INTRODUCTION
Atrial fibrillation (AF) can have many potential consequences, the most disabling of which is stroke. AF is associated with a three-to five-fold increased risk of stroke, and onequarter of all ischemic strokes1. In elderly patients (> age 80), 40% of strokes are associated with AF2,3. Stroke prevention strategies in patients with AF include pharmacotherapy (antiplatelet therapy, vitamin k antagonists, and direct oral anticoagulants [DOAC])1 and left atrial appendage mechanical exclusion. According to clinical guidelines, anticoagulant therapy is the gold standard pharmacological prevention strategy in patients with no contraindications and a CHADs2-Vasc2 score ≥ 2 points4,5. Despite the proven value of oral anticoagulants for stroke prevention, studies show that these drugs are frequently underprescribed and/or underdosed, especially in frail patients, mainly due to concerns about drug-drug interactions6, poor therapeutic adherence, overestimated bleeding risk, older age, and/or risk of falls7,8.
Drug-related problems (DRP), which have been defined as a “situation that causes the emergence of a negative health effect associated with the drug”9, are an important and preventable cause of morbidity and mortality in all health care settings and patient populations. Several studies have found that anticoagulants are among the most common medications associated with preventable safety-related DRPs10,11, and these drugs have also been associated with untreated health-related DRPs, in which health problems occur as a consequence of not receiving the appropriate medical treatment. In one study, nearly one-third of patients with permanent AF who presented to the emergency department (ED) had medication-related negative outcomes, mostly due to undertreatment with antithrombotic therapy (31.1% of cases)12. Currently, the proportion of patients admitted to the ED for a stroke-related DRP associated with untreated or undertreated AF is unknown. Similarly, the effect of treatment modification at discharge in this patient population is also unknown.
In this context, the main aim of this study was to describe the characteristics of patients admitted to the ED for cardioembolic ischemic stroke with undertreated nonvalvular AF, a CHADs2-VASc ≥ 2, and no absolute contraindications for anticoagulant therapy. A second aim was to evaluate the effects of treatment modification on readmission rates and the risk factors associated with 30-and 180-day readmission to the ED, with the aim of determining the characteristics of patients who should be targeted for secondary prevention of this DRP.
MATERIAL AND METHODS
Study design
This was a retrospective, cross-sectional, observational study performed in a tertiary care hospital.
Setting and participants
The study was conducted at the ED at an urban teaching, tertiary referral hospital in Catalonia (Spain) that serves a population of approximately 407,000 inhabitants. The approximate annual volume at the ED is 150,000 patients, mainly adults (115,000). Of these, 40% are > age 65 years and more than 30% of them are considered vulnerable (dementia, dependence, active cancer, chronic diseases and comorbidities, and disability).
The study population included patients who presented to the ED for cardioembolic ischemic stroke during the year 2019 (January 1 to December 31). Inclusion criteria were: 1) adult patients (>18 years) with a previous diagnosis of nonvalvular AF or paroxysmal AF; 2) CHADs2-VASc score ≥2, and 3) no absolute contraindications for anticoagulants1.
Population of the study was identified through a search of the hospital database (Datawarehouse, SAP Business Object).
Variables
From the patients included, the pharmacological stroke prevention strategies used before and after the ischemic stroke were recorded, as well as, age, sex, hypertension, diabetes mellitus, dyslipidemia, heart failure, ischemic heart disease, chronic kidney disease stage 3 or worse (eGFR<60 mL min 1.73m2), active oncological disease, cognitive impairment and the destination at discharge. All the variables were collected by retrospective review of the Clinical Health Shared Record 242 of Catalonia.
Statistical análisis
Chi-squared tests were used to compare categorical data, and t-tests were used to compare mean ages at baseline.
Differences between patients readmitted to the ED 30 and 180 days after discharge versus those not readmitted based on the pharmacological treatment prescribed were evaluated using the chi-square test.
