Meu SciELO
Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Pharmacy Practice (Granada)
versão On-line ISSN 1886-3655versão impressa ISSN 1885-642X
Pharmacy Pract (Granada) vol.4 no.2 Redondela Abr./Jun. 2006
|
Original research |
Private pharmacy staff in Hanoi dispensing steroids - theory and practice
Personal de farmacias privadas de Hanoi dispensando corticoides - teoría y práctica
Mattias LARSSON, Nguyen Thanh BINH, Göran TOMSON, Nguyen
TK CHUC, Torkel FALKENBERG.
|
ABSTRACT Objective: To investigate self reported practice and actual practice
of private pharmacy staff in relation to drug regulations and provision
of prednisolone (a prescription-only corticosteroid) on request to treat
lower back pain. Key words: Corticosteroid. Simulated Client. Good Pharmacy practice. Pharmacy Staff. Knowledge. Vietnam. |
RESUMEN Objetivo: Investigar la práctica auto-comunicada y la práctica
real del personal de las farmacias privadas en relación a la regulación
sobre medicamentos y provisión de prednisolona (un corticoide de
prescripción) solicitado para tratar un dolor lumbar. Palabras clave: Corticoides. Cliente simulado. Buenas prácticas de farmacia. Personal de farmacia. Conocimiento. Vietnam. |
Mattias LARSSON, MD, PhD. Division of International Health (IHCAR), Department
of Public Health Sciences, Karolinska Institutet, Stockholm, Sweden.
Nguyen Thanh BINH. Pharmacist. Hanoi College of Pharmacy, Hanoi, Vietnam.
Göran TOMSON. MD. Professor. Division of International Health (IHCAR),
Department of Public Health Sciencies, Karolinska Institutet, Stockholm, Sweden;
and Medical Management Centre (MMC), Karolinska Institutet, Stockholm, Sweden.
Nguyen TK CHUC. PhD. Ass. Professor. Hanoi Medical University, Hanoi, Vietnam.
Torkel FALKENBERG. PhD. Division of International Health (IHCAR), Department
of Public Health Sciences, Karolinska Institutet, Stockholm, Sweden.
INTRODUCTION
In many low-income countries, health care reforms and privatization have increased the availability of drugs for lay people through private pharmacies. The private provision of drugs has, however, frequently been associated with inequitable affordability, impaired rational use and substandard drug quality. Effective regulatory framework is therefore a major opportunity and challenge.1,2 Although regulations commonly exist, the regulatory authorities often lack resources for effective implementation and enforcement, limiting their ability to influence private sector activity.1,3 Little work has been done to assess the compliance of regulations as well as exploring how, and to what extent, regulations fail.
Vietnam has been progressive in dealing with basic health problems, and has achieved a comparably low infant mortality rate and high life expectancy.4,5 In the late 1980s, there were shortages of drugs after a period of isolation from the international community and a costly post-war reconstruction.6 In 1986, an economic reform, the Doi Moi renovation towards market economy, was initiated. The pharmaceutical industry and drug retail business were liberalized. Pharmacists were allowed to open retail pharmacies, and the pharmaceutical market shifted from publicly financed to private enterprise. Between 1986 and 1994, there was a six-fold increase in per capita drug consumption.7 The number of private pharmacies increased from none in 1986 to more than 6000 in 19968 and currently acts as the first line medical care providers, a situation also found in other low-income countries.9-11 Hence the quality of pharmacy service is of great public health importance. The formulation of both the Tokyo declaration of Good Pharmacy Practice (GPP) in 199312 and the GPP Guidelines issued by WHO in 199413 attest to their importance.
In Vietnam, a prescription and drug dispensing regulation has been in place since 1995 and includes detailed information regarding prescription-only drugs, which includes all corticosteroids and all but 8 antibiotics.14 A drug policy was adopted 1996 and includes paragraphs regarding rational use of drugs.15 The private pharmacies are obliged to continuously stay updated and comply with the current regulations. However, several studies in Vietnam and other low-income countries have found that pharmacy customers commonly request specific drugs and that the pharmacies dispense prescription-only drugs such as corticosteroids and antibiotics, often without any questions.9-11,16-19 Hence the ability of the pharmacy staff to deal with drug requests is important.
