Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Medicina Oral, Patología Oral y Cirugía Bucal (Internet)
versión On-line ISSN 1698-6946
Med. oral patol. oral cir.bucal (Internet) vol.11 no.6 nov./dic. 2006
Benign cementoblastoma: A case report
Mahmut Sumer 1, Kaan Gunduz 2, A. Pinar. Sumer 2, Omer Gunhan 3
(1) Ondokuz Mayis University, Faculty of Dentistry, Department of Oral and Maxillofacial Surgery, Samsun, Turkey
(2) Ondokuz Mayis University, Faculty of Dentistry, Department of Oral Diagnosis and Radiology, Samsun, Turkey
(3) Department of Pathology, GATA, Ankara, Turkey
ABSTRACT
In the past the benign cementoblastoma was recognized in the World Health Organizations classification of odontogenic tumours as one of the cementoma neoplasias. Recently the benign cementoblastoma is included into Mesenchyme and/or odontogenic ectomesenchyme, with or without odontogenic epithelium odontogenic tumours. Benign cementoblastoma has characteristic radiologic and microscopic features and it appears to be fused to the tooth roots. Symptoms may be totally absent, and when they do occur, pain and swelling are frequent findings. The final diagnosis is usually made histopathologically, but the clinical diagnosis is comparatively easy if it is examined radiographically. The tumour has unlimited growth potential. Most frequently tends to be associated with an erupted permanent tooth, most often the first molar: rarely has an association with an impacted or partial impacted tooth been reported. This case represents a case of benign cementoblastoma associated with a partially impacted mandibular third molar.
Key words: Benign cementoblastoma, odontogenic tumour, partially impacted.
Introduction
The benign cementoblastoma is a relatively rare odontogenic neoplasm of the jaws and was first described by Dewey (1) in 1927. The lesion is considered as the only true neoplasm of cementum origin (2). The benign cementoblastoma, which generally occurs in young persons, comprises less than 1% to 6.2% of all odontogenic tumours (2) and is characterized as being attached to the roots, most frequently tends to be associated with an erupted permanent tooth, most often the first molar or second premolar in the lower jaw: only rarely has an association with an impacted or partially impacted tooth been reported (3).
Symptoms may be totally absent, and when they do occur, pain and swelling are frequent findings (3-5). The final diagnosis is usually made histopathologically, but the clinical diagnosis is comparatively easy if it is examined radiographically. The tumour has unlimited growth potential (3-6). The recommended treatment is complete enuclation of the tumor mass with extraction of the involved tooth (2-6).
This case report describes a benign cementoblastoma that attached to the lateral portion of the root of the partially impacted mandibular third molar; treatment included surgical excision of the lesion.
Case report
A 46-year-old male presented complaining of pain, trismus and swelling in the left third molar area for a period of 2 months. His medical and family history was noncontribibutory. There was no reported history of orafacial trauma. The clinical examination revealed acute pericoronitis involved with a partially impacted left mandibular third molar with swelling of the overlying mucosa. Also there was a slight expansion of bone on the buccal side of the mandible. A panoramic radiography is taken for radiological examination. The panoramic radiograph revealed a 20 mm, radiopaque mass attached to the lateral portion of the root of the lower left third molar that was surrounded by a radiolucent periphery (Figure 1).
After the symptoms improved with treatment with antibiotic and anti-inflammatory agents, enucleation of the calcified mass with the extraction of the tooth involved was performed under local anesthesia. The wound was irrigated and closed. Soft tissue healing was complete by 3 weeks. Eleven-month follow up shows no evidence of recurrence.
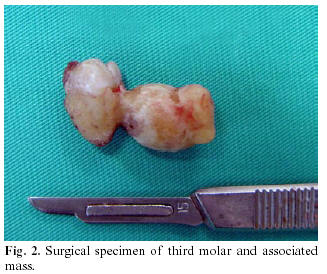
Macroscopically, a hard ovoid mass of calcified material measuring 20 x 10 x 10 mm, attached to the lateral portion of the root of the mandibular third molar (Figure 2). Radiographs and macroscopic appearance led to diagnose the lesion as a cementoblastoma. The surgical specimen was sent for pathologic examination.
Histopathologic examination showed dens, irregularly lamellated, osteocementum-like material with lack of interstitial tissue. A diagnosis of benign cementoblastoma was made (Figure 3).
Discussion
In the past the benign cementoblastoma was recognized in the World Health Organizations classification of odontogenic tumours as one of the cementoma neoplasias (3). Recently the benign cementoblastoma is included into Mesenchyme and/or odontogenic ectomesenchyme, with or without odontogenic epithelium odontogenic tumours (7). The lesion derives from mesenchymal tissue, although its aetiology is unknown (4,5).
Benign cementoblastomas are predominantly seen in young persons. Ulmansky et al. (3), has reviewed literature and reported that close to three quarters of the patients (73%) are under the age of 30. Although it has been reported that there is no significant sex predilection between two sexes (8, 9) some authors (10, 11) indicates that males are affected more frequently than females. The mandible is involved more often than the maxilla (2-6, 8-11). The tumour usually involves an erupted permanent tooth. The most commonly affected tooth is the first permanent molar (2). The benign cementoblastoma rarely has an association with a partially impacted third molar tooth like in this case.
