Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Medicina Oral, Patología Oral y Cirugía Bucal (Internet)
versión On-line ISSN 1698-6946
Med. oral patol. oral cir.bucal (Internet) vol.11 no.5 ago./sep. 2006
ORAL MEDICINE AND PATHOLOGY
Darier disease: case report with oral manifestations
Camila Lopes Cardoso1, Patrícia Freitas1, Luís Antônio de Assis Taveira2, Alberto Consolaro2
(1) DDS
(2) DDS, MSc, PhD, Department of Stomatology (Oral Pathology), Bauru Dental School, University of São Paulo, Bauru, São Paulo, Brazil
ABSTRACT
Darier disease, also known as keratosis follicularis or dyskeratosis follicularis, is a rare autosomal dominant genodermatosis. It is clinically manifested by hyperkeratotic papules primarily affecting seborrheic areas on the head, neck and thorax, with less frequent involvement of the oral mucosa. When oral manifestations are present, they primarily affect the palatal and alveolar mucosa, are usually asymptomatic, and are discovered in routine dental examination. Histologically, the lesions present suprabasal clefts in the epithelium with acantholytic and dyskeratotic cells represented by corps ronds and corps grains. This paper reports a case of an adult male patient presenting clinical signs of Darier disease in the palatal mucosa and skin on the neck and upper limbs. Intraoral biopsy of the affected area, analysis of family history and evaluation by a multidisciplinary team led to the diagnosis of Darier disease. Dental professionals and pathologists should be aware of these lesions to allow correct diagnosis and proper management of this disease.
Key words: Darier disease, keratosis follicularis, dyskeratosis follicularis, oral manifestation.
Introduction
Darier disease, also known as keratosis follicularis or dyskeratosis follicularis, is a rare keratinization disorder. It is an autosomal dominant genodermatosis with high penetrance and variable expressivity. Its manifestations appear in childhood and adolescence. The clinical signs are represented by several hyperkeratotic papules primarily affecting seborrheic areas on the head, neck, thorax, hand palms and foot soles, and less frequently the oral mucosa (1-6). The formation of nails is also altered, with presence of longitudinal lines or grooves and painful fissures. Associated anomalies have been described in the literature, including mental retardation and psychosis (4).
Darier disease was initially described by Prince Marrow in 1886 and simultaneously by Darier and White in 1889, independently. The first report of mucosal manifestations was described by Reenstierna in 1917(3).
The prevalence of this disorder in the population is 1:100,000, most often affecting males (1,3,7). The oral mucosa is affected in 50% of cases (2, 4), in these cases, lesions are usually asymptomatic and discovered during routine dental examination. Lesions are represented by multiple firm papules with normal, whitish or reddish color, primarily affecting the palatal and alveolar mucosa. Initially, papules are reddish and may coalesce, forming crusts that may be ulcerated.
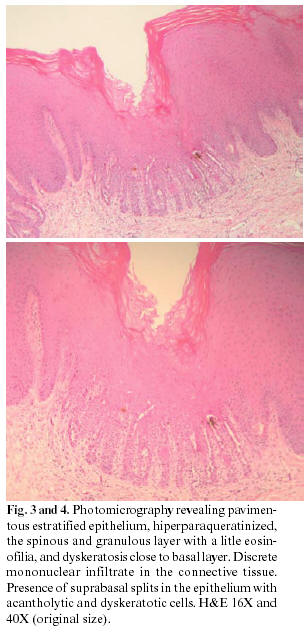
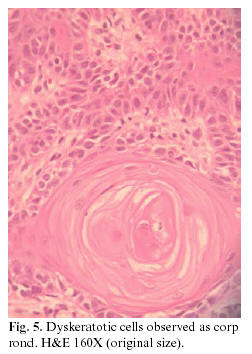
Histologically, the lesions present suprabasal splits in the epithelium with acantholytic and dyskeratotic cells observed as corps ronds and corps grains. They present many fragments of orthokeratin and parakeratin (5, 6).