Corticosteroids are an important group of drugs used mainly for two purposes: (i) replacement therapy in patients with adrenal gland deficiency; (ii) immunosuppressive and anti-inflammatory therapy. When indicated, they may be lifesaving, such as for patients with anaphylactic shock or life expanding as for patients with autoimmune diseases. However, there are serious adverse effects of steroid use such as peptic ulcers, immuno-suppression and metabolic effects on water and electrolyte balance, muscle wasting, osteoporosis, hyper-glycaemia, hypertension-increased fatty tissue (moon face and buffalo hump), all part of Cushings syndrome.20,21 For most infectious diseases, steroid use is contraindicated, as steroids tend to disguise inflammatory symptoms, giving a subjective feeling of improvement, while in fact the immunosuppressive effect decreases the ability of the infected person to fight the invasive organism.20 It has been found that corticosteroids are commonly irrationally used for health problems like diarrhoea, fever, jaundice and lower back pain in low and middle-income countries.19,22 Due to the severe adverse effects, most countries, including Vietnam, have chosen to restrict the availability of steroids through prescription-only regulations.
In this study we have assessed private pharmacy self reported practice and actual practice in relation to dispensing of prednisolone on request for treatment of lower back pain. This tracer condition was used to assess compliance with prescription regulations as well as determining the current level of rational dispensing of corticosteroids in private pharmacies in Hanoi. Most episodes of lower back pain are mechanical in origin, associated with muscle strain and resolve naturally within 1 to 2 weeks. The pain can in most cases successfully be relieved with paracetamol, NSAIDs including diclofenac and ibuprofen23 as well as with acupuncture24, whereas corticosteroids are not indicated. This study was part of the European Union supported Towards Good Pharmacy Practice in Thailand and Vietnam, a randomised controlled trial aiming to improve dispensing of prescription only steroids and antibiotics as well as case management of Acute Respiratory Infections and Sexually Transmitted Diseases.
METHODS
Study population: The study was conducted in the urban area of Hanoi with 789 private pharmacies, pharmacies located in hospitals and wholesalers were excluded. From the list of the remaining 641 pharmacies, 60 pharmacies were randomly selected by computerized randomization using the Excel program. This paper reports baseline data from a randomized-controlled trial where the pharmacies are the unit of analysis. Analysis is also done at the level of individual simulated client encounters (SCM) client encounters in the pharmacies.
Questionnaire: Interviews of pharmacy staff at the selected pharmacies were conducted with a semi-structured questionnaire containing mainly multiple choice and a few open-ended questions regarding dispensing of prescription-only drugs including prednisolone. The interviews aimed to get the respondent to state how they would manage a client requesting prednisolone to treat lower back pain. Questions included: "My back is aching. Could I have 2, 3, 4 or 5 tablets of prednisolone please? If they did not offer to ask questions or give advice, the interviewer would prompt with would you ask any questions? or would you give any advice?. The interviewees were aware that they were answering a survey. Four interviewers, two pharmacists, one medical doctor and one sociologist, were trained through role-play on how to conduct the interviews. All sixty pharmacies were visited by one of the interviewers and all the staff working (mostly one) at the pharmacy at the time of the visit where interviewed. The answers were coded and entered into the computer by using the program Epi Info 6 (a computer program for processing and analyzing epidemiological data). The interviews took place after all the simulated clients visits had been completed.
The Simulated Client method (SCM) was used to measure provider behaviour and was used before the questionnaire survey to avoid contaminating the SCM results. Research assistants with fictitious case scenarios visited the selected pharmacies and requested their assistance. SCM has frequently been used to assess practice in both low and high-income countries.9,10,24-26 In this methodology, the simulated clients present complaints to pharmacy staff and purchase the drugs recommended. To avoid attention and recognition by pharmacy staff, five different clients visited all the pharmacies simultaneously according to a prearranged rotating schedule. All clients were trained to act in a reproducible way. A specific recording sheet for the clients containing information regarding the drugs, questions and advice was developed. Five female assistant pharmacists from Hanoi College of Pharmacy were selected as simulated clients and trained to act according to the client scenario. Each simulated client encountered all 60 pharmacies, presented the scenario complaining about lower back pain, asking for a few capsules of prednisolone without providing a prescription (Table 1), bought the recommended drugs and within 15 minutes recorded the events in the record sheet. A total of 295 encounters were conducted. Data on 5 encounters were not collected since the pharmacies were closed at the time of the visit. The simulated clients submitted the drugs purchased and the record sheets to the research staff at the College of Pharmacy in Hanoi. Drugs were classified according to the Anatomical Therapeutic Chemical (ATC) classification, an instrument for classification of drugs adopted by the World Health Organisation and whether they were prescription-only drugs or over the counter (OTC) drugs, according to Vietnamese regulations.
The results were coded and entered into a computer using "Microsoft Access 1998 and the Statistical Package for Social Sciences for Window Software (SPSS) version 9.0 (a software for data processing and statistical analysis). The pharmacies are the unit of analysis for SCM and questionnaire data as well as for comparisons between SCM and questionnaire data. Analysis of SCM data is also done at the level of individual SCM client encounters at the pharmacies. Statistical analysis was performed with chi square, Wilcoxon and a 2-tail t-test to determine group differences.
The study was planned and conducted in collaboration with the Ministry of Health (MoH), the Hanoi Health Bureau and the Hanoi Pharmacy Association, who were formally responsible for the study. Informed consent from the individual pharmacy staff was not obtained in advance, as this could have seriously impaired the results by introducing observation and selection bias.25 There were no punishments for those private pharmacy staff members who acted against the regulations. The pharmacies were coded and the results are provided as group averages. One important reason for using SCM was that the potential harm of the low quality of pharmacy practice, including the frequent irrational provision of drugs, was considered by the national health authorities to be an increasing problem.
RESULTS
Self reported practice assessed with questionnaire interviews
Seventy interviews were performed in the 60 pharmacies, in ten pharmacies there were 2 staff members present who both were interviewed (table 2).
In response to the question "Have you ever had a customer who asked for some tablets of corticosteroids" 86% of the interviewees stated yes. The majority, 60% of the pharmacy staff interviewed, said that they would not dispense corticosteroids on request without prescription. The reasons mentioned are shown in Figure 1. Of the 40% who stated that they would dispense, 90% justified this by saying that they wanted to comply with the clients request, and 3% that "otherwise other pharmacies would sell the drugs". In 2 of the 10 pharmacies with two staff interviewed, one of the staff stated that they would dispense and the other that they would not.
Regarding knowledge of adverse effects, 43% mentioned osteoporosis, 41% peptic ulcers, 16% edema, 9% immune defence inhibition and 9 % muscle wasting. Moon face (4%), high blood pressure (3%) and mental disturbance (3%) were also mentioned.
Pharmacy staff practice assessed with SCM
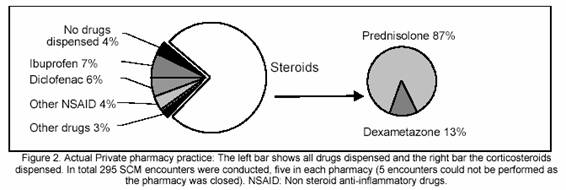
All but one pharmacy (98%) dispensed corticosteroids. 16 pharmacies (27%) dispensed in all 5 encounters, 26 pharmacies (43%) dispensed in 4 encounters, 9 (15%), 3 (5%) and 5 (8%) pharmacies dispensed in 3, 2 and 1 of the encounters, respectively. In total, corticosteroids were dispensed in 76 % of all the encounters. In only three encounters (1%) did the pharmacy staff ask for a prescription. Drugs dispensed are shown in figure 2.
In the encounters, where questions were asked and advice given there were significantly less steroids dispensed, 66 % and 64% respectively (table 3 and 4), compared to the encounters where no questions were asked (82%) and no advice given (91%).
Questions were asked in 41% of the encounters with an average of 1.15 questions per encounter (table 3). Questions related to significantly less dispensing (p<0.01) were: questions related to back-pain; previous use; alternative treatment with other analgesic drugs; who had advised you to buy and; why do you want to take prednisolone (table 3). Questions related to significantly more dispensing (p<0.05) were: stomach problems and if they just wanted the requested amount of tablets.
Advice was given in 57% of all the encounters with an average of 1.47 advices per encounter (table 4). Advice related to significantly less dispensing (p<0.01) were: not to use corticosteroids; use other drugs; visit a doctor; take before meals; and to use massage. Advice related to significantly more dispensing (p<0.05) were: information about adverse effects (4% of the encounters) and recommended to take the drug at least 5-7 days.
Comparison between self reported practice and actual practice
There was a significant difference (p<0.001) between stated (questionnaire) dispensing (40%) and actual dispensing (98% of the pharmacies in 76% of all the encounters). Pharmacies stating they would not sell dispensed significantly (p<0.001) less corticosteroids, in 70% of the encounters, compared to the pharmacies stating that they would sell which dispensed in 84% of the encounters. All pharmacies that justified not dispensing by saying, that it is against the regulation, nevertheless did so in practice in at least one encounter.
DISCUSSION
Corticosteroids were dispensed by all but one pharmacy on average in 76 % of the encounters and prescription requests were only recorded in 1% of the encounters. This was done despite that 60% stated during interviews that they would not dispense steroids on request without prescription. A decree regulating prescribing, stating that all corticosteroids are prescription-only drugs, has been in place since 1995.28 Clearly this shows that the regulations regarding prescriptions are generally not respected. Several studies have shown that prescription-only drugs are commonly dispensed without prescription in Vietnam and other Asian countries.10,11,17,18 In a Brazilian study clients asked for corticosteroids; the pharmacies complied with the request in 65% of the encounters.19
The effectiveness of regulation is strongly influenced by the socioeconomic context.1,2 Determinants such as customers expectations, social acceptance, commercial pressures and profit needs may have more impact on actual practice compared to regulations and clinical indications.29,30 As the number of pharmacies has grown dramatically in Vietnam competition has increased and profit margins decreased.4 Pharmacy staff may feel compelled to focus more on profit than on their professional role.29-31 The potential risk of not complying with the regulation might not be enough of a deterrent, especially if economic margins are small. In Vietnam, the control needed to implement regulations has been lacking, due to weak and not clearly defined sanctions for violations as well as few incentives for officials and inspectors to focus on the issue.32-34 This has also been described in other low-income countries.3,29 In Lao PDR, the regulatory system was not able to deal with the existence of dangerous, fake or substandard drugs.1 In Vietnam, an enforcement system including sanctions is being developed.33
The difference between stated behaviour and actual practice is often attributed to observation bias.25 This has previously been shown with oral rehydration solution treatment for diarrhoea in Kenya35 as well as in other studies in low-income countries25,27,29,36 showed that even though 74% of private pharmacies in Hanoi stated that they would not treat STD symptoms, 84% still dispensed prescription-only antibiotics and none gave the syndromically correct treatment. This underlines the importance to assess not only self reported practice or knowledge but also actual practice; using a questionnaire by itself would have grossly underestimated the incidence of irrational steroid dispensing.
Asking diagnostic questions such as what kind of back pain do you have and duration of back pain were associated with significantly less dispensing of corticosteroids. Hence strategies to initiate communication in combination with case management training might be important. Much of the pharmacy staff advice was poor and the most common advice, to take after meals, has no relevance. Lack of knowledge about standard treatments and regulations, commercial pressures and a failure to implement the existing regulations has been identified as major factors behind poor pharmacy advise.37 In Vietnam, continuous education among practitioners is often non-existent or depends heavily on information from the representatives of the pharmaceutical companies which tends to be biased.38
Information about adverse effects was only given in 4% of the encounters, although it was mentioned by 60% in the questionnaire. It has been shown that some physicians deny hazardous drug effects, even though they have acknowledged adverse effects during interview.30 The importance of awareness regarding adverse drug reactions is emphasized by the fact that adverse drug reactions now may account for up to 10% of the admissions of patients to internal medicine wards at a cost of hundreds of millions of US dollars annually.39 The extent of disease due to adverse drugs reactions in Vietnam is not known, but might - considering the ubiquitousness of self-medication - be extensive.
Corticosteroids are potent drugs that are useful for many diseases; this is also perceived by the patients.11 The serious adverse effects however justify restrictive use only on correct indications.40 Being relatively cheap, in Vietnam one tablet costs less than 1000 Dong (about 7 cents), corticosteroids could without loss of profit be substituted by less harmful non-steroid anti-inflammatory drugs. Studies in Kenya and Indonesia have shown that it is possible to improve private pharmacy practice through a combination of focused small group training and supporting their self-image as health professionals.35 Multi-faceted interventions including regulatory enforcement and education have been proven effective in public sector29 as well as to improve private pharmacy case management of common diseases and regulatory compliance.33 In addition, empowering consumers to make informed choices must also be taken into account.3 In addition to monitoring of the effects of the enforcement system reform in Vietnam, more research is needed to understand, in more detail, aspects relevant for counter staffs motives for their practices including profit motives, customers demand and commercial pressures.
ACