Meu SciELO
Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Pharmacy Practice (Granada)
versão On-line ISSN 1886-3655versão impressa ISSN 1885-642X
Pharmacy Pract (Granada) vol.4 no.1 Redondela Jan./Mar. 2006
|
Original Research |
Electronic prescription as contributing factorfor hospitalized patients' safety
Prescripción informatizada como factor contribuyente
para la seguridad de los pacientes hospitalizados
Fernanda R.E. GIMENES, Adriana I. MIASSO, Divaldo P. de LYRA JUNIOR, Cris Renata GROU.
|
ABSTRACT* The following study was performed to identify factors related to medication errors in the computerized physician order entry and their advantages and disadvantages according to doctors, nursing team and administrative officers. It is a survey descriptive study carried out at three units of a Brazilian academic hospital in the southeast area. The study was divided in two phases. In the first phase, we analyzed a total of 1,349 prescriptions from general medical unit, surgical and orthopaedic wards during 30 days consecutively. A semi-structured instrument, elaborated by a group of researchers for the study proposals, was used. In the second phase, a semi-structured questionnaire was applied to the health professionals containing closed and open items approaching their opinion about the composition of electronic prescription, the advantages and disadvantages of them, and their suggestions for its improvement. Out of 1,349 prescriptions observed, 17.5% presented deletions, 25.0% medicines written manually and 17.0% of them were incomplete. Some of the advantages pointed by health professionals were its legibility (37.5%), little time spent when elaborating and emitting them (20.5%) and the way they are a practical and organized (8%). The disadvantages pointed were repetition of previous prescriptions (34%), typing mistakes (17%), dependence on computers (11%) and alterations made manually (7%). We conclude, this way, that the computerized prescription order entry represents a great progress among the strategies used to minimize medication errors caused by prescriptions badly formulated. However, it doesn't eradicate the possibility of medication error occurrences, needing some system modifications. Key words: Medication errors. Computerized physician order entry. Patients safety. |
RESUMEN El presente estudio se realizó para identificar factores relacionados con los errores de medicación en las recetas informatizadas y sus ventajas y desventajas según los médicos, enfermeras y personal administrativo. Es un estudio descriptivo realizado en tres unidades de un hospital universitario del suroeste de Brasil. El estudio se dividió en dos fases. En la primera fase, analizamos un total de 1349 prescripciones de los servicios de medicina general, cirugía y ortopedia durante 30 días consecutivos. Se utilizó un instrumento semi-estructurado, elaborado por un grupo de investigadores para este estudio. En la segunda fase, se aplicó un cuestionario semi-estructurado a los profesionales de la salud, que contenía preguntas abiertas y cerradas sobre sus opiniones sobre la prescripción electrónica, sus ventajas y desventajas, y sus sugerencias para mejorarla. De las 1349 prescripciones observadas, el 17,5% presentaban correcciones, el 25,0% estaba escrita manualmente y el 17,0% estaba incompleta. Algunas de las ventajas señaladas por los profesionales de la salud era su legibilidad (37,5%), poco tiempo empleado en elaborarla y emitirla (20,5%) y el modo práctico en que se organizaban (,0%). Las desventajas que se señalaban fueron la repetición de prescripciones previas (34,0%), los errores tipográficos (17,0%), la dependencia de los ordenadores (11,0%) y las alteraciones hechas manualmente (7,0%). En conclusión, la prescripción informatizada representa un gran progreso entre las estrategias utilizadas para minimizar los errores de medicación producidos por prescripciones mal formuladas. Sin embargo, no erradica la posibilidad la aparición de error, necesitándose algunas modificaciones. Palabras clave: Errores de medicación. Prescripción informatizada. Seguridad del paciente. |
* Fernanda R. E. GIMENES. Nurse, Ribeirão Preto Nursing School, University
of São Paulo (EERP-USP), Brazil,
WHO Collaborative center for Nursing
Research and Development.
Adriana I. MIASSO. Nurse, Ribeirão Preto Nursing School, University of
São Paulo (EERP-USP), Brazil.
Divaldo P. de LYRA JUNIOR. MSc (Pharm). Ribeirão Preto Nursing School,
University of São Paulo (EERP-USP), Brazil.
Cris R. CROU. Nurse, Ribeirão Preto Nursing School, University of São
Paulo (EERP-USP), Brazil.
INTRODUCTION
The number of patients been harmed by medication is perceived to be a problem, and it is clear that adverse drug events appear to represent an epidemic.1 The Institute of Medicine (IOM) 1999´s report estimates that about 44,000 to 98,000 Americans die in any given year from medical errors that occur in hospitals and 7,000 due to the medication errors.2 Ever since, many studies have been developed with the intention of minimizing the risks for these errors and seeking the quality of care rendered to the patients and their safety.
In England, about 85.000 medication errors were registered by the National Health Service.3 A study developed in United Kingdom identified, from 3,141 (15%) prescription order, one or more errors.4 Another recent work realized at 36 American hospitals detected 19% errors.5 Studies realized in Colorado, Utah and New York identified several adverse events in the hospitalized patient, half of them could be prevented.6
The medication errors are divided in prescription stages, dispensing and administration and all phases of the process are susceptible for errors.3,7 However, Winterstein et al (2004) showed that 72% of the medication errors were initiate during prescription, followed by administering (15%), dispensing (7%) and transcribing (6%).8
In Brazil, little is known about the theme. Few articles were published on some punctual aspects of the problem and it does not exist a public or private institution who take care of these matters.9 Those studies demonstrate the presence of information deletions (18%), abandoned medicines (17%) and no information about pharmaceutical form, frequency (9%) and administration route (82%).10
According to Bates (2000), computerized prescription order entry (CPOE) can enlarge the safety of the medicines because they are more structured, legible and a lot of information can be supplied to the prescriber during the prescription process.11 In addition, they make possible that errors be corrected at the moment they are typed with no need of deleting or scribbling. However, less than 5% of all prescriptions are currently processed entirely electronically.12
So, the objective of this paper is to identify factors related to medication errors in computerized prescription order entry and to identify their advantages and disadvantages according to physicians, nursing team and administrative officers.
METHODS
In the present article a descriptive survey study was developed in three units (general, surgical and orthopaedic clinics) of an academic hospital in the Brazilian southeast area. This institution was chosen by possessing bond with state public university and for belonging to the Rede Sentinela of ANVISA (Brazilian National Health Surveillance Agency). ANVISA is an institution that provides workshops to physicians, nurses, pharmacists and hospital managers about medication errors made during prescription, preparing and administering drugs. Furthermore, a Sentinela Hospital Net was created as a kind of national net pilot test, which has more than 100 hospitals involved. Those hospitals were chosen for having a larger number of medical residence programs per state. Adverse drug events notification is incited to get as many information as possible, so the government is able to regulate medication commerce.
Data collection was divided in two phases and it begun after the local ethic committee had approved the study. It happened in July 2001 in the medical and orthopaedic clinics and in July 2002 in the surgical ward. Data were collected next to the Nursing staff and always at the end of the afternoon since, in this institution, the prescriptions begin to be worth from 16 o'clock.
In the first phase, direct observation was made upon medical order to get the information presented on them, such as presence of the drug name (generic or brand), pharmaceutical form, dose, frequency or schedule, administration route, presence of abbreviations and deletions. The sample was composed by 535 prescriptions in the general medical unit, 424 in the surgical clinic and 390 in the orthopaedic ward, and they were revised for 30 consecutive days, excluding weekends. A structured instrument was elaborated for the study whose content was composed by items related to the composition of the prescription.
In the second phase, the sample was composed by 84 health care professionals among doctors, nurses, technicians and nursing auxiliaries, as well as administrative officers. A semi-structured questionnaire was applied to the professionals containing questions about their opinions concerning prescriptions composition, the advantages and disadvantages of electronic order, as well as their suggestions for its improvement.
