My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Medicina Oral, Patología Oral y Cirugía Bucal (Internet)
On-line version ISSN 1698-6946
Med. oral patol. oral cir.bucal (Internet) vol.11 n.6 Nov./Dec. 2006
Topic tacrolimus, alternative treatment for oral erosive lichen planus resistant to steroids: A case report
Tacrolimus tópico, tratamiento alternativo para liquen plano erosivo de mucosa resistente a corticoides: A propósito de un caso
Ana Riaño Argüelles 1, Raúl Martino Gorbea 2, María Eugenia Iglesias Zamora 3, Joaquín Garatea Crelgo 2
(1) Medical Assistant. Maxillofacial Surgery. Virgen del Camino Hospital
(2) Maxillofacial Surgeon. Virgen del Camino Hospital
(3) Dermatologist. Navarra Hospital. Pamplona
ABSTRACT
The lichen planus is a mucocutaneous disease with unknown etiology and auto-immune pathogenia. There have been three variants of lichen planus: the reticular, the plaque-like and the atrophic-erosive lesions. Its a chronic disease with acute relapses that generally affects more frecuently to women from the fourties. The diagnostic is based on the clinic identification of the lesions joined with the histopathologic study (basal cells hidropic degeneration, linfoplasmocitic infiltration and absence of displasy signs). The great number of therapeutic options are explained for its high prevalency (0.5-2%), its recurrence and its risk for malignant transformation.
We present a case of oral erosive lichen planus, refractory to numerous treatments, mainly corticosteroids. During 15 days the lesion responded to the administration of a 0.1% tacrolimus in topic application. This article tries to show the new indication of tacrolimus, a calcineurin inhibitor immunosuppressor, that it is effective in the erosive lesions treatment.
Key words: Oral erosive lichen planus, oral topic tacrolimus.
RESUMEN
El liquen plano es una enfermedad mucocutánea de etiología desconocida y patogenia autoinmune. Existen tres variantes de liquen plano: la forma reticular, la forma en placas y la forma atrófico-erosiva. El curso es crónico con frecuentes reactivaciones. Afecta con más frecuencia a mujeres en la 4ª década de la vida y superiores. El diagnóstico se basa en la identificación clínica de las lesiones junto a el estudio histopatológico (degeneración hidrópica de la capa basal, infiltrado de linfo-plasmocitario y ausencia de signos de displasia). Su alta prevalencia (0,5-2%), su carácter recurrente y el potencial riesgo de transformación maligna explican el gran número de opciones terapéuticas disponibles.
Presentamos un caso de liquen plano erosivo, de mucosa oral, resistente a múltiples tratamientos, fundamentalmente corticoideos. En el plazo de 15 días respondió a la administración de tacrolimus al 0,1% en aplicación tópica. El artículo pretende señalar la indicación novedosa del principio activo tacrolimus, un inmunosupresor inhibidor de la calcineurina, que se ha demostrado eficaz en la solución de las lesiones erosivas.
Palabras clave: Liquen plano erosivo oral, tacrolimus tópico oral.
Introduction
The lichen planus is a chronic disorder with unknown etiology that affects from 0.5 to 2% of the population (1). It frequently appears in patients in the age range from 30 to 70 years old. In 52 for 80% of the cases these patients are women (2).
Its pathogenia is autoimmune mediated for T-cells that attacks the mucosa basal cells and/or skin by retarded hypersensibility mechanism (1).
The oral form is more frecuently, resistant and persistent than the cutaneous one. The main oral localizations are the buccal mucosa, tongue and joined gum. There are three recognized varieties of lichen planus that, according to an increased order in gravity and symptomatology, are: the reticular, the plaque-like and the atrophic-erosive lesions.
The classic therapeutic management of erosive lichen planus is based on the topic application or intralesional injection of corticosteroids. As immunosuppressor agent is also used cyclosporine. Other alternatives to the treatment are creams based on retinoids (vitamin A), anti inflammatories o antipruritics. Lidocain mouthwashes may numb the area temporarily. Ultraviolet light therapy may be beneficial in some cases.
Clinical case
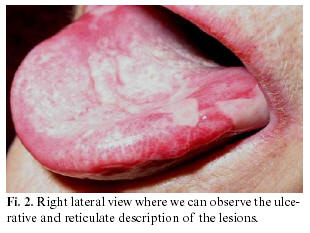
Patient, woman, 68 years old. She was remitted to our consultation because she presented two years old ulcerative lesions, with reticulated aspect, on the lateral border of the tongue (figure 1 and 2). These lesions were very painful and produced a weight loss of 10 kg. since she wasn´t able to eat or use her dental prosthesis normally. She also had minor ulcerative lesions on the superior lip and genital mucosa. The patient, as a personal antecedent, had hepatitis C for 12 years old.
