Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Medicina Oral, Patología Oral y Cirugía Bucal (Internet)
versión On-line ISSN 1698-6946
Med. oral patol. oral cir.bucal (Internet) vol.12 no.2 mar. 2007
Oral rehabilitation with the new SG® attachment in a patient treated for oral squamous cell carcinoma
Gisela Senent1, Ignacio Barjau2, F. Javier Silvestre 3
(1) Associate Professor of the Unit of Prosthodontics and Occlusion, Department of Stomatology, University of Valencia
(2) Assistant Professor of the Unit of Prosthodontics and Occlusion, Department of Stomatology, University of Valencia
(3) Assistant Professor of the Unit of Clinical-Surgical Odontology, Department of Stomatology, University of Valencia. Head of the Stomatology Unit, Dr. Peset University. Valencia (Spain)
ABSTRACT
In patients who have undergone surgery and radiotherapy for oral squamous cell carcinoma (OSCC), the posterior oral rehabilitation may prove complex. In addition to the defects produced by surgical ablation of the primary tumor, radiotherapy induces deleterious effects upon the oral tissues. We present the case of a 48-year-old male treated two years before due to OSCC in the retromolar trigone and left lateral wall of the oropharynx. Following study of the case with clinical examination and orthopantomography, a management plan was defined involving rehabilitation of the upper dental arch with fixed ceramometallic prostheses, while in the lower arch we chose a unilateral removable prosthesis adapted to a fixed prosthesis by means of a special and versatile attachment based on a new system that functions as a fixed element but which can be removed or changed at some later date. The present clinical case illustrates this type of prosthodontic solution for the management of oncological patients of this kind.
Key words: Oral cancer, oral rehabilitation, SG® attachment.
RESUMEN
En los pacientes tratados con cirugía y radioterapia, debido a un carcinoma oral de células escamosas la posterior rehabilitación bucal puede resultar compleja. A los defectos producidos por la cirugía ablativa del tumor primario, se le añaden los efectos de la radioterapia sobre los diversos tejidos orales.
A continuación se presenta el caso de un varón de 48 años tratado 2 años antes de un carcinoma oral de células escamosas en trígono retromolar y pared lateral de orofaringe. Tras la exploración clínica y radiográfica se realizó un plan de tratamiento que en la rehabilitación de la arcada dental superior fué con prótesis fija ceramometálica y una prótesis removible unilateral inferior sujeta a una prótesis fija mediante un atache especial. Este tipo de atache está basado en un nuevo sistema que funciona como una prótesis fija, pero puede ser removido o cambiado en el futuro, lo cual resulta muy versátil.
El objetivo de la presentación de este caso clínico es mostrar esta nueva solución para el tratamiento de este tipo de pacientes oncológicos.
Palabras clave: Cáncer oral, rehabilitación oral, atache SG-pasador.
Introduction
Approximately 3% of all malignant tumors affect the oral cavity, and of these, oral squamous cell carcinomas (OSCC) accounts for over 90% of all cases. The frequency of oral cancer in Spain ranges from 12-15 cases/100,000 inhabitants per year in males, versus 2-4 cases/100,000 inhabitants per year in females. If diagnosed in the early stages of the disease, survival after 5 years reaches 80%, versus 40% if the regional lymph nodes are affected at the time of diagnosis (1,2).
In the past, the treatment of OSCC inevitable left physical and mental sequelae, with a loss of patient quality of life. The most important management options for these lesions comprise surgery and radiotherapy, either isolatedly or in combination, depending on the clinical stage of the tumor (3). Ablative surgery involves removal of the entire lesion, ensuring a generous resection safety margin, together with excision of the cervical lymph nodes.
One of the problems of the posterior oral rehabilitation of these oncological patients after surgery is represented by the removal of hard tissues along with the tumor lesion – leaving important tissue defects. This in turn complicates the subsequent fitting of a removable dental prosthesis in an attempt to substitute the affected dental arch – particularly if radiotherapy has also been administered (4). At present, there are cases in which the utilization of a unilateral removable prosthesis may help solve these problems, even if the prosthesis is not biomechanically ideal. In the present study we describe the preparation and fitting of a unilateral removable prosthesis as clinical solution to these problems.
Clinical case
A 48-year-old male had been diagnosed two years before of OSCC in the retromolar trigone and left lateral wall of the oropharynx. At that time ablative surgery was carried out with resection of the lesion, including a segmental mandibulectomy and posterior of placement of a titanium bar for mandibular reconstruction. Bilateral radical left and right supraomohyoid cervical lymph node resection was also carried out. This was followed by radiotherapy. After surgery, the patient developed facial edema (treated with corticoids) and grade III mucositis (alleviated with analgesics and topical antiseptics to avoid secondary infection of the lesions).
The patient was then seen in our center for oral rehabilitation due to the existence of eating problems. Physical examination of the upper maxilla revealed the absence of left premolars and molars (second quadrant), and of two right premolars. The upper right third molar was fully impacted. Caries were seen to affect the incisors, and particularly the two upper central incisors.
In the mandibular process there were teeth up to tooth 35, followed by a segmental mandibulectomy extending to the mandibular angle. The left hemimandible was splinted with a titanium bar screwed at both ends. On the lower right side there were teeth up to the second premolar, followed by a posterior edentulous zone (Fig. 1). The lower incisors showed some attrition at the incisor margins, and anterior occlusion corresponded to Class I.
Management planning was conditioned by a number of factors. On one hand, dental implant rehabilitation was not possible, due to the risks posed by the prior radiotherapy. A bilateral conventional removable prosthesis was likewise not feasible, since forces were to be avoided on the left mandibular side. We considered a fixed rehabilitation in the upper arch with individual ceramometallic crowns from 12 to 23, and with a ceramometallic bridge from 13 to 16, using both teeth as abutments. The reason for not extending treatment beyond 23 was to avoid leverage on the tooth closest to the line of the mandibular lesion, thus favoring its recovery. Likewise, in the lower arch, we planned placement of a right unilateral, removable partial prosthesis using a special attachment anchored to three splinted abutment teeth by means of crowns of the same characteristics, with their corresponding contours drilled to increase stability of the removable prosthesis. We avoided touching the rest of the mandibular teeth – in wait of full patient recovery after the imminent programmed graft procedure.
The SG® attachment was used (Cendres-Metaux). This is a new system based on the use of a single male adaptor attached to the fixed part of the prosthesis, and over which 6 different female adaptors can be used, attached to the removable part of the prosthesis; exchange and replacement is thus greatly facilitated. These female adaptors offer: (a) hinge mobility; (b) friction attachment; (c) adjustable friction attachment; (d) retention attachment; (e) lock attachment; and (f) screw attachment.
The male adaptor in turn consists of a cylinder which on one side attaches via a rectangular body to a likewise rectangular structure ending in a tip on the gingival side, with two semicircular grooves on either side, vestibular and lingual. This body is traversed occlusal to gingival by a cylindrical hollow compartment communicating with the exterior via a groove. At its opposite end, the cylinder presents a notch perpendicular to the latter.
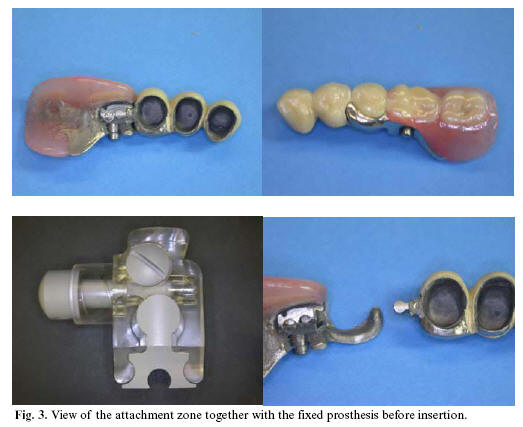
The female adaptor used in this case comprised the lock attachment design. The internal female cage fully adapts to the male at its buccal and lingual portion, while the distal portion is equipped with a bolt presenting a spring and bolt retention screw which is inserted through the apical portion of the female adaptor. The bolt is equipped with a button which upon pressing gives rise to a cylinder with a notch at its lingual most portion that extends beyond the cylinder of the male adaptor; distally, it in turn presents a longer notch for retention with the retention screw. The spring is housed in the lingual most portion of the bolt (Fig. 2 and 3).
The dimensions of the attachment are 3.50 mm in the apical-occlusal direction, 3.50 mm vestibular-lingual, and 6.55 mm in the mesial-distal direction. It is indicated for use in unilateral or bilateral free-end prostheses, interspaced prostheses, interspaced and free-end prostheses, over implants, and in prostheses with prevention of future modifications.
Discussion
It is known that removable prostheses are to be prepared bilaterally to ensure good retention and function. However, there are situations in which an ideal approach is not possible, and alternatives must be available for adequately resolving the problems faced.
With the growing use of implants, our first choice would have been to use them for the restoration, particularly in the lower arch, to thus offer the advantage of fixed rehabilitation in the mouth. However, due to the particularities of the case and rejection on the part of the patient, implants were in principle discarded, in wait of their possible use at some future point in time (5-7).
In the present case there were two posterior edentulous zones, though we opted for a unilateral rather than a bilateral removable prosthesis, in view of the complications derived from treatment of the oral cancer on the left side. In the upper part we established ceramometallic restorations in the anterior teeth, due to the caries secondary to xerostomia (Fig. 4). The left side was left without occlusion, and group function was established on the right side.
This type of attachment was used in view of its stability in unilateral cases, and its in-mouth safety, since removal is not possible unless the aforementioned button is pressed and the prosthesis is deliberately displaced. It is also important to emphasize that this type of attachment is equipped with a male adaptor that can be used with different female fittings, depending on the planned treatment modality. As a result, it is useful for future changes in rehabilitation. If a bilateral removable prosthesis were planned, it would suffice to place a second similar male adaptor on the right side, without having to remove the prosthesis already in place. Another solution could be to position a lower bridge on the right side, though we could only have secured one further crown in extension – with the risks this involves – and the pre-existing problem would not have been resolved, since chewing function would not have been improved to any important degree.
References
1. Martínez R, Aguirre JM, Burgos JJ, Rivera JM. Factores clínico-patológicos en el carcinoma de células escamosas inicial de lengua y suelo de la boca en Vizcaya. Med Oral 2001;6:87-94. [ Links ]
2. Chimenos E, Finestres F, Huguet P. Carcinoma escamoso gingival: caso clínico y diagnóstico diferencial. Med Oral 2001;6:335-41.
3. Ord RA. Surgical management of oral cancer. En: Oral Cancer. The dentist´s role in diagnosis, management, rehabilitation and prevention. Ord RA, Blanchaert RH (eds). Chicago:Quintessence Publishing Co; 2000. p. 81-92.
4. Kramer DC. The radiation therapy patient: treatment planning and postreatment care. En: Clinical maxillofacial prosthetics. Taylor TD (ed). Chicago:Quintessence Publishing Co; 2000. p.37-52.
5. Taylor TD, Worthington P. Osseointegrated implant rehabilitation of the previously irradiated mandible: results of a limited trial at 3 to 7 years. J Prosthet Dent 1993;69:60-9.
6. Cohen SR, Orenstein JH. The use of attachments in combination implant and natural-tooth fixed partial dentures: a technical report. Int J Oral Maxillofac Implants 1994;9:230-4.
7. Ormianer Z, Brosh T, Laufer BZ, Shifman A. Strains recorded in a combined tooth-implant restoration : an in vivo study. Implant Dent 2005;14:58-62.
8. Etienne OM, Taddei CA. Use of bar-clip attachments to enhance the retention of a maxillofacial prosthetic obturator: a clinical report. J Oral Rehabil 2004;31:618-21.
9. Omondi BI, Guthua SW, Awange DO, Odhiambo WA. Maxillary obturator prosthesis rehabilitation following maxillectomy for ameloblastoma: cases series of five patients. Int J Prosthodont 2004;17:464-8.
10. Arigbede AO, Dosumu OO, Shaba OP, Esan TA. Evaluation of speech in patients with partial surgically acquired defects: pre and post prosthetic obturation. J Contemp Dent Pract 2006;7:89-96.
![]() Correspondence:
Correspondence:
Dr. F. Javier Silvestre
Clínica Odontológica Universitaria
C/ Gascó Oliag 1, 46010-Valencia
E-mail: francisco.silvestre@uv.es
Received: 20-04-2006
Accepted: 5-01-2007