Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Medicina Oral, Patología Oral y Cirugía Bucal (Internet)
versión On-line ISSN 1698-6946
Med. oral patol. oral cir.bucal (Internet) vol.12 no.1 ene. 2007
Mandibular ameloblastoma. Reconstruction with iliac crest graft and implants
Javier Mareque Bueno1, Santiago Mareque Bueno2, Jorge Pamias Romero 3,
Mª Socorro Bescos Atín 3, Pedro Huguet Redecilla 4, Guillermo Raspall Martin 5
(1) Trainee Oral and Maxilofacial Surgery. Vall d´Hebrón Hospital. Barcelona
(2) Dentist. Fellow Periodontics NYU
(3) Faculty Oral and Maxilofacial Surgery. Vall d´Hebrón Hospital. Barcelona
(4) Faculty Pathology Unit. Vall d´Hebrón Hospital. Barcelona
(5) Head of Oral and Maxilofacial Surgery Unit. Vall d´Hebrón Hospital. Barcelona
ABSTRACT
The ameloblastoma is a bening odontogenic tumor. The treatment planning in young persons is still not clear. We describe a case report of a young boy who was treated in our unit and we review the different aproaches for this type of lesions, which nowadays still not clear in this patients.
Key words: Ameloblastoma, reconstruction, young.
RESUMEN
El ameloblastoma es un tumor odontogénico benigno.El plan de tratamiento en pacientes jovenes sigue siendo controvertido. Describimos un caso clinico de un varón joven tratado en nuestro servicio y revisamos los diferentes enfoques de este tipo de lesiones, que a dia de hoy sigue sin estar claramente definido.
Palabras clave: Ameloblastoma, reconstrucción, jóvenes.
Introduction
The mandibular ameloblastoma is a bening odontogenic tumor that develops from the remaining components of the enamel organ (Epithelial rests of Mallasez), originally described by Falkson in 1879. Later on, Mallasez introduced the term "adamantioma" and Churchill finally named it in 1934 as it is known nowadays (1).
It is a slow growing, locally aggressive tumor capable of causing facial deformity. It has a high recurrence rate due to its capacity to infiltrate trabecular bone. Malignant forms metastise occasionally (2).
They are only 1% of the tumors in he Maxillofacial field (3), but it is the most common odontogenic neoplasia (4). Most of the cases are localized in the angle and the body of the mandible, and are seldom found in the maxilla, where their prognosis is much worse because of greater infiltration in trabecular bone in this anatomic location.
There are 6 histologic subtypes: folicular, plexiform, acantomatos, granulose cells, basal cell and desmoplásic. They can be found combined or isolated and that are not related to prognosis of the tumor. There are also three different macroscopic subtypes: solid or multiquístic, uniquístic and periferic This classification may have a prognostic value (5).
It normally presents after the age of 20 in the case of the solid ameloblastoma, and before the age of 30 in the case of unicystic ameloblastoma. A difference of 20 years exists in the peak of incidence.
Case report
A 19 year old male presents to our center after biopsy consistent with great mandibular ameloblastoma. A FNA was performed that showed no malign or atypical cells.
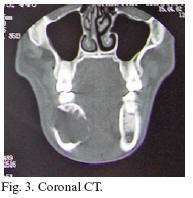
An orthopantomography (fig. 1) and a CT scan were performed (figs 2, 3) where diagnosis of cystic lesion consistent with ameloblastoma that perforated both lingual and buccal corticals in the left mandibular side with displacement of the dental nerve to the most caudal part of the lesion. It extended from tooth 28 to tooth 31.
Resection of the lesion was performed under general anaesthesia. The macroscopic characteristics of the lesion were consistent with unicystic ameloblastoma. The lingual margin of the lesion did not have a clear osseous limit due to perforation of the lingual cortical at this site. The inferior alveolar nerve could be freed. It had been rejected to a caudal position. Extraction of teeth 3.7 to 3.4 and tumor was removed.
A reconstruction plate was fixed in order to reinforce and to help to stabilize an onlay iliac crest bone graft placed in conjunction with rich platelet plasma (RPP) and a fibrin membrane.
The results of the histopathologic study were unicystic follicular ameloblastoma with partial cystic transformation, without atypical or malign cells, free margins, medial zone without security margin (fig 4).
A control postoperative CT scan was performed four months after surgery, confirming consolidation of the graft. A new Ct scan was performed 8 months postsurgery confirming complete integration of the graft without recurrence (figs 5).
Reentry is performed at 12 moths after first surgery for retrieval of the reconstruction plaque and placement of 4 Branemark implants in position of 28 to 31. Primary stability was achieved (fig 6). Second stage surgery was performed at 6 months. Healing caps were placed, impressions were taken, and a provisional prosthesis was prepared by the laboratory. Figure 6 shows the result of the rehabilitation.
After more than 2 years of radiological follow up there is no evidence of recurrence. A low-morbidity surgery has been performed with an optimal prosthetic rehabilitation that offers a good quality of life. Follow up must be performed once a year up to 10 years.
Discussion
The therapeutic approach to the ameloblastoma is still a controversy. There are problems to determine incidence, management or recurrence rate. Not every ameloblastoma has the same destructive potential or recurrence tendency (6).
The possibility of predicting recurrence of an ameloblastoma prior to surgery would permit adjustment of the treatment plan for each case (7). Thus, recurrence could be decreased without increasing morbidity of the surgery and extension of mandibular resection. However, there seems to be more consensus in the management of ameloblastomas in children, due to the psychological impact of an aggressive resection, and its relationship with growth and function. A more conservative approach is normally considered for this type of cases.
The determinants of the biologic behaviour are (8):
1 Location: 75% in the mandible, but worse prognosis in the maxilla due to spongier bone that facilitates dissemination of the tumor. There is an absence of the "contention effect" that provides the mandibular cortical bone.
2 Arquitectonic pattern: of the lesion does have a prognostic validity. Unicystic and periferic have a better prognosis than multicystic or solid.
The histological patterns have no prognostic validity, except for unicystic subtypes.
The uncystic ameloblastoma usually presents between 16 and 20 years of age, and the multicystic ameloblastoma after 30 years of age (9). Generally, the unicystic ameloblastoma presents an unilocular image associated to a third molar (10) severely displaced and occasionally presents a multilocular image in the premolar area. Unicystic ameloblastomas have been shown to have less recurrence (15-48%).
Histologically, it presents cystic characteristics delimited by a layer of ameloblastic epithelium. There are three types of unicystic ameloblastomas: intraluminal, plexiform (where enucleation is considered the treatment indicated) and mural, that requires marginal resection because of aggressive behaviour and higher recurrence rate (11, 12).
The multilocular image in this case could be consistent with a solid ameloblastoma. However, a conservative approach was chosen due to age of the patient and macroscopic appearance of the lesion. Thus, excision of the lesion and its margins was performed (12).
This option was selected instead of a more aggressive choice indicated in case of recurrence of the tumour (11).
References
1. J. Philip Sapp JP. Patología oral y maxilofacial contemporánea. 2 ed. Madrid: Elsevier; 2005. [ Links ]
2. Feinberg SE, Steinberg B. Surgical management of ameloblastoma. Current status of the literature.Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1996;81:383-8.
3. Gardner DG. Some current concepts on the pathology of ameloblastomas.Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1996;82:660-9.
4. Kahn MA.Ameloblastoma in young persons: a clinicopathologic analysis and etiologic investigation.Oral Surg Oral Med Oral Pathol 1989;67:706-15.
5. Gardner DG, Pecak AM. The treatment of ameloblastoma based on pathologic and anatomic principles. Cancer 1980;46:2514-9.
6. Rosenstein T, Pogrel MA, Smith RA, Regezi JA. Cystic ameloblastoma--behavior and treatment of 21 cases. J Oral Maxillofac Surg 2001;59:1311-6.
7. Leider AS, Eversole LR, Barkin ME. Cystic ameloblastoma. A clinicopathologic analysis. Oral Surg Oral Med Oral Pathol 1985;60:624-30.
8. Al-Khateeb T, Ababneh KT. Ameloblastoma in young Jordanians: a review of the clinicopathologic features and treatment of 10 cases. J Oral Maxillofac Surg 2003;61:13-8.
9. Nakamura N, Higuchi Y, Mitsuyasu T, Sandra F, Ohishi M. Comparison of long-term results between different approaches to ameloblastoma.Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2002;93:13-20.
![]() Correspondence:
Correspondence:
Dr Javier Mareque Bueno
Secretaría servicio Cirugía oral y maxilofacial 8ª centro
Hospital Universitario Vall d´Hebrón
Pg de la vall d´Hebrón 119-129
08035 Barcelona
E.mail: 36984jmb@comb.es
Received: 30-10-2005
Accepted: 21-05-2006