We practised a biopsy over the ulcerative area. The biopsy was reported as an unspecified ulcer although it was observed a band-like linfocitic infiltration, epithelial covered loss and ampouled lesion absence in the cuts by congelation. The immunofluorescent study resulted negative as well as anti-substance intercellular antibodies.
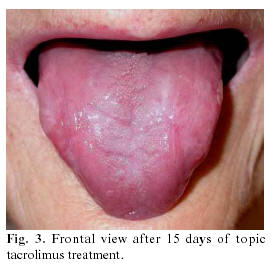
Based on the clinical aspect of the lesion, that it had a suspected erosive lichen, we started a treatment with topic costicosteroids (0,1% triamcinolone acetonide ointment 2 applications/ 12 hours). No clinical improvement was achieved. Then we consulted the case with the Dermatology Department that ratified the clinical diagnosis and, using their experience in the treatment of these lesions, they decided to establish a therapy with 0.1% topic tacrolimus cream, 1 application/day and night. The clinical and macroscopic improvements at 15 days treatment beginning are evident (figure 3 and 4). Because of the good response to the treatment, and after many chases in the consultation, it was decided to maintain the therapy another month and a half, in a continuous way. After this time, another outbreak emerged but it was reduced in five days. She remained asymptomatic throughout the three-month period.
However, the patient didnt tolerate the 0.1% tacrolimus treatment on her genital lesions and it was necessary to reduce the posology to the 0.03% tacrolimus.
Discussion
The patients affected for lichen planus frecuently exceed the 40 years old and, according to clinical studies, from 50 to 80% of the cases are women (2). The more frecuently localizations are buccal mucosa, tongue and joined gum (in its vestibular way). As predisposed factors of lichen planus there were implicated numerous associations of histocompatibility antigens, mainly the HLA-DR type that produced a more intense band-like infiltration (2). The symptoms are increased with emotional stress, chemicals or medications including (gold, non steroid anti-inflammatories) and many others.
The most accepted pathogenic mechanism is based on the basal cell induction by unknown factors (tissular damage, drugs, γ interferon produced by non-specific activated lymphocytes ). After this stimulus, the basal cells start a class II antigen production (type HLA-DR), that normally they dont have interacting with lymphocytes as a Langerhans cell. In this way a cell mediated autoimmunity reaction is started (3). The immunopathogenic hypothesis achieved great importance when we discover a frequently association between lichen planus and other autoimmune processes (myasthenia gravis, Sjögren syndrome, ulcerous colitis ).
Likewise it has been described cases of association between lichen planus and hepatic diseases, in some cases with hepatitis C, even though it doesnt exist a significant statistic correlation (3). Although the viral genome in the epithelium of the patients affected for lichen planus cant be detected, it seems to act as indirect way altering the percentage of lymphokynes (increases the percentage of TNF-a and reduced the IL-1, INF-γ e IL-8) (4).
Recent studies (5) explain the relation between the psychological situation of the patient and the lichen planus lesions, that is usually observed in the daily clinical practice. When a psychological alteration is present, a significant stadistic increased number of linfocites T CD4+ exists, joined to a high tendency of suffering atrophic-erosive lesions. According to this study, it can be suggested a pathogenic model in which the psychological alteration produced an impact over the neuroendocrinous system, that would influence over the linfocites subpopulations.
Some authors describe a possible implication of the lipid metabolism in the pathogenia and evolution of the oral lichen planus lesions, since there are significant stadistic differences in the cholesterol and VLDL rates between patients suffering lichen planus and healthy volunteers (6).
The erosive form, case of this article, is the variant with more symtomatology and the second in order of frequency behind the reticular form. It produces ulcers over a erythematosus lesion with some hyperkeratosis focus. Due to the mucosa basal cells destruction it is possible to find blister formation and the appearance of Nikolsky + sign. Our patient explained a regular descamative evolution of her lesions, perhaps due to this failure in the basal cells support.
