My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Medicina Oral, Patología Oral y Cirugía Bucal (Internet)
On-line version ISSN 1698-6946
Med. oral patol. oral cir.bucal (Internet) vol.12 n.2 Mar. 2007
Temporomandibular juxtaarticular chondroma: case report
Inés Vázquez Mahía1, José Luis López-Cedrún Cembranos2, José Ferreras Granado1, Fernanda Lorenzo Franco1
(1) Médico Adjunto del Servicio de Cirugía Oral y Maxilofacial
(2) Jefe de Servicio de Cirugía Oral y Maxilofacial. CHU Juan Canalejo. A Coruña
ABSTRACT
Chondromas are benign tumours composed of mature hyaline cartilage.
We present here the first case in the English language medical literature of juxtaarticular chondroma of the temporomandibular joint in the parotid region. Within the rarity of cartilage disorders of the temporo-mandibular joint (TMJ), this particular condition is a diagnostic curiosity. The patient, a 54 year old woman, presented a right preauricular tumour of 3.5 cm. which had been developing for 4 years. It was not painful but there was a recent symptomology of TMJ dysfunction, with pain and clicks. The diagnostic possibilities of a parotid pleomorphic adenoma and of a cartilage tumour of the TMJ suggested a difficult preoperative differential diagnosis, which influenced our approach regarding therapy. The tumour was excised, preserving the parotid gland. This enabled us to confirm the histological diagnosis of chondroma, composed solely of chondroide tissue.
We have described the clinical characteristics of our case, and carried out a review of the relevant literature, emphasising the differential diagnoses.
Key words: Juxtaarticualar chondroma, TMJ, parotid tumour.
RESUMEN
Los condromas son tumores benignos compuestos por cartílago hialino maduro.
Presentamos el primer caso en la literatura anglosajona de condroma yuxtaarticular temporomandibular en la región parotídea. Dentro de la rareza de los trastornos cartilaginosos de la ATM, esta entidad constituye una auténtica curiosidad diagnóstica. El paciente, mujer de 54 años de edad, presenta un tumor preauricular derecho de 3,5 cm, de 4 años de evolución, no doloroso pero con sintomatología reciente de disfunción de ATM, con dolor y chasquidos. Las posibilidades diagnósticas de un adenoma pleomorfo parotídeo y de un tumor cartilaginoso de la ATM plantean un diagnóstico diferencial preoperatorio difícil, que nos condicionaba la actitud terapéutica.
Se realizó la extirpación del tumor conservando la glándula parótida, lo que nos permitió confirmar el diagnóstico histológico de condroma, compuesto exclusivamente por tejido condroide.
Describimos las características clínicas de nuestro caso, y hacemos una revisión de la literatura al respecto, haciendo hincapié en los diagnósticos diferenciales.
Palabras clave: Condroma yuxtaarticular, ATM, tumoración parotídea.
Introduction
Chondromas are benign tumours of mesenchymal origin composed of multiple nodules of mature hyaline cartilage. Depending on their location they are either classified as enchondromas, which make up 80% of the total, located in the medullary cavity of the bony skeleton, or as juxtaarticular chondromas (related to extraskeletal cartilage) (1,2). The enchondromas generally appear in the metaphysis of the long bones of patients who are growing and in the diaphysis of adult patients. The juxtaarticular chondromas were described for the first time by Lichtenstein and May in 1952 (3), and at present the term "pereosteal" is preferred due to the involvement of the pereosteum in the genesis of these tumours (4). A third group of chondromas consists of the extraskeletal chondroma or soft tissue chondroma, a rare cartilaginous tumour which is found most frequently in the hands and feet (5). They are extremely rare in the head and neck area, having been described mainly in the tongue and the buccal mucosa (6,7).
We present here a case of chondroma in the parotid region, near but not in contact with the temporomandibular joint, which presents a difficult differential diagnosis between a pleomorphic adenoma of the parotid gland and cartilaginous tumours of the TMJ.
Clinical case
A 54-year-old female patient, who presented a petrous tumour in the right preauricular region of approximately 2.5cm x 2.5cm, which had been developing painlessly over 4 years. In the last two years it had increased in size slowly and progressively, presenting clicks and pain in the right TMJ.
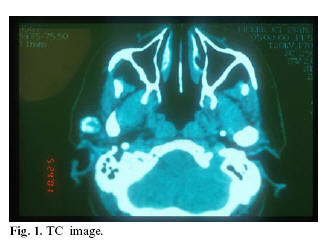
The orthopantomographic assessments did not reveal any alterations, showing a condyle of normal morphology. The CT scan showed tumouring in the right parotid bed, which was heterogeneous and "lumpy" in appearance (fig. 1). The fine needle aspiration (FNA) showed a cytological picture corresponding to a tumour with exclusively chondroid differentiation, which could well be a mixed salivary tumour with significant cartilaginous differentiation or a true chondroid tumour.
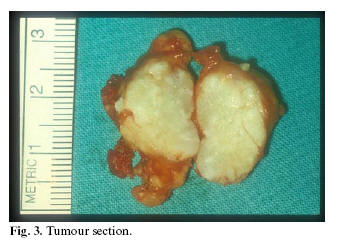
The tumour was excised by means of a preauricular incision, checking intraoperationally both that it was independent of the parotid gland and its proximity to the capsule of the temporomandibular joint. Macroscopic examination during the operation showed that it was not a salivary tumour and that it was indeed a chondroid tumour (figure 2 and 3). Because of this the parotid gland was not resected.
Microscope study confirmed the diagnosis of chondroma.
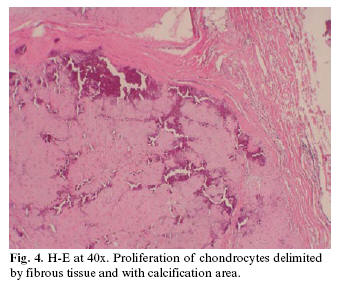
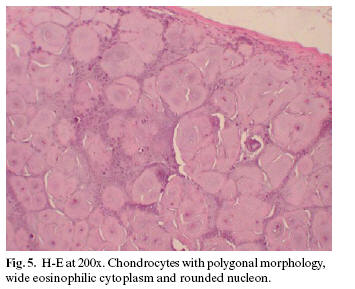
A lobed formation could be observed, well delimited by fibrous tissue, composed of chondroid tissue with abundant base material. Small calcified granules were similarly observed in its interior. The chondrocytes showed quite regular nuclei, ovoid in shape (fig 4 and 5).
Discussion
Chondromas represent approximately 2.38% of osteocartilaginous tumours of the organism in the register of tumours described by Dahlin and Unni (8). Tumours are rarely located in the TMJ: out of a series of 3,200 tumours in the head and neck, only 7 were found in the TMJ (9). The majority are primitive bone tumours, principally osteomas or osteochondromas (10). At this level they present as a preauricular tumour, of progressive slow growth that eventually produce a symptomology of auricular dysfunction.
The cartilaginous tumours of the TMJ are even less common, principally being chondromas. Other less common histological types are chondromyxoid fibroma, chondroblastoma, chondrosarcoma, synovial chonromatosis (11) and ganglions or synovial cysts, which are the result of a herniation of the synovial capsule.
The rarity of cartilaginous tumours of the TMJ, their painless nature and their unremarkable radiological appearance makes their diagnosis difficult. There are three types of articular chondromas: enchondromas, which are situated in the medulla, which for many authors represent a variant of condylar hyperplasia; juxtaarticular or pereosteal chondromas, located in the periphery of the joint; and the extraskeletal or soft tissue chondromas, which are situated outside the joint. Hystologically they are characterised by lobulated masses partially subdivided in nodules of hyaline cartilage immersed in a fibrous stoma. Frequently there are calcified foci and even ossification (1).
The TMJ chondromas published correspond to osteochondromas, diagnosed radiologically by a circular or ovoid growth on the head of the condyle. Some authors consider this to be an osteocartilaginous exostosis due to an alteration of development because of a fault in the direction of epiphyseal cartilage growth, leading to exotosis in the bone surfaces (1).
Other authors consider them to be the result of the growth of germ cells with cartilaginous potential as a consequence of continuous tensions exerted on particular tendons (12,13). Kruger considers that they are calcified chondromas and that they have stopped growing (14). Lichtenstein considers that the areas of calcification should be considered as evidence of development or regression of a lesion over a long period (15,16).
Forssell and Cols (13), in a review of the literature, found 19 well documented cases of articular osteoma. The majority of the tumours of this series are situated in the external face of the condyle, above all in the anterior medial section; in their article they provide a new case, radiologically evident due to a visible oval mass in the anterior medial face of the head of the condyle. This is a typical example of these tumours. We think that some of the cases in the series outlined by these authors relate to pereosteal chondromas, as there have not been any TMJ tumours described in the published literature with this name.
The difficulty of a preoperational diagnosis in the case which we present is based on the location and the histological appearance which, a priori, are incompatible. From the clinical point of view initially the differential diagnosis suggested a pleomorphic adenoma of the parotid gland. The FNA indicated two possibilities: either chondroide differentiation of a pleomorphic adenoma or an extraskeletal chondroma. The "lumpy" appearance did not point to this latter possibility. However, the possibility of a pleomorphic adenoma could not be ruled out until the interoperational finding of a microscopically wholly chondroide extraglandular adenoma. The chondromatosic changes of the pleomorphic adenoma or mixed parotid tumour can be similar to a chondroide tumour, these areas being cartilaginous as the result of the accumulation of mucoid material around the myoepithelial cells.