The lesion is slow growing and usually asymptomatic; however, pain and swelling have been reported in a number of cases including the one presented in this article. Cortical expansion and facial asymmetry are common (4-6, 8, 9).
Radiographically, the lesion usually shows a radiopaque mass often fused with a root or roots of a tooth and surrounded and limited peripherally by a radiolucent halo. When the intimate relation with roots is present, the radiographic appearance is nearly pathognomonic (3). The present case providing this parameter had this characteristic. Few authors have reported a more radiolucent form of the lesion and considered it to represent an early uncalcified matrix stage (12).
There are a few lesions which should be distinguished from this lesion such as osteoma, benign osteoblastoma, chronic focal sclerosing osteotitis, osteomyelitis and osteosarcoma, etc (3-5, 6, 9, 14). Clinical and especially radiological findings are helpful for differential diagnosis. Sometimes the general appearance of the lesion is very similar with osteoma or osteoblastoma. Microscopic differential diagnosis between cementoblastoma and osteoblastoma, the direct connection with the radicular surface is the most significant finding (13).
Because benign cementoblastoma has unlimited growth potential, the usual treatment is complete surgical excision with extraction of the associated teeth. In literature, there are 13 recurrent cases associated with cemetoblastomas. Extraction of the involved tooth or teeth along with removal of the lesion was performed in 9 of the 13 recurrent cases. Four cases were treated with curettage only without extraction of the involved tooth. Recommended treatment of cementoblastoma should consist of removal of the lesion along with the affected tooth or teeth, followed by thorough curettage or peripheral ostectomy (8). In our case, there has been no recurrence more than 11 months after the surgical procedure.
The benign cementoblastomas usually involve an erupted permanent tooth and most commonly found in the patients younger than 30 year old. In this case report; a case of benign cementoblastoma of a 46-year-old male is presented involving a mandibular semi-impacted third molar and arising from the lateral portion of the root of the involved tooth which had a very characteristic macroscopic appearance.
References
1. Dewey KW. Osteoma of a molar. Dent Cosmos 1927; 69:1143-9. [ Links ]
2. Lu Y, Xaun M, Takata T, Wang C, He Z, Zhou Z, et al. Odontogenic tumours. A demographic study of 759 cases in a Chinese population. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1998;86:707-14. [ Links ]
3. Ulmansky M, Hjorting-Hansen E, Praetorius F, Haque MF. Benign cementoblastoma; a review and five new cases. Oral Surg Oral Med Oral Pathol 1994;77:48-55. [ Links ]
4. Piattelli A, Di Alberti L, Scarano A, Piattelli M. Benign cementoblastoma associated with an unerupted third molar. Oral Oncol 1998;34:229-31. [ Links ]
5. Piatelli A, Daddona A, Piatelli M. Benign cemento-blastoma: Review of the literature and report of a case at unusual location. Acta Stomatol Belg 1990;87:209-15. [ Links ]
6. Cundiff J. Developing cementoblastoma: Case report and update of differential diagnosis. Quintessence Int 2000; 31:191-5. [ Links ]
7. Barnes L, Eveson JW, Reichart P, Sidransky D, eds. Pathology & Genetics: Head and Neck Tumours. Geneva: WHO; 2005. [ Links ]
8. Brannon RB, Fowler CB, Carpenter WM, Corio RL. Cementoblastomas: an innocuous neoplasm.? A clinicopathologic study of 44 cases and review of the literature with special emphasis on recurrence. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2002;93:311-20. [ Links ]
9. Regezi JA, Sciubba JJ, eds. Oral pathology: Clinical-pathological correlations. Philadelphia: Saunders; 1989. p. 359-61. [ Links ]
10. Ohki K, Kumamoto H, Nitta Y, Nagasaka H, Kawamura H, Ooya K. Benign cementoblastoma involving multiple maxillary teeth: report of a case with a review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2004;97:53-8. [ Links ]
11. Monks FT, Bradley JC, Turner EP. Central osteoblastoma or cementoblastoma? A case report and 12-year review. Br J Oral Surg 1981;19:29-37. [ Links ]
12. Gingell JC, Lunin M, Beckerman T, Levy BA. Benign cementoblastoma. J Oral Med 1984;68:8-11. [ Links ]
13. Fujita S, Takahashi H, Okabe H, Watanabe C, Sonobe H. A case of benign cementoblastoma. Oral Surg Oral Med Oral Pathol 1989;68:64-8. [ Links ]
14. Junquera-Gutierrez L, Lopez-Arranz JS, Albertos-Castro JM, De Vicente-Rodriguez JC. Odontogenic tumors: classification. clinical features. diagnosis and treatment. Med Oral 1997;2:94-101. [ Links ]
![]() Correspondence:
Correspondence:
Dr. Kaan Gunduz
Ondokuz Mayis Universitesi,Dişhekimliği Fakültesi
Oral Diagnoz ve Radyoloji Anabilim Dali
55139 Kurupelit, Samsun Turkey
E-mail: kgunduz@omu.edu.tr
Received: 21-03-2006
Accepted: 16-06-2006