The diagnosis is clinic and it must be confirmed by biopsy. The biopsy will be more significative if it is done in an eritematous zone instead of in the nucleus of the ulcer, because the epithelial layers have been lost in this area and a secondary inflammation is existed. The histologic study of the biopsy will observe a superficial and fine epithelium joined to a connective tissue thanks to a fine basal layer that shows hydropic degeneration because of the cytotoxic effect of the T cells over the basal cells. These fine epithelium areas alternate with others, denudated, where the epithelium has disappeared and it only has seen a vascular connective tissue and a profuse inflammatory infiltrated of lympho-plasmocytic cells (7). The immunofluorescence isnt useful in these cases because it hasnt been implicated auto antibodies.
Its necessary to realize a differential diagnosis between the erosive form and the erythroplasia as a clinic translation of a dysplasia. The lichen planus has been considered as a premalignant lesion. The malignant transformation into a squamous carcinoma occurs from 1 to 3 % of the cases, above all when the lesion is located on the tongue. Other similar diseases are: penphigoid, pemphigus vulgaris, chronic ulcerative stomatitis and even chronic candidiasis (8).
The treatment of this pathology is varied. The principal goal is to reduce the symptoms and secondary the total o partial extinction of the lesion. Although traditional treatment is based on immunosuppressor therapy with topic or injected corticosteroids on the lesion, there isnt a main therapeutic group because of the variety in the response of each patient. Other treatment options are the cyclosporine, vitamin A analogues, topic anti-inflammatories applications. Understanding the pathogeny its easy to understand the high rate of recurrence of this disease.
In lesions resistant to this conventional therapy, as is this case, it has been described the benefits of 0.1% topic tacrolimus. The posology varies from one to four times a day (9-11) according to different studies. Tacrolimus is caused by the Streptomyces tsukubaensis (12) and belongs to the macrolid family. It has an immunosuppressor action similar to the cyclosporine although it penetrates deeply on the mucosa and its from 10 to 100 times more potent that this (1). It inhibits the first step of the T lymphocytes activation, since it fixes to the immunophilin, the FKBPB 12, forming a complex inhibitor to the calcineurins phosphatase. This enzyme catalyses a critic un-phosphorilation for the transcription of various lymphokynes (IL-2, IL-3, IL-4 ). These cytokines activate the T and B lymphocytes. When the levels of T cells activators decrease proliferation answers cells against the antigens and mitogens also decreased.
The topic tacrolimus is an active principle of proved efficacy in the resistant atopic dermatitis treatment. Recently its used for lichenoid lesions in oral topic way although this application isnt recognized by the fabricant. In this sense, tacrolimus must be prescribed as a "compassionate use" standing for the use of a drug in a few patients, for new indications, without a clinical test when the doctor considers essential its use.
The symptoms decrease in the first month of tacrolimus treatment. The recurrences start form 6 to 12 months after the suspension of treatment although these cases seem to be less resistant to the conventional therapy. If we look up different studies about efficacy and security of long tacrolimus treatment (9), we can conclude that after the 0.1% tacrolimus application twice a day during 8 weeks a 94% of the patients experiment clinical improvement. Although during the first 8 weeks, an optimal control of the syntomathology is achieved, its necessary to continue with the treatment, in an intermittent way, to achieve the remission. Tacrolimus treatment is revealed as an effective and secure alternative due to its low systemic absorption (9) and the low incidence and importance of its secondary effects. Among the undesirable effects, we must mention the burning sensation on the application area (16%), transitory alteration of taste (8%) and reverse pigmentation of the treaty area (due to an increase in the melanocytes number and the melanogenesis) (9, 13). The unique effect not related to the application site is the intermittent migraine in the 4% of the treated patients (9). A lot of secondary effects, that not exceed the 1% of frequency, can be related to the skin application /alopecia, ALT and AST increased, anaphylactic reaction, pneumonia, depression ).
Several publications associate the topic tacrolimus treatment with an increased risk of lymfoproliferative disorders or skin tumours. Taking into account the information from the pharmacological industry (protopic®), the existence of animal studies in this matter is checked. A carcinogenetic study of dermal effect of 0,03 to 3% of tacrolimus over mousses during 104 weeks, concluded that there arent statistical differences in the skin tumour incidence but in pleomorphic lymphoma and skin undifferentiated tumours, when the application doses are maximum. There arent studies about the effects over pregnancy or lactation although its known that tacrolimus goes through the placenta and maternal milk, causing hypercalcemia and renal dysfunction in the foetus. Its use in these patients must be clinically justified and it must be sure that the benefits surpass the potential foetus risk (14).
Recent articles (12) are in favour of the pimecrolimus use belonging to the same family of the tacrolimus but it has a less firm union to the FKBPB 12 protein than the second. For this reason, the burning sensation is minor than the tacrolimus one. The use of photodynamic therapy to the oral lichen planus is more recent. It consists in the application of methylene blue into the lesion. Secondary the inflammatory cells pick up it and then its applied a determinate wave length over the lesion that induces an apoptosis of these cells (15).
Therefore, in a high prevalent pathology such as lichen planus with potential malignant transformation, tacrolimus can be offered as an alternative, safety and secure therapy to be considered when the lesions are resistant to the conventional treatment.
References
1. Edwards PC, Kelsch R. Oral Lichen Planus: Clinical presentation and Management. J Can Dent Assoc 2002;68:494-9. [ Links ]
2. Bagán Sebastián JV, Cerero Lapiedra R. Liquen plano oral. En: Bagán Sebastián JV, Ceballos Salobreña A, Bermejo Fenoll A, Aguirre Urízar JM, Peñarrocha Diago M, eds. Medicina Oral. Barcelona: Masson;1995. p. 202-19. [ Links ]
3. Bagán JV, Aguirre JM, del Olmo JA, Milián A, Peñarrocha M, Rodrigo JM, et al. Oral lichen planus and cronic liver disease. A clinical and morphometric study of the oral lesions in relation to transaminase elevation. Oral Surg 1994;78:337-42. [ Links ]
4. Femiano F, Scully C. Functions of the cytokines in relation oral lichen planus-hepatitis C. Med Oral Patol Oral Cir Bucal 2005;10:E40-4. [ Links ]
5. Gandara Rey J, García García A, Blanco Carrion A, Gandara Vila P, Rodriguez Nunez I. Cellular inmune alterations in fifty-two patients with oral lichen planus. Med Oral 2001;6:246-62. [ Links ]
6. Blanco A, Gandara JM, Rodriguez A, Garcia A, Rodriguez L. Biochemical alterations and their clinical correlation to oral lichen planus. Med Oral 2000;5:238-49. [ Links ]
7. Bagán Sebastián JV, Jiménez Soriano Y, Milián Masanet MA. Liquen plano oral. En: Bermejo Fenoll A, eds. Medicina bucal. Madrid: Editorial Síntesis; 2000. p. 198. [ Links ]
8. Marx RE, Stern D. Immune-Based Diseases. En: Marx RE, Stern D, eds. Oral and maxillofacial pathology: a rationale for diagnosis and treatment. Hong-Kong:Quintessence Books; 2003. p. 156-62. [ Links ]
9. Hodgson TA, Sahni N, Kaliakatsou F, Buchanan JA, Porter SR. Long-term efficacy and safety of topical tacrolimus in the management of ulcerative/erosive oral lichen planus. Eur J Dermatol 2003;13:466-70. [ Links ]
10. Olivier V, Lacour JP, Mousnier A, Garraffo R, Monteil RA, Ortonne JP. Treatment of chronic erosive oral lichen planus with low concentrations of topical tacrolimus: an open prospective study. Arch Dermatol 2002;138:1335-8. [ Links ]
11. Kaliakatsou F, Hodgson TA, Lewsey JD, Hegarty AM, Murphy AG, Porter SR. Management of recalcitrant ulcerative oral lichen planus with topical tacrolimus. J Am Acad Dermatol 2002;46:35-41. [ Links ]
12. Swift JC, Rees TD, Plemons JM, Hallmon WW, Wright JC. The effectiveness of 1% pimecrolimus cream in the treatment of oral erosive lichen planus. J Periodontol 2005;76:627-35. [ Links ]
13. Fricain JC, Sibaud V, Campana F, Lepreux S, Taïeb A. Mucosal pigmentation after oral lichen planus treatment with topical tacrolimus. Dermatology 2005;210:229-32. [ Links ]
14. Astellas Pharma.org (homepage on the internet). United States: Focus on protopic (tacrolimus). Full prescribing information. Healthcare Professionals.c.2005. Available from: http://www.protopic.com/physician/facts.html. [ Links ]
15. Aghahosseini F, Arbabi-Kalati F, Fashtami LA, Fateh M, Djavid GE. Treatment of oral lichen planus with photodynamic therapy mediated methilene blue: a case report. Med Oral Patol Oral Cir Bucal 2006;11:126-9. [ Links ]
![]() Correspondence:
Correspondence:
Dra. Ana Riaño Argüelles
Plaza Rafael Alberti nº 9 1º C
31010 Barañain (Navarra)
E-mail: anara_teverga@hotmail.com
Received: 9-10-2005
Accepted: 3-06-2006