Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Medicina Oral, Patología Oral y Cirugía Bucal (Internet)
versión On-line ISSN 1698-6946
Med. oral patol. oral cir.bucal (Internet) vol.11 no.2 mar./abr. 2006
Evaluation of 80 implants subjected to immediate loading in edentulous mandibles after two years of follow-up
Evaluación de 80 implantes, sometidos a carga inmediata en desdentados inferiores tras un seguimiento de dos años
José María Martínez González1 , Cristina Barona Dorado2 , Jorge Cano Sánchez3,
Fernando Fernández Cáliz2, Andrés Sánchez Turrión4
(1) Assistant Professor of Surgery. Madrid Complutense University Dental School
(2) Collaborating Professor. Madrid Complutense University Dental School
(3) Degree in Dental Surgery. Implantologist
(4) Assistant Professor of Prostheses. Madrid Complutense University Dental School. Madrid (Spain)
ABSTRACT
Aim: An analysis is made of the clinical and radiological
behavior of 80 implants with a new surface subjected to etching with a sulfuric
and hydrofluoric acid solution followed by thermal treatment, and subjected to
immediate loading in patients with lower overdentures.
Study design: A prospective observational study was made
of 20 patients with lower overdentures supported by four implants measuring 13
mm in length. All patients were included after the obtainment of informed
consent, anamnesis, clinical examination and radiological study, with prior
clinical elaboration of the lower dentures.
Results: Over two years of follow-up, no important plaque
or tartar accumulation was observed (with Silness and Löe indexes of 0-1).
Periodontal probing proved favorable, with no pocket depths of over 2 mm in any
case. The radiological controls showed no implant failures during follow-up. No
cervical bone loss was recorded in the first year in a large proportion of cases
(65%), while reabsorption of the cervical half was observed in 10%, and of three-quarters
of the cervical portion in the remaining 35%. Performance in the second year was
compatible with the standard references with losses of between 0.5-1.5 mm.
Conclusions: Rehabilitation with lower overdentures
should be regarded as a priority indication, and implantological treatment
substitution by conventional and/or early resting periods should be considered.
Key words: Implants, acid etching, immediate loading, overdentures.
RESUMEN
Objetivo: Analizar el comportamiento tanto clínico
como radiológico de ochentas implantes con una nueva superficie tratada
mediante una disolución de ácido sulfúrico y fluorhídrico con posterior
tratamiento térmico, que han sido sometidos a carga inmediata en pacientes
rehabilitados con sobredentaduras inferiores.
Diseño del artículo: Estudio observacional, prospectivo en 20 pacientes
rehabilitados con sobredentaduras inferiores, soportadas sobre cuatro implantes
de 13 milímetros de longitud. Todos los pacientes fueron planificados e incluídos
tras el consentimiento, anamnesis, exploración clínica y estudio radiográfico
y mediante montaje clínico previo de la prótesis inferior.
Resultados: Durante los dos años de seguimiento, se ha obervado que el
acúmulo de placa y cálculo no ha sido importante, oscilando los índices (Silness
y Löe) entre 0 y 1. El sondaje periodontal, ha sido favorable no encontrando
pacientes que superasen 2 milímetros.
Los controles radiográficos mostraron a lo largo del seguimiento ausencia de
fracaso implantológico. Las pérdidas óseas cervicales, durante el primer año,
no existieron en un alto porcentaje (65%), mientras que en un 10% se produjo la
reabsorción de la mitad cervical y en el 35% restante sobre las ¾ partes
cervicales. El comportamiento durante el segundo año fue compatible a los
patrones estándares, observándose pérdidas que oscilaron entre 0,5 y 1,5 milímetros.
Conclusiones: La rehabilitación mediante sobredentaduras inferiores,
debiera contemplarse como una indicación prioritaria, planteándose la
sustitución de los tratamientos implantológicos con períodos de reposo
convencionales y/o precoces.
Palabras clave: Implantes, grabado ácido, carga inmediata, sobredentaduras.
Introduction
The anteroinferior region of the mandible is the prevalent initial zone for implant-based rehabilitation procedures. The first Results reported by Branemark established the principles for defining a series of selection and planning criteria. However, some authors soon questioned some of these principles. In this context, one of the most rigid guiding principles at the time referred to the osteointegration times: three months for the mandibular region and 4-6 months for the upper maxilla. In 1979, implantologists such as Ledermann (1) began to treat lower totally edentulous patients with overdentures, in the absence of any waiting period i.e., immediate loading was applied, with a success rate of 91.2%.
These early initiatives probably encouraged further developments, and years later improved performance figures were obtained. Thus, Schroeder (2) in 1983 reported a success rate of 98.1% in this same type of patient population. In 1986, Babbusch (3), adopting an identical treatment procedure and after a follow-up period of over 5 years, reported a 96.1% success rate.