RESULTS AND DISCUSSION
Phase I: Revision of the electronic prescription
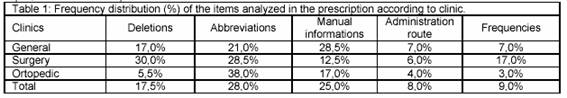
Out of 1,349 prescriptions observed, 17.5% presented deletions, which was more frequent at the surgical clinic (30.0%), followed by general medical unit (17.0%), and orthopaedic ward (5.5%). Such deletions were characterized by modifications made on prescription and they included scribbling or circles around the drug name, dose or frequency. This difference may be justified for the fact that in the first two units, patients are more complex, being more vulnerable to the modifications in their health condition. So, the prescriptions tend to be modified more frequently. In spite of that, the presence of deleted items can lead to misunderstanding information presented on prescriptions that, contributing to the occurrence of the error.13
Although the medical order is computerized, the system allows the presence of abbreviations as BIC (computerized bomb infusion), ACM (according to medical device), PMV (to maintain vein), 1 med. (a measure); incomplete sentences that don't give clear information (to "give in alternate days") and use of decimal points (100.00 ml). We must remind that, in our hospital, the dose prescribed as "1 med" is allowed, but there is not standardization, remaining the question: how much is a measure?
The occurrence of these cases, in the general medical unit was 21%, in the surgical unit was 28.5% and, in the orthopaedic ward, 38%. Such problems may generate doubt in the professionals who prepare and administer drugs. Studies affirm that the medical orders should not contain abbreviations, once they may cause doubts in the other professionals and, consequently, lead to error.14,15 The difficulty on interpreting the pharmaceutical forms writing manually doesn't allow the distinction, for instance, from comp (tablets) x amp (flask); caps (capsules) x comp (tablets); sup (suppositories) x susp (suspension), which could take to the incorrect route and/or wrong drug administration technique.16,17 The use of abbreviations like "U" for "units" is problematic, for example, a dose of heparin 100U is even more likely to be misread as 1000 units when there is no space between the numerical dose and the abbreviation "U".18 In those cases, a possible substitution of the pharmaceutical forms, in the dispensation, could implicate in the modification of several pharmacokinetic factors, especially in the medicine absorption, that depends on drug solubility.19 It would be appropriate for prescriber to avoid it or make use of those standardized by the institution.
It is worth to point out that the current system allows the physician to prescribe medicines manually; especially when patients general state is altered, needing new drugs to be prescribed or to be abandoned. Out of 1.349 prescriptions, 25.0% presented medicines written manually. However, not always this information is readable. As Cohen et al (1994) affirmed that 50% of the manual prescriptions request extra time to interpret them due to the illegible letter and that the costs of the extra care related to this factor can be assessed by time spend for the nursing team, secretaries, other physicians, pharmacists and other professionals.20 The risk for medication errors is increased if health care professionals are not able to read the prescriptions correctly.14 Besides, when nurses and pharmacists get used to common indications, dosing and frequency for an established medication, they can fall into the trap of quickly reading an order and assuming it is correct when it´s really unclear or questionable.21 Kalmeijer et al (2003) they also affirm that manual prescriptions contribute significantly as the potential mistakes of medication related the illegibility, abbreviations no conclusive of the name of the medicine, lack of information, etc.22
Regarding the composition of the medicines, there were not mistakes in none of the studied units. That is justified for the fact that the names of the drugs prescribed are standardized by the institution (generic name) and recorded in the computer system. The standardization of drug name is of extreme importance what concerns to the minimization of the risks for medication error. Example of that is the case of the "cisplatin" related by Cohen (1999) where a patient developed hearing loss and acute renal failure after an excessive dose due to confusion in reading the drug name and dose, what could be avoided if the physician had prescribed it using generic name instead of the brand name.18
When analyzing the presence of information about administration route and schedule (or frequency), the resulted pointed was 30.0% at the surgical clinic, 14.0% in the general medical clinic and 7.5% in the orthopaedic. This means that 231 (17.1%) prescriptions didn't contain a piece of information or the other. Incomplete prescriptions increase risks for medication errors because logical but incorrect assumptions can be made about the missing information. In addition, this increases the time devoted to connections for elucidation.23 Computerized systems should present a program that impedes the prescribers of elaborating prescriptions with absence of information (Table 1).
Phase II: Professionals and users opinions
In this phase, the data of the three clinics were classified in agreement with the similarity of the answers. Out of 84 professionals that accepted to participate in the study, 14 were physicians or residents, 17 nurses, 40 nursing auxiliaries, 5 nursing technicians and 8 administrative officers.
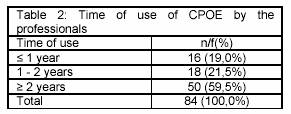
Regarding the time of use, it was observed that 59,5% of the professionals have been using CPOE for more than two years, as it is demonstrated in the Table 2.
Out of 69 professionals that referred errors in the prescription, 43 related dose errors, 49 in the administration route, 31 in the frequency, 7 in the drug name when prescribed manually and there was more 7 references to other problems such as abandoned medicines which are not communicated to the nursing staff, errors involving dose calculation and repetition of previous prescriptions, even when a medication was already abandoned.
It is worth to remind that in the period of data collection, the system didn't have alarms to alert prescribers for errors made at the moment of typing. Systems which have those alarms are efficient in minimizing the occurrence of errors, because when the doctor types incongruous information, a warning appears in the screen of the computer making possible the mistakes correction.
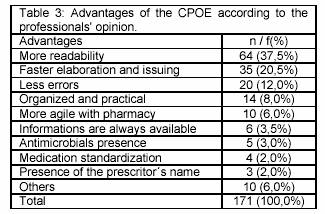
Some of the advantages were pointed by health care team. 64 professionals mentioned the easiness in reading electronic orders; 35 mentioned the speed with that is made and delivered; 20 informed errors decreasing; 14, the way informations are organized through printed paper; 10 referred the agility with pharmacy; 6, the possibility of the data stay filed by long periods of time; 5 told the inclusion of the antimicrobials records; 4, the standardization of the medicines; 3, the presence of the prescriber´s name (Table 3).
As we can observe, the legibility of the electronic prescriptions was pointed as the main advantage, besides they are more complete. It can eliminate the illegibility of the letter promoting safety in dispensing phases, preparation and administration of drugs.5 Kalmeijer et al (2003) also appeared as advantages these subjects: more readable prescriptions and complete, faster and efficient, larger accessibility to the patient's data.22
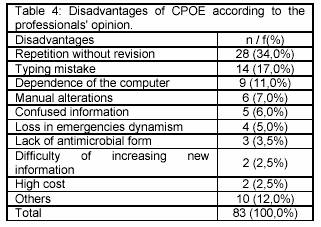
The disadvantages of the electronic medical prescription, according to the professionals, are present in the Table 4.
Although electronic prescriptions mean a great progress among the strategies created to minimize the risks of medication errors, yet other errors may occur. Thus, it is necessary to provide doctors and residents a larger understanding about the importance of the training program for use of the system, with the objective of limiting the consequences of adverse drug events due to prescriptions badly formulated.13 With the implementation of this system more elaborated and with a larger education on the part of those than they prescribe will be possible to turn the most detailed and easy prescriptions of they be understood by the professionals that handle them.
CONCLUSION
Data obtained in the first phase show us presence of deletions, abbreviations and absence of information such as administration route, frequency and presence of medicines written manually.
Regarding the professionals' opinion, it was verified that great part of them identified mistakes concerning CPOE which demonstrate that computerized system does not eradicate the possibility of occurrence of medication error. However, several advantages were pointed: its legibility, they are more practical and organized, less time spent when elaborating and emitting, and others.
Therefore, electronic prescription represents a great progress among the strategies used to minimize current errors related to illegible prescriptions and to those badly formulated. However, some modifications in the system are necessary for improving the existing ones. Adverse drug events may be reduced by the success of the programs implementation, improving the quality of the care.