A univariate analysis was performed to identify the variables potentially associated with readmission to the ED at 30 and 180 days. The following variables were assessed: age >80 years; sex; presence of comorbidities, including stage 3 or higher chronic kidney disease (eGFR <60 mL/min 1.73 m2) 13, heart failure, type II diabetes mellitus, and hypertension; major polypharmacy (≥10 drugs, included medication prescribed as regular and “if needed”)14; change in anticoagulation therapy; and anticoagulant treatment prescribed at discharge from the ED. In patients who received low-molecular-weight heparin (LMWH) in the ED, this drug was also included in the analysis if the patient continued treatment for > seven days after the first episode or was readmitted to the ED during the course of LMWH treatment.
All variables on the univariate analysis with a p value <0.2 were included in the multivariate analysis to assess the risk factors significantly associated with 30 and 180-day ED readmission for all causes.
All statistical analyses were performed with the Stata 2 Software (StataCorp. 2011. Stata Statistical Software: Release 12. College Station, TX: StataCorp LP).
This study was approved by the Clinical Research Ethics Committee of the Sant Pau Hospital (Hospital Sant Pau; Reference No: IIBSP-COD-2018-25).
RESULTS
During the study period (2019), 547 patients presented at the ED for ischemic stroke. Of these, 113 (20.6%) met the study inclusion criteria and were analysed. The baseline characteristics of these patients are shown in table 1.
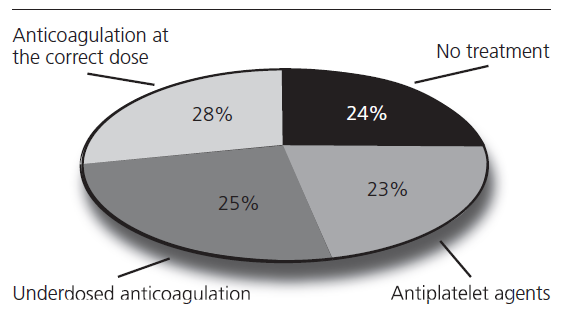
Of the 113 patients included in the study, 53 (46.9%) were not receiving anticoagulant drugs prior to the stroke episode. Of these 53 patients, 26 (49%) were receiving antiplatelet therapy (acetylsalicylic acid [n=22] or clopidogrel [n=4]), while the other 27 patients were not receiving any primary stroke prevention medication, despite the presence of AF.
The other patients (n=60, 53.1%) were taking anticoagulants prior to the ischemic stroke. However, 28 (46.6%) of these patients were taking lower doses than those recommended in the drug's technical data sheet. Thirty-two patients (28.3%) had an ischemic stroke, despite taking the appropriate preventative anticoagulant dose.
These results are summarized in figure 1 and table 2.
The stroke prevention strategy was modified in 44 patients (38.9%) at discharge. A total of 12 patients (10.7%) died during the episode and/or were discharged to an intermediate care centre for palliative or end of life care. In 57 patients, the preventive anticoagulation management strategy was not modified, despite the ischemic event.
The modifications made to the preventative treatment strategy are shown in table 3.
A total of 20 patients (17.7%) returned to the same ED for any cause at 30 days while 36 patients (31.8%) returned between days 31 and 180. Early re-consultation was associated with ischemic and/or haemorrhagic events in one patient (3.3%) (cardioembolic stroke in a patient with secondary prevention with acetylsalicylic acid). Between days 31 and 180, two patients presented at the ED for a second consultation, both for gastrointestinal bleeding (both patients were taking anticoagulants prior to the stroke) and none for ischemic events.
Diabetes is a risk factor associated with early readmission to the ED in the study population. No other risk factors associated with readmission at 30 and 180 days post-discharge were found (table 4).
DISCUSSION
This study was performed to describe the characteristics of patients with a diagnosis of AF admitted to the ED for cardioembolic stroke and to determine the effects of treatment modification on readmission rates and the risk factors associated with readmission. Most of the patients included in this study (71.6%) who presented to the ED for cardioembolic ischemic stroke did not meet the recommendations given in clinical guidelines for preventative anticoagulation therapy5. Importantly, undertreatment persisted even after the stroke in a high percentage of patients. On the multivariate analysis, the only risk factor significantly associated with early revisits to the ED was diabetes mellitus. Most of the patients in the study population were old (> age 80), had multiple comorbidities, and were receiving polypharmacy. Cognitive impairment was present in one-third of patients and one in four were institutionalized before the stroke.