In the nineties, Dietrich (4) applied immediate loading with a 94.6% success rate after 5 years, and finally in 1997, Chiapasco (5) published a retrospective study of 226 lower edentulous patients subjected to treatment in the form of overdentures with immediate loading. The Results were conclusive and similar to those reported above (96.9% success rate).
It was at this point in time, and coinciding with the Introduction of new implant surfaces, that immediate loading began to be viewed as a new approach to the management of implantological patients. Standardization of the procedure has remained elusive, however, due to the limited number of publications offering acceptable follow-up periods, and because of the important number of theoretically applicable surfaces.
In this context, the present study was designed to contribute new data on immediate loading involving a new surface subjected to etching with a sulfuric and hydrofluoric acid solution followed by thermal treatment.
Patients and Methods
Twenty patients (8 females and 12 males; age range 48-74 years) programmed for implantological mandibular rehabilitation in our Service were included in the study. The initial clinical examination included an assessment of the mucosal conditions, alveolar crest morphology, maxillary-mandibular relation and opposing occlusion (Table 1). Inclusion criteria were the absence of systemic diseases contraindicating surgery, and the obtainment of informed consent to immediate loading. A panoramic X-ray study and tomographic evaluation were made in all cases, and all patients were required to present a minimum bone height of 13 mm in the intermentonian region.
Imprints and casts were obtained for the wax preparations, followed by registries and mounting in teeth for the control of prosthetic height and occlusion. In this same phase the surgical splint was designed with guides for four implants in the intermentonian region.
Following the above steps, surgery was performed in the form of a triangular incision with a trajectory over the alveolar crest to the region of the second premolars, with anterior releasing incisions on the midline. Careful raising of the mucoperiosteal layer allowed for crest regularization where required, followed by placement of the surgical splint and the application of notches using rounded drills in the predetermined zones. The sequence required for preparation of the bone bed was completed using the appropriate drills (marker / pilot 2.8-3.0), with the placement of four 13-mm implants (Defcon TSA series 3, Avantblast® surface) using a threading drill with posterior mechanical insertion.
Following implant insertion with the corresponding transporters, the latter were removed and replaced with the specific imprint posts of the system, for the obtainment of heavy and fluid silicone imprints. Following withdrawal of the latter, the healing caps were positioned, and pharmacological treatment was prescribed: amoxicillin 750 mg/8 hours p.o. for 8 days, sodium diclofenac/12 hours via the rectal route for four days, and magnesium metamizol p.o. (in case of need).
On the following day the noble metal bar was submitted by the laboratory, the healing caps were removed following topical anesthesia of the zone, and insertion was carried out with radiographic confirmation of correct fitting. The healing caps were again removed 48 hours later, and the bar and completed prosthesis were positioned.
The first clinical controls were carried out four days later, with the evaluation of poorly fitting areas or interferences, and removal of the suture stitches. Strict instructions on hygiene of the prosthesis and bar were provided, and the patients were advised to gradually increase food consistency.
The same follow-up protocol was applied in all cases, with clinical controls after 15 days and after 1, 3, 6, 12, 18 and 24 months, in which the plaque and tartar index was scored as follows: 0 = absence of plaque and tartar; 1 = no visible plaque, with supragingival tartar; 2 = visible plaque, with supra- and subgingival tartar; and 3 = important accumulation of both plaque and tartar.
Periodontal probing was performed with a specific probe, expressing pocket depth in millimeters.
Radiological follow-up was carried out based on panoramic projections and periapical studies, assessing the presence of periimplant radiotransparencies and bone resorption as follows: 0 = absence, with covered implant head on crest; 1 = half of the cervical portion without bone covering; 2 = three-quarters of the cervical zone without covering; 3 = fully exposed cervical portion; 4 = loss affecting body and expressed in millimeters. These controls were made after 6, 12, 18 and 24 months.
Results
The plaque and tartar indices (Silness and Löe) were between 0-1, i.e., plaque and tartar accumulation was low (Figure 1).
These scores were recorded in 30% of cases in the first 6 months, and increased to 80% after one year. After cleaning of the bar, the patients were again instructed on the need to observe strict hygiene. This was followed by a decrease in plaque and tartar at the control visit after 18 months (50%), though the proportion increased again after 24 months (90%).
Regarding periodontal probing, the depth values recorded throughout the observation period did not exceed 2 mm with any of the implants.
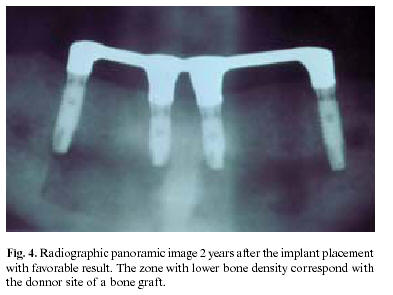
In the course of the two-year follow-up period, the radiological evaluations revealed no periimplant radiotransparencies suggestive of implant failure. None of the implants were lost in this period of time (Figures 2-4). As regards cervical bone loss very characteristic of implants with external connections it should be stressed that in the first year no absorption was noted in a large proportion of cases (65%), while reabsorption of the cervical half was observed in 10%, and of three-quarters of the cervical portion in the remaining 35%. Performance in the second year was compatible with the standard references with losses of between 0.5-1.5 mm (Figure 5).
Discussion
The present tendency of implant therapy is to prescribe immediate dental restoration, with the provision of esthetic performance adapted to the initial dental situation of the patient. However, in cases such as edentulous patients, the fundamental objective is to ensure increased denture stability. In such circumstances different aspects should be evaluated in order to decide whether to offer implant-supported fixed dentures, or a implant-mucosal-supported removable prosthesis (overdentures). The anatomical situation is a key consideration when immediate loading is contemplated, since the morphological and histological characteristics of the upper and lower jaw are distinct the mandible being defined as a quite favorable location (6).
The current state of implant surface technology likewise contributes to shorten the time to loading. In this context, and in addition to surface blasting procedures with or without acid etching or anodic oxidation, other techniques involving exclusively acid etching have been developed. The latter approach in the case of the Osseotite® surface makes use of etching with hydrofluoric acid (HF), hydrochloric acid (HCl) and sulfuric acid (H2SO4)(7). The Avantblast® surface belongs to this same group, and is subjected to sulfuric and hydrofluoric acid etching followed in a second phase by thermal treatment in an oven. This process affords surface roughness and a profile suitable for application in early and immediate loading protocols.
In the present study, lower overdentures were prescribed based on the defined inclusion criteria, with the evaluation of other aspects such as surgical time, subject age, opposing dentition and patient perspectives.
Surgical time is a factor to be taken into account when indicating treatment. Rehabilitation with four implants for overdentures implies a surgical time of 60-90 minutes, and the duration of the procedure increases in proportion to the number of added implants involved. Elderly patients (around 65 years of age) show lesser adaptability to prolonged surgery, as a result of which this treatment approach may be a good option in such cases. In our series the mean patient age was 62.6 years, with a broad range (48-74 years).
Another factor deciding the initial indication of lower overdentures was the observation that the opposing dentition in many cases consisted of removable dentures. In such situations the proposed treatment offers a simple solution, involving smaller and more controlled masticatory forces. Of the 20 patients presented, 15 wore complete dentures and 5 had fixed restorations. After being informed of the possibilities afforded by fixed or removable rehabilitation, these 5 patients preferred the latter option due to its simplicity, rapidity (immediate loading), cost effectiveness and the possibility of increasing the number of implants in future, with conversion of the prosthesis from removable to fixed.
After global evaluation of the patient, careful instructions and information must be provided to ensure correct maintenance and follow-up of treatment.
As has been commented above, prior to actual surgery, it is important to test the prosthesis with teeth, so that both the vertical dimensions and occlusion characteristics can be anticipated.
The surgical technique is no different to conventional surgery, and we only recommend avoiding posterior releasing incisions with the performance of an anterior triangular releasing incision to minimize swelling of these posterior zones and ensure that mucosal seating of the prosthesis does not cause patient discomfort.
The choice of implants measuring 13 mm in length was based on the experience of most authors in relation to immediate loading the general recommendation being to use lengths in excess of 10 mm (8).
The obtainment of imprints and cooperation with the prosthesis laboratory are additional aspects of fundamental importance to shorten treatment times and ensure performance of the first test on the day after surgery. The bar used in this study consisted of noble metal in all cases correct fitting being confirmed radiographically. In only four cases was fitting suboptimal; the bar in these cases was sectioned and fixed again with rapid-setting resin and then welded.
During this procedure most patients expressed discomfort in response to manipulation in the zone; as a result, before removing the healing caps, we recommend local application of an anesthetic solution with a cotton swab. This same procedure is performed on the following day, coinciding with definitive placement of the bar and prosthesis.
At this point the patients received careful instructions on hygiene, with clinical controls according to protocol. As has been described under Results, follow-up based on the plaque and tartar levels proved quite satisfactory. The increments in plaque and tartar index recorded after one and two years should be regarded as a consequence of patient neglect thus stressing the importance of correct patient follow-up, information, training and motivation. Nevertheless, it is to be expected that at some time during treatment, loosening of the bar will be required for cleaning in an ultrasound bath and polishing, followed by repositioning within the mouth.
