Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Medicina Oral, Patología Oral y Cirugía Bucal (Internet)
versión On-line ISSN 1698-6946
Med. oral patol. oral cir.bucal (Internet) vol.12 no.4 ago. 2007
Reparative giant cell granuloma in a pediatric patient
Blanca Duarte Ruiz1, Francisco de Asís Riba García1, Carlos Navarro Cuéllar2, Tommaso Bucci3, Matías Cuesta Gil4, Carlos Navarro Vila5
(1) Associate Doctor. Servicio de Cirugía Oral y Maxilofacial. Hospital General de Ciudad Real
(2) Associate Doctor. Servicio de Cirugía Oral y Maxilofacial. Hospital Universitario de Guadalajara
(3) Resident Doctor. Servicio de Cirugía Oral y Maxilofacial. Hospital General Universitario Gregorio Marañón. Madrid
(4) Head of Service. Servicio de Cirugía Oral y Maxilofacial. Hospital General de Ciudad Real
(5) Head of Department, Maxillofacial Surgery. Universidad Complutense de Madrid. Jefe de Servicio. Servicio de Cirugía Oral y Maxilofacial. Hospital General Universitario Gregorio Marañón. Madrid. España
ABSTRACT
Reparative giant cell granulomas are benign, infrequent tumors, of non-odontogenic origin, that develop at central or peripheral level. Peripherally located lesions are frequently denominated giant cell epulis, and never correspond to true neoplasia, but rather to inflammatory reactions secondary to another lesion (hemorrhage, etc.).
It should be taken into account, that in general, head and neck tumors of infancy usually demonstrate an atypical biological behaviour. Furthermore, the anatomicopathologic diagnosis is often compromised in this type of lesion.
We present the case of a 6-year-old boy, who, three weeks after suffering a slight facial trauma, developed a painless, exophytic swelling of approximately 4 cm, with bleeding on palpation, in the ipsilateral hemimaxilla. The lesion demonstrated rapid, progressive and continuous growth. The facial CT and incisional biopsy confirmed the suspected diagnosis of reparative giant cell granuloma. The patient was surgically treated, carrying out a left marginal maxillectomy associated with the extirpation of the soft-tissue lesion.
The resultant defect was reconstructed with a Bichat fat-pad providing the patient with optimal esthetic and functional results. The definitive anatomicopathologic report of the surgical piece is compatible with reparative giant cell granuloma.
Key words: Reparative granuloma, giant cells, marginal maxillectomy, Bichat fat-pad.
RESUMEN
Los granulomas de reparación o reparativos de células gigantes, son tumores benignos e infrecuentes, de estirpe no odontogénica, que se desarrollan a nivel central o periférico. Las lesiones emplazadas en esta última localización, con frecuencia se denominan épulis de células gigantes, y en ningún caso corresponden a neoplasias verdaderas, sino a procesos inflamatorios reactivos y secundarios a otra lesión (hemorragia, etc.).
Debemos tener en cuenta que, en general, los tumores de cabeza y cuello en la infancia, suelen mostrar un comportamiento biológico peculiar. Por otra parte, el diagnóstico anatomopatológico de este tipo de lesiones, en muchas ocasiones resulta comprometido.
Presentamos el caso de un paciente varón de 6 años de edad que a las tres semanas de sufrir un traumatismo facial izquierdo leve, desarrolla una tumoración de 4 cms. aproximadamente, indolora, exofítica y sangrante al tacto, en el hemimaxilar superior ipsilateral. La lesión muestra un crecimiento continuo, progresivo y veloz. Realizados TC facial y biopsia incisional de la lesión que nos confirma el diagnóstico de sospecha de granuloma reparativo de células gigantes, se procede a intervenir quirúrgicamente al paciente, realizándosele, maxilectomía marginal izquierda asociada a la extirpación de la tumoración dependiente de partes blandas. El defecto se reconstruye con un colgajo de bola adiposa de Bichat que proporciona al paciente una funcionalidad y resultado estético óptimos. El informe anatomopatológico definitivo de la pieza quirúrgica, ulterior a la cirugía, es compatible con granuloma reparativo de células gigantes.
Palabras clave: Granuloma reparativo, células gigantes, maxilectomía marginal, colgajo de bola adiposa de Bichat.
Introduction
Head and neck tumors of infancy present some particular characteristics with regard to their biological behaviour, and often their anatomicopathological diagnosis is compromised. Giant cell lesions are benign, non-odontogenic, relatively uncommon tumors of the oral cavity. They develop peripherally in soft tissues (gingiva) or centrally (in bone) (1). Although the etiology remains unclear, the peripheral lesions are often denominated giant cell epulis and correspond to secondary inflammatory reactions to another type of aggression (local trauma, hemorrhage, chronic irritants, etc.) (1, 2). Given that they are not true neoplasia, it is convenient to name them reparative giant cell granuloma.
We present this unusual clinical case, which we consider to be of great interest, together with the diagnostic and treatment methods applied. Likewise, we establish the differential diagnosis against other intraoral lesions of infancy, especially giant cell tumors.
Clinical case
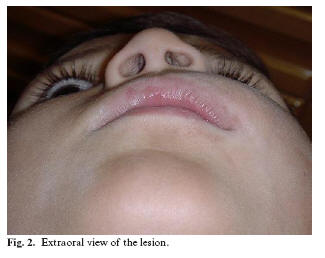
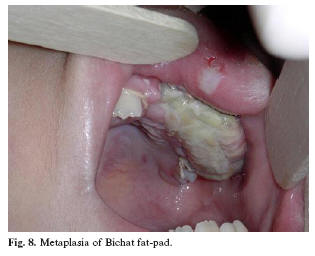
The case concerns a young, six-year-old male patient evaluated for the presentation of a painless swelling of less than one months evolution in the left hemimaxilla. The patient referred having suffered a slight left facial trauma three weeks before the appearance of the lesion, following which a rapid, progressive, and continuous growth ensued. The patient was unhurt and in general good health. On examination, we confirmed the presence of a swelling of approximately 4 cm in size, in the left hemimaxilla, between the incisor and molar teeth (Figure 1). There was mobility of the permanent incisors and of the remaining deciduous teeth. The swelling extended over the left nasogenian sulcus producing an obvious facial asymmetry (Figure 2). The palatal mucosa remained entirely preserved, and was of normal appearance and consistency. The facial CT revealed that the lesion had destroyed the left external maxillary bone, from the incisors to the molars on that side (Figure 3). The biopsy results were compatible with the diagnosis of giant cell granuloma. Based on the above-mentioned suspected diagnosis, a left marginal maxillectomy, associated with the extirpation of the soft-tissue lesion, was carried out under general anesthetic. Likewise, the permanent central and lateral incisors as well as the tooth germs of the canine and first premolars were included in the resection (Figures 4, 5). The defect was reconstructed using a Bichat fat-pad (Figures 6, 7, 8). The definitive anatomicopathologic report of the surgical specimen was compatible with reparative giant cell granuloma.
Two years after surgery, the patient is free of disease. The intraoral reconstruction has an excellent appearance, almost indistinguishable from the adjacent mucosa (Figures 9, 10). The child is wearing a removable prosthesis until he is fully-grown, when a maxillary and dental reconstruction can be designed on demand (Figures 11, 12).
Disscusion
The term giant cell lesions, covers three nosologic entities: giant cell granuloma, brown tumor and cherubism. All are highly controversial, both etiologically (neoplastic or reactive) and regarding their denomination (giant cell granuloma, reparative giant cell granuloma, or giant cell tumor). Histologically, the three lesions are characterized by the presence of abundant giant multinucleated cells. Some studies have investigated the etiology of this disease, concluding that the three entities have some similar cytologic and histologic characteristics, and when evaluating the expression of the c-Src gene have established that this may be implicated in the development of these three pathologies include under the term giant cell lesions (3).
The giant cell lesion originates either peripherally (gingival mucosa) or centrally (in the bone), affecting the adjacent tissues (by direct spread) as it grows.
Mandibular involvement is more frequent (6.5% of benign mandibular tumors) than maxillary (4). Furthermore, the majority of these lesions are located anteriorly to the first molar, on many occasions crossing the midline. They behave as single lesions, consequently, the appearance of multiple lesions should alert the possibility of an associated hyperparathyroidism or cherubism (the central giant cell lesion can be associated to both these entities).
The mean age at diagnosis is around 24 years (89% before the age of 40), there is a female predilection, and no racial differences have been found (1). The existence of prior trauma to the affected area is uncommon.
The clinical behaviour of these types of lesion is distinctly variable, and sometimes difficult to predict. The fundamental clinical sign is swelling, with or without tooth mobility, and growth that ranges between silent and aggressive. Patients with highly aggressive lesions (generally younger patients with larger tumors) usually have associated pain, bleeding, and local bone destruction (resorption) with tooth displacement and radicular resorption, as with the case herein described (4).
In the radiographic study, the lesion usually presents a transparent, multilocular honeycombed appearance, with fine bone walls that cross the affected area.
However, unilocular tumors, without trabeculation exist. An intense spread is often seen, with cortical thinning and even cortical perforation in the case of large tumors. The maxillary lesions produce radiopacities in hourglass configuration.
Histologically, this granuloma is characterized by the appearance of abundant benign giant cells (each with 5-10 nuclei, and high mitotic activity, above all in the case of highly-aggressive lesions) with proliferation of cells in bone without atypia and with osteoclastic activity among them (4). Abundant hemorrhagic foci are evident. Increased osteoblastic activity with development of reactive bone is also characteristic of this entity.
The differential diagnosis should be established against other types of lesions such as aneurysmatic bone cyst, cherubism, brown tumor, ameloblastoma, lesions associated with hyperparathyroidism and fibrous dysplasia, among others.
The histological, radiographic and clinical diagnosis is particularly difficult in these types of lesion. In spite of this, the combination of a radiographic examination (unilocular or multilocular radiolucency), histological findings (giant cells contained within the fibroblastic matrix), serum levels of parathyroid hormone (compatible with normal levels) plus the clinical characteristics, confer the diagnosis of giant cell granuloma, and allow us to approach the surgical treatment correctly (5).
On the other hand, and in general, the anatomicopathologic characteristics of reparative giant cell granuloma are reliable indicators of the differentiation between aggressive and nonaggressive lesions. This fact should also be taken into account when planning individualized treatment and follow-up for each case (4).
The treatment for these types of lesion has frequently been a subject of interest for the scientific community. Thus, some authors, based on the presumed similarities existing between giant cell granulomas, brown tumors in hyperparathyroidism, and some proliferative vascular lesions, have administered calcitonin and interferon alpha as a basis of treatment for this pathological entity. Unfortunately, on occasions the result has not been as successful as was first anticipated, producing severe secondary complications such as erythematous lupus, and pancreatitis secondary to the administration of interferon alpha due to the difficulty in managing these types of drug (6).
Regarding the therapeutic approach, controversy may arise with regard to the aggressiveness of surgical treatment. Our attitude tends to be as conservative as possible (always and whenever there is no evidence of malignant neoplasia), at all times taking into consideration that recurrences are not infrequent, above all in association with the more aggressive lesions (4, 5, 7). Finally, we highlight the use of the Bichat fat-pad in the repair of these types of maxillary lesions. This reconstructive method was chosen because it is simple to apply, it bears a close resemblance to the surgical defect and is highly reliable; there are no sequelae, and the esthetic and functional results are excellent, thanks to the metaplasia developed by the fat-pad, which makes it practically indistinguishable from the remaining oral mucosa (8, 9).
References
1. Yalcin F, Yalcin S, Berber L, Gur H. Peripheral giant cell granuloma combined with facial hemangioma. A case report. J Int Acad Periodontol 2005;7:108-13. [ Links ]
2. Martins MD, Pires F, Daleck F, Myaki SI, Friggi MN, Martins MA. Peripheral giant cell granuloma in anterior maxilla: case report in a child. J Clin Pediatr Dent 2005;30:161-4. [ Links ]
3. Wang C, Song Y, Peng B, Fan M, Li J, Zhu S et al. Expression of c-Src and comparison of cytologic features in cherubism, central giant cell granuloma and giant cell tumors. Oncol Rep 2006;15:589-94. [ Links ]
4. Kruse-Losler B, Diallo R, Gaertner C, Mischke KL, Joos U, Kleinheinz J. Central giant cell granuloma of the jaws: a clinical, radiologic and histopathologic study of 26 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2006;101:346-54. [ Links ]
5. Driemel O, Staudenmaier R, Hertel K, Pistner H, Kosmehl H. Central giant cell granuloma of the mandible: Definition and differential diagnosis. HNO 2006;54:705-8. [ Links ]
6. Goldman KE, Marshall MK, Alessandrini E, Bernstein ML. Complications of alpha-interferon therapy for aggressive central giant cell lesion of the maxilla. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2005;100:285-91. [ Links ]
7. Curtis NJ, Walker DM. A case of aggressive multiple metachronous central giant cell granulomas of the jaws: differential diagnosis and management options. Int J Oral Maxillofac Surg 2005;34:806-8. [ Links ]
8. Cuesta Gil M. Indicaciones actuales de los colgajos pediculados en la cirugía oncológica de cabeza y cuello. Madrid: Ed. Azulmarino; 2004. p. 21-9. [ Links ]
9. Martín-Granizo R, Naval L, Costas A, Goizueta C, Rodriguez F, Monje F et al. Use of buccal fat pad to repair intraoral defects: Review of 30 cases. Br J Oral Maxillofac Surg 1997;35:81-5. [ Links ]
![]() Correspondence:
Correspondence:
Dra Blanca Duarte Ruiz
C/ Ibiza 66, 1º D
28009 – Madrid (España).
E-mail: blancaduarte@terra.es
Received: 15-03-2006
Accepted: -2007