FINACIAL SUPPORT
CNPq and FAPESP
|
References |
1 Dean B. Adverse drug events: what´s the truth? Qual Saf Health Care 2003; 12(3): 165-6. [ Links ]
2. Kohn LT, Corrigan JM, Donaldson MS, eds. To err is human: building a safer health system. Washington, DC: National Academy Press, 1999. [ Links ]
3. Timbs, O. Leading role for pharmacists to reduce drug errors and improve patient safety. Pharm J 2002, 268(7190): 392. [ Links ]
4. Ridley AS, Booth SA, Thompson CM. Prescription errors in UK critical care units. Anaesthesia 2004; 59: 1193-200. [ Links ]
5. Barker KN, Flynn EA, Pepper GA, Bates DW, Mikeal RL. Medication errors observed in 36 health care facilities. Arch Intern Med 2002; 162:1897-1903. [ Links ]
6. Berger RG, Kichak J, PCHAK, BA. Computerized physician order entry: helpful or harmful? J Am Med Inform Assoc 2004;11:100–3. [ Links ]
7. Allard J, Carthey J, Cope J, Pitt M, Woodward S. Medication errors: Causes, prevention and reduction. Br J Haematol 2002; 116(2): 255-65. [ Links ]
8. Winterstein AG, Thomas E, Rosenberg EI, Hatton RC, Gonzalez RR, Kanjanarat P. Nature and causes of clinically significant medication errors in a tertiary care hospital. Am J Health Syst Pharm 2004; 61(18): 1908-16. [ Links ]
9. Rosa MB, Perini E. Erros de medicação: quem foi? Rev Assoc Med Bras 2003; 49(3): 335-41. [ Links ]
10. Cassiani SHB, Freire CC, Gimenes FRE. Computerized physician order entry in a university hospital: writing failure and user´s opinios. Rev Esc Enferm USP 2003; 37(4): 51-60. [ Links ]
11. Bates DW. Improving medication safety across institutions. Journal on Quality Improvement 2000; 26(6):319-20. [ Links ]
12. Howell S. e-Rx systems seek to improve care. Quality Indicator, Pharmacy Resource 2000; 3(4), 3-7. [ Links ]
13. Cassiani SHB, Freire CC, Gimenes FRE. Computerized physician order entry in a university hospital: writing failureand user´s opinions. Rev Esc Enferm USP 2003; 37(4): 51-60. [ Links ]
14. Winslow EH, Nestor VA, Davidoff SK. Thompson PG, Borum JC. Legibility and completeness of physicians´ handwritten medication orders. Heart Lung 1997; 26:158-64. [ Links ]
15. Bates DW et al. The impact of computerized physician order entry on medication errors prevention. J Am Med Inform Assoc 1999; 6 (4): 313-21. [ Links ]
16. Vaida AJ, Peterson J. Incomplete directions can lead to dispensing errors. Pharmacy Times 2002; 5: 34-8. [ Links ]
17. Marques FB. Erros de medicação. Revista Informação Terapêutica 2000; 4: 3-5. [ Links ]
18. Cohen M. Letter and number characters that run together may lead to serious errors. Int Pharm J 1999; 13(3):108-9. [ Links ]
19. Lyra Junior DP, Prado MC, Abriata JP, Pelá IR. Recetas médicas como causantes de riesgo de problemas relacionados con medicamentos. Seguimiento Farmacoterapeutico 2004; 2 (2): 86-96. [ Links ]
20. Cohen MR, Senders J, Davis NM. Failure mode and effects analysis: a novel approach to avoiding dangerous medication errors and accidents. Hosp Pharm 1994; 29 (4): 319-30. [ Links ]
21. Lilley LL, Guanci R. Unfamiliar drug uses. Am J Nurs. 1995, 95(1):15. [ Links ]
22. Kalmeijer MD, Holtzer W, Dongen R, Guchelaar HJ. Implementation of a computerized physician medication order entry system at the Academic Medical Centre in Amsterdam. Pharm World Sci 2003; 25(3): 88–93. [ Links ]
23. Lesar TS, Briceland LL, Delcoure K, Parmalee JC, Masta-Gornic V, Pohl H. Medication prescribing errors in a teaching hospital. JAMA 1990; 263 (17): 2329-34. [ Links ]











 texto em
texto em