This paper reports a case of a patient with Darier disease diagnosed during dental examination.
Case report
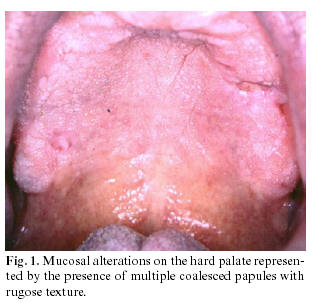
A male patient aged 35 years was submitted to routine dental examination, which revealed mucosal alterations on the hard palate with presence of multiple asymptomatic coalesced papules with rough texture and hard to palpation (Figure 1). The patient did not wear prostheses nor presented signs of inflammation. During anamnesis, the patient reported no systemic problems; however, extraoral physical examination revealed papules on the neck and upper limbs similar to those observed in the intraoral examination. The patient also reported that his daughter presented the same skin signs. With the suspicion that the lesions could be part of a systemic alteration or syndrome, the team decided to perform an intraoral biopsy of the area affected by lesions for anatomopathological examination (Figure 2).
The biopsy was compatible with keratosis follicularis or Darier disease, represented by the presence of suprabasal splits in the epithelium with acantholytic and dyskeratotic cells observed as round and granular corpuscles (Figure 3 and 4). The patient was then referred to a dermatologist for evaluation of skin alterations. Mouthrinse with antiseptic solutions was prescribed for oral hygiene and utilization of sunscreen was indicated to prevent exacerbation of skin lesions.
Microscopic confirmation associated to family history and skin alterations allowed clinical-histopathological diagnosis of Darier disease by the multidisciplinary team. The patient has been followed for 3 years for evaluation of oral and skin alterations.
Discussion
The Darier disease is a genodermatosis caused by an autosomal dominant keratinization disorder (1-6)whose etiology is poorly explained in the literature. It is believed to be related to structural disorders in cell adhesion complexes (components of desmosomes), triggering self-immune reactions among epithelial cells. More recently, it has been related to mutations in the gene encoding the sarco/endoplasmic reticulum Ca2+ ATPase pump (SERCA2), resulting in abnormal organization or maturation of complexes responsible for cell adhesion, thus leading to the disturbance (1,8-10).
Intraoral lesions primarily affect the hard palate and alveolar mucosa, and secondarily the oral mucosa and tongue (6). Macleod et al.(4) in 1991 investigated the incidence and distribution of oral lesions in 24 patients with Darier disease, among whom only 50% had oral manifestations. The palate was the most affected area in the present study, followed by the gingiva, oral mucosa and tongue, with varying severity usually following the skin signs (4). Ferris et al. observed that 30% of patients presented intermittent sialadenitis of the parotid glands (1), which is a rare condition first described in the literature by Spouge in 1966 (1,11).
Histologically, Darier disease is similar to other acantholytic diseases as Hailey-Hailey disease, Grovers disease and pemphigus vulgaris, with the common finding of suprabasal splits in the epithelium. However, cell necrosis is more frequent in pemphigus vulgaris and rarer in Hailey-Hailey and Darier diseases. Clinical signs are also different for each disorder (7).
Clinically, moderate forms of the disease are similar to nicotine stomatitis and severe forms are similar to inflammatory fibrous hyperplasia. Thus, smokers and individuals wearing complete dentures should undergo biopsy for final diagnosis. Warty dyskeratoma is histologically similar to Darier disease; however, this is a rare and isolated lesion that affects only mucosa or only skin, thus being classified as an isolated form of Darier disease by some authors (3,6).
The implications of the Darier disease are more associated with cosmetic and esthetic than functional implications, since this is a benign dermatosis. However, depending on the severity of the disease and affected area, the patient has more complaints and the emotional status may be damaged by esthetic reasons.
The systemic treatment of the Darier disease is symptomatic. The lesions relapse because of the hereditary etiopathogenesis, especially in patients with the severe and generalized form of the disease, who are usually treated with systemic and topical retinoids and in whom oral lesions still persist (4).