Histologically our case presents a clear diagnosis of chondroma, as the scarcity of areas of calcification rule out a diagnosis of osteochondroma. In the review of the literature we did not find any cases of chondroma of the TMJ. There was only one description, in German, of a chondroma in the parotid area (17). In this exceptional case the authors employed immunohistochemistry to make a differential diagnosis with pleomorphic adenoma. The cells presented a clear morphology of cartilaginous cells and were only positive for the protein S-100 (cartilage-specific). In our case the total absence of epithelium was sufficient to rule out pleomorphic adenoma.
In relation to the classification of the chondroma, we consider that it is a juxtaarticular or pereosteal chondroma due to its proximity to the joint. The posterolateral location in relation to the manibular condyle, and lack of contact with the articular surface, differentiates it from the osteochondromas published in the literature, as all of them were in an anterior medial position or above, always in contact with the articular surface, as well as having a bony component present in their histology.
References
1. SL Robbins, RS Cotran,V Kumar. El aparato locomotor en Patología estructural y funcional. Madrid: Ed Mc Graw-Hill; 1995. p.1358-9. [ Links ]
2. Takayuki N, Krishnan KU, Richard AM. Douglas JP: Periosteal chondroma and periosteal chondrosarcoma. The American Journal of Surgical Pathology 1985;9:666-77.
3. Lichtenstein L, Hall JE. Periosteal chondroma: a distinctive bening cartilage tumour. J Bone Joint Surg (Am) 1952;34:691-7.
4. Boriani S, Bacchini P, Bertoni F, Campanini M. Periosteal chondroma. A review of twenty cases. The Journal of bone and Joint Surgery 1983;65:205-12.
5. O´Malley MJ, Faller GT, Craig CC. Extraskeletal chondroma of the foot. Orthopedics 1996;19:256-8.
6. Blum MR, Danford M, Speight PM. Soft tissue chondroma of the cheek. J of Oral Pathology and Medicine 1993;22:334-6.
7. Chang SE, Lee MW, Choi JH, Sung KJ, Moon KC, Koh JK. A case of lingual chondroma. Br J of Dermatology 1999;141:773-4.
8. Dahlin DC, Inni KK. Bone tumours. General aspects and data on 8542 cases, 4th eds. Springfield, Illinous: Charles C. Thomas; 1986. p.120-8.
9. Nkoku A, Koch H. The temporomandibular joint: a rare localitation for bone tumours.J Max Fac Surg 1974;2:113-9.
10. Reychler H. Pathologie articulare temporo-mandibulaire. En: Piette E, Reychler H. Traité de pathologies buccale et maxillo-faciale. Bruxelles : De Boeck-Wesmael, S.A.; 1991. p. 1437-79.
11. Martin-Granizo R, Sanchez JJ, Jorquera M, Ortega L. Synovial chondromatosis of the temporomandibular joint: a clinical, radiological and histological study. Med Oral Patol Oral Cir Bucal 2005;10: 272-6.
12. Weinmann SP, Sicher H. Bone and bones:Fundamentals of bone biology, 2nd Ed. St. Louis: Mosby; 1955. p. 339-60.
13. Forssell H, Happonen RP, Forssell K, Virolainen E. Osteochondroma of the mandibular condyle report of a case and review of the literature. Br J of Oral and Max Surg 1985;23:183-9.
14. Kruger GO. Text book of oral and maxillofacial surgery 6ª ed. St. Louis: Mosby; 1984. p.648-50.
15. Ashley DJB. Evans Histological Appearances of Tumours. 4th edition. London: Livingstone; 1990. p.133-9.
16. Linchtenstein L. Bernstein D. Unusual bening and malignant chondroid tumours of bone: a survey of some mesenchymal cartilage tumours and malignant chondroblastic tumours, including a few multicentric as well as many atypical bening chondroblastomas and chondromyxoid fibromas.Cancer 1959;12:1142-57.
17. Kostopoulos IS, Daniilidis I, Velegrakis G, Papadimitriou CS. Chondroma of the parotid gland. Clinical-histologic-immunohistochemical findings of a rare case. Laryngorhinootologie.1993;72:261-3.
![]() Correspondence:
Correspondence:
Dra. Inés Vázquez Mahía
Servicio de Cirugía Oral y Maxilofacial.
CHU Juan Canalejo.
As Xubias de Arriba, 84
15006 A Coruña
E-mail: vmahia@canalejo.org
Received: 30-11-2005
Accepted: 3-09-2006