torrente-Sánchez MJ, Ferrer-Márquez M, Hernández-Padilla JM, Ruiz-Muelle A, López-Entrambasaguas OM, Fernández-Sola C. Sexuality amongst heterosexual men with morbid obesity in a bariatric surgery programme: A qualitative study. J Clin Nurs. 2020 Nov;29(21-22):4258-4269. https://doi.org/10.1111/jocn.15461. Epub 2020 Sep 3. PMID: 32786151. [ Links ]
21. Aramburu Alegría C, Larsen B. Contextual care of the patient following weight-loss surgery: Relational views and maintenance activities of couples. J Am Assoc Nurse Pract. 2017 Jan;29(1):17-25. doi: https://doi.org/10.1002/2327-6924.12372. Epub 2016 May 10. PMID: 27166854. [ Links ]
22. Felix MMDS, Ferreira MBG, Oliveira LF, Barichello E, Pires PDS, Barbosa MH. Guided imagery relaxation therapy on preoperative anxiety: a randomized clinical trial. Rev Lat Am Enfermagem. 2018 Nov 29;26:e3101. doi: https://doi.org/10.1590/1518-8345.2850.3101. PMID: 30517586; PMCID: PMC6280172. [ Links ]
23. Akkayaoglu H, Çelik S. Eating attitudes, perceptions of body image and patient quality of life before and after bariatric surgery. Appl Nurs Res. 2020 Jun;53:151270. doi: https://doi.org/10.1016/j.apnr.2020.151270. Epub 2020 Apr 18. PMID: 32451007. [ Links ]
24. Mussi FC, Palmeira CS, Santos CAST, Guimarães AC, Lima ML, Nascimento TS. Effect of nursing telemonitoring on the knowledge of obese women: clinical trial. Rev. Bras. Enferm. 2019;72(3):212-219.[acessado 2021 Ago 01]. DOI: http://dx.doi.org/10.1590/0034-7167-2018-0500. [ Links ]
25. Balenton N, Chiappelli F. Telenursing: bioinformation cornerstone in healthcare for the 21st Century. Bioinformation [Internet]. 2017 [cited 2018 Sept 11];13(12):412-4. Available from: https://dx.doi.org/10.6026/97320630013412. [ Links ]
26. Mirón RM, Ceballos FR, Parras PI, Palomo IA, Fernández FBM, Medina MJ, et al. Telemonitoring and home hospitalization in patients with chronic obstructive pulmonary disease: study TELEPOC. Expert Rev Respir Med. 2018 Apr;12(4):335-343. https://doi.org/10.1080/17476348.2018.1442214. [ Links ]
27. Oliveira SC, Costa DGL, Cintra AMA, Freitas MP, Jordão CN, Barros JFS et al. Telenfermagem na COVID-19 e saúde materna: WhatsApp(r) como ferramenta de apoio. Acta paul. enferm. 2021;34:eAPE02893. [acessado 2021 Ago 01]. Disponível em: http://www.revenf.bvs.br/scielo.php?script=sci_arttext&pid=S0103-21002021000100449&lng=pt. Epub 14-Jul-2021. http://dx.doi.org/10.37689/acta-ape/2021ao02893. [ Links ]
28. Barbosa IA, Silva MJP. Nursing care by telehealth: what is the influence of distance on communication?. Revista Brasileira de Enfermagem. 2017; 70(5):928-934 [acessado 2021 Ago 01]. Disponível em: https://doi.org/10.1590/0034-7167-2016-0142. [ Links ]
29. Ferrari MFM, Daher DV, Antunes JM, Amim EF, Jesus CM, Geraldo MA. Pain as the Fifth Vital Sign, Challenges For Its Incorporation in Health Training. REME - Rev Min Enferm. 2019;23:e-1233 Disponível em: https://cdn.publisher.gn1.link/reme.org.br/pdf/en_e1233.pdf. [ Links ]
30. Assis GLC, Sousa CS, Turrini RNT, Poveda VB, Silva RCG. Proposal of nursing diagnoses, out-comes and interventions for postoperative patients of orthognathic surgery. Rev Esc Enferm USP. v. 52, n. 1, p. 1-7. 2018. Acesso: 20-01-2022. DOI: http://dx.doi.org/10.1590/S1980-220X2017025303321. [ Links ]
Received: January 27, 2023; Accepted: March 05, 2023











 texto en
texto en