According to clinical guidelines, the management of AF, especially in older patients, should prioritise anticoagulant therapy due to the high risk of cardioembolic stroke in these patients. Although age, cognitive impairment, and/or risk of falls do not contraindicate anticoagulation therapy, several studies have shown that these drugs are often underprescribed in these patients, as the findings of our study confirm7,8.
Table 1. Demographic and baseline clinical characteristics of the patient cohort

SD: standard deviation; n: number.
Table 2. Preventive pharmacological treatment prior to cardioembolic ischemic stroke
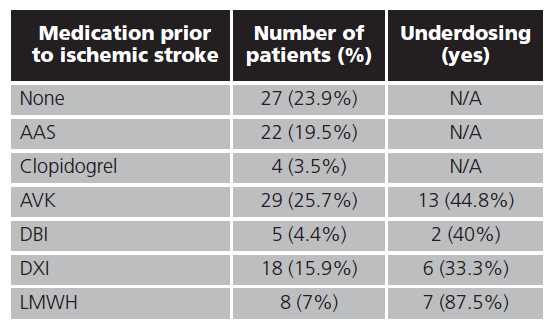
AAS: acetylsalicylic acid; DXI: direct Xa inhibitor; AVK: anti-vitamin k anticoagulants; LMWH: low-molecular-weight heparin; DBI: direct thrombin inhibitors; N/A: not applicable.
Table 3. Modifications made to the preventative treatment strategy
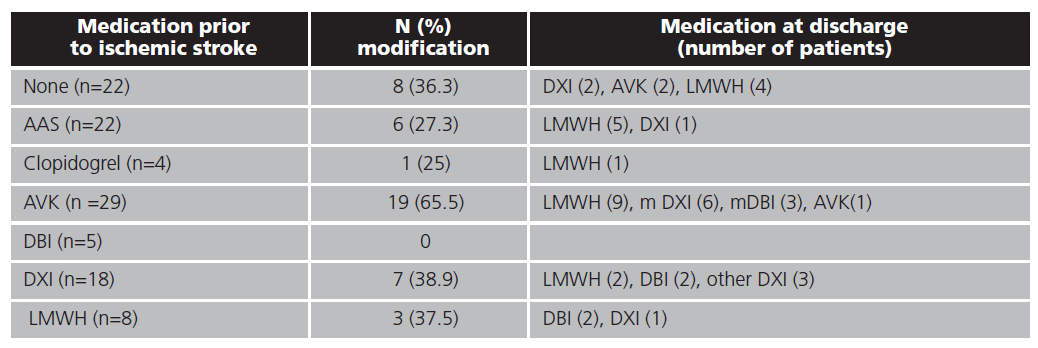
AAS: acetylsalicylic acid; DXI: direct Xa inhibitor; AVK: anti-vitamin k anticoagulants; LMWH: low-molecular-weight heparin; DBI: direct thrombin inhibitors.