The periodontal index recorded during the study reflects adequate behavior of the periimplant soft tissues a decisive influence being played by the hygiene measures adopted and the presence of keratinized mucosa in all cases.
Once of the criteria for implantological success originally proposed by Albrektsson (9) was the maintenance of the marginal bone crest, with losses of between 1-1.5 mm being considered normal.
In 52 implants (65%), and in contrast to the normal situation, we recorded no reabsorption in the first year at implant cervical level. A number of hypotheses have been proposed to account for reabsorption, including a supposed attempt by the soft tissues to secure biological sealing. However, our own findings do not support this idea, in view of the high percentage absence of reabsorption in our series (10).
In turn, authors such as Hermann (11) suggest that such reabsorption Results from bacterial invasion of the existing microgap. According to these studies involving implants without loading, crest reabsorption is more accentuated in two-phase versus single-phase implantation. The Results of immediate loading in our study coincide with these observations and moreover suggest that the same principle could be extended to situations characterized by implant loading.
Lastly, overloading secondary to masticatory forces has also been proposed as a cause of bone crest loss. Isidor (12), among other authors, suggests that masticatory overload with good periimplant hygiene implies bone loss, while defective hygiene in the absence of overload produces no such loss. Our own Results support this idea, not in terms of hygiene (which was good), but because of the type of opposing occlusion involved. In effect, in the 52 implants (corresponding to 13 cases) without marginal bone loss, there were no parafunctional habits, and the opposing dentition consisted of complete dentures as a result of which masticatory overload was minimal.
Thus, it can be affirmed that final assessment of our immediate loading protocol after two years of follow-up suggests that rehabilitation with lower overdentures is an acceptable management option that affords excellent results.
![]() Correspondence
Correspondence
Dr. José María Martínez González
Facultad de Odontología.
Universidad Complutense de Madrid
E-mail: jmargo@odon.ucm.es
Received: 27-04-2005
Accepted: 30-11-2005
References
1. Ledermann PD. Stegprothetische versorgung des zahnlosen unterhiefers mit hilfe plasmabeschichteten titanschraubimplantaten. Deutsche Zahnartzlische Zeitung 1979;34:907-11. [ Links ]
2. Schroeder A, Maeglin B, Sutter F. Das ITI-Hohlzyl-inderimplantat Typ F zur Prothesenretention beim zahnlosen Kiefer. Schweizerische Monatschrift fur Zahnheilkunde 1983;93:720-33. [ Links ]
3. Babbusch CA, Kent J, Misiek D. Titanium plasma sprayed (TPS) screw implants for the reconstruction of the edentulous mandible. J Oral Maxillofac Surg 1986;44:274-82. [ Links ]
4. Dietrich U, Skop P, Lippold R, Behnecke N, Wagner W. Vergleich verschiedener implantatsysteme und deren prognose im zahnlosen unterkiefer. Deutsche Zahnartzlische Zeitung 1993;48:793-6. [ Links ]
5. Chiapasco M, Gatti C, Rossi E, Haefliger W, Markwalder TH. Implant-retained mandibular overdentures with immediate loading. A retrospective multicenter study on 226 consecutive cases. Cin Oral Impl Res 1997;8:48-57. [ Links ]
6. Donado M, Donado A, Guisado B, Ortega R, Sanz JV, eds. Anatomía implantológica. Bases morfológicas y su aplicación clínica en implantología dental. Barcelona: Ed Ars Médica; 2003. [ Links ]
7. Cano Sánchez J, Martínez-González JM, Gonzalo Lafuente JC, Cantero Álvarez M, Barona Dorado C. Superficie de los implantes dentales: estado actual. Quintessence 2004; 5:301-8 [ Links ]
8. Grunder U, Polizzi G, Goene R. A 3 year prospective multicenter follow up report on the inmediate and delayed placement of implants. Int J Oral Maxillofac Implants 1999;14:210-6. [ Links ]
9. Albrektsson T, Zarb G, Worthington P. The long-term efficacy of currently used dental implants: a review and proposed criteria of success. Int J Oral Maxillofac Impl 1986;1:11-25. [ Links ]
10. Martínez-González JM, Cano J, Campo J, Martínez MJS, García-Sabán F. Diseño de los implantes dentales: Estado actual. Av Periodon Implantol 2002;14:129-36 [ Links ]
11. Hermann JS, Cochran DL, Nummikoski PV, Buser D. Crestal bone changes around titanium implants. A radiographic evaluation of unloated nonsubmerged and submerged implants in the canine mandible. J Periodontol 1997;68:1117-30. [ Links ]
12. Isidor F. Loss of osseointegration caused by oclusal load of oral implants. Clin Oral Implants Res 1996;7:143-52. [ Links ]











 texto en
texto en