Thus, therapies mentioned in the literature have a cosmetic goal, aiming at improving the patients quality of life with regard to esthetics and especially hygiene, which may be improved in the oral cavity by utilization of non-alcoholic mouthrinses, since the coalescence of papules in skin or mucosa leads to accumulation of organic products (keratin degraded by bacteria), which causes a bad odor and favors the accumulation of microorganisms, producing secondary infection. Some authors mention that these complications are worsened by heat (2,6).
Several treatments have been presented in the literature, such as utilization of topical retinoids, steroids and antibiotics; however, they provide limited benefits (6). Medical therapy includes utilization of systemic retinoids due to their efficacy; however, they should be carefully described by the medical doctor. More radical treatments have been reported, including surgical excision, abrasion, application of carbon dioxide and laser (9). Photodynamic therapy has been also considered; however, authors believe that it should not replace systemic retinoids in patients requiring systemic treatment (9). Utilization of topical 1% vitamin A acid is advocated in dyskeratoses, yet favorable outcomes have not been reported (2).
Regardless of the clinical severity and treatment option, the patient should receive genetic counseling with information on the inherited condition and risk of transmission to the offspring. Most often, dental doctors diagnose the oral manifestations in routine examinations before medical doctors, since lesions are asymptomatic. Biopsy is fundamental to allow final diagnosis; based on this result, the patient should be referred to dermatological examination.
Patients should be informed on the complications of this disorder and the care required. The emotional status in more severe cases should be followed by a psychologist; therefore, these patients should be treated by a multidisciplinary team.
References
1. Ferris T, Lamey PJ, Rennie JS. Dariers disease: oral features and genetic aspects. Br Dent J 1990;168:71-3. [ Links ]
2. Tommasi, AF, eds. Diagnóstico em patologia bucal. São Paulo: Pancast Editora; 2002. p. 455. [ Links ]
3. Prindiville DE, Stern D. Oral manifestations of Dariers disease. J Oral Surg 1976;34:1001-6. [ Links ]
4. Macleod RI, Munro CS. The incidence and distribution of oral lesions in patients with Dariers disease. Br Dent J 1991;171:133-6. [ Links ]
5. Weedon D, eds. Skin Pathology . London; New York: Churchill Livingstone; 2002. p.296. [ Links ]
6. Neville BW, Damm DD, Allen CM, Bouquot JE, eds. Patologia Oral & Maxilofacial. Rio de Janeiro: Guanabara Koogan; 2002. p. 625-6. [ Links ]
7. Jalil AA, Zain RB, van deer Wall I. Darier disease: a case report. Br J Oral Maxillofac Surg 2005;43:336-8. [ Links ]
8. Kimoto M, Akiyama M, Matsuo I. Dariers disease restricted to sun-exposed areas. Clin Exp Dermatol 2004; 29:37-9. [ Links ]
9. Exadaktylou D, Kurwa HA, Calonge E, Barlow RJ. Treatment of Dariers disease with photodynamic therapy. Br J Dermatol 2003;149:606-10. [ Links ]
10. Sehgal VN, Srivastava G. Dariers (Darier-White) disease/keratosis follicularis - review. Int J Dermatol 2005; 44:184-92. [ Links ]
11. Spouge JD, Trott JR, Chesko G. Darier-Whites disease. A cause of white lesions of the mucosa. Oral Surg 1966; 21:441-57. [ Links ]
![]() Address for correspondence:
Address for correspondence:
Prof Dr Luís Antônio de Assis Taveira
Disciplina de Patologia, Faculdade de Odontologia de Bauru - USP
Rua Alameda Octávio Pinheiro Brisolla 9-75
Bairro Vila Universitária
Bauru, SP, Brazil
CEP 17012-901
Email: lataveir@fob.usp.br
Received: 21-01-2006
Accepted: 6-05-2006