Tabla 4. Results of the univariate and multivariate analyses
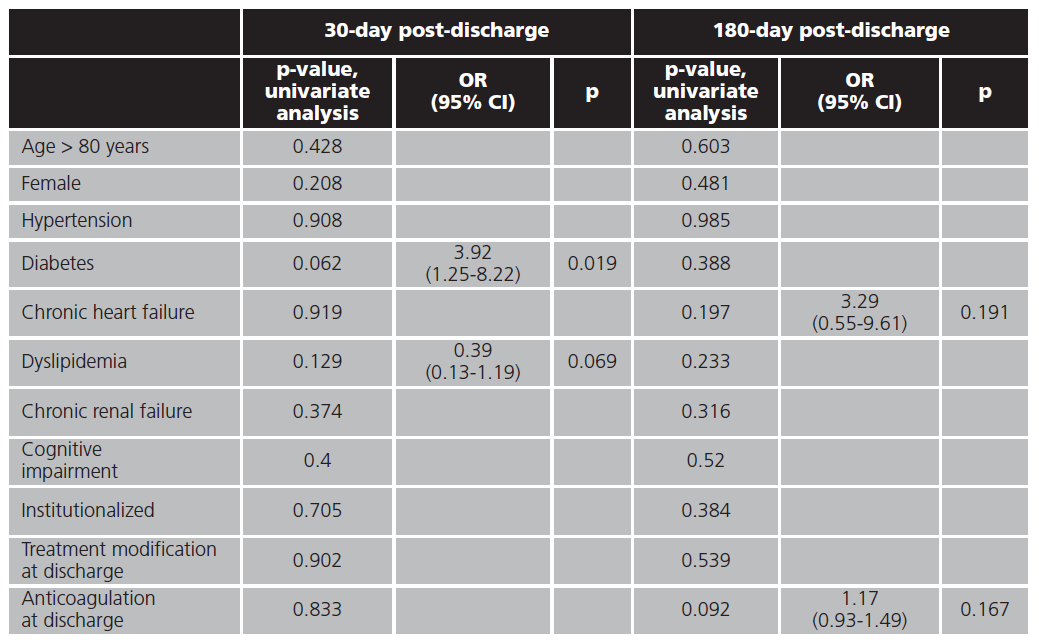
OR: odds ratio; CI: confidence interval.
In our cohort of patients who presented to the ED with cardioembolic ischemic stroke associated with undertreated AF (DRP-related stroke), we found that the risk of early and late ED consultations for any cause did not decrease after switching to another anticoagulant treatment. Nearly 18% of the sample returned to the ED within 30 days for any cause, a slightly lower percentage than observed in other DRP-related visits to the ED among frail patients in our setting. Other studies have found slightly higher rates of second ED consultations at day 30 in patients with different conditions. For example, one study found that 27.5% patients with gastrointestinal bleeding revisited the ED within 30 days of discharge15, while another study found that 27.9% of those with constipation associated with high anticholinergic burden did so16. In a study involving patients with high therapeutic complexity at discharge, 34.8% presented within 30 days of discharge17.
Our findings suggest that pharmacists could play an essential role within a multidisciplinary team in primary and secondary prevention of DRPs associated with ED visits in frail patients. In cardioembolic ischemic stroke, studies have shown that pharmaceutical care programs improve adherence to anticoagulant therapy18, quality of life after ischemic stroke19, and resolve DRP in these patients20. Our data strongly suggest that patients with diabetes should be prioritised in secondary prevention programs for DRP-related strokes.
This study shows the consequences associated with the non-use or underuse of anticoagulant therapy in frail patients. Traditionally, the focus of multidisciplinary pharmaceutical care programs in elderly patients has been to minimise the risks of safety-related DRPs. Our findings highlight the importance of approaching rational drug use in its three dimensions: necessity, effectiveness and safety, regardless of the type of patient population.
Study strengths and limitations
The main limitation of this study is the single-centre study design, as the findings may not be generalizable to centres located in other regions or countries due to differences in healthcare services, the management of chronic patients in primary care, and in access to certain medicines. All of these differences could influence treatment outcomes in other settings. However, our results are consistent with other studies that have reported underuse of anticoagulant drugs in elderly patients in different health care systems6. The main strength of this study is that it is, to our knowledge, the first to specifically assess the proportion of patients admitted to the ED for cardioembolic stroke associated with untreated or undertreated AF.
CONCLUSIONS
The findings of this study show that most patients (71.6%) with a previous diagnosis of AF who presented at the emergency department for cardioembolic ischemic stroke had not received the optimal anticoagulant preventive treatment. Diabetes was the only risk factor significantly associated with early revisits to the ED in this study population. No other risk factors associated with ED readmission at 30 or 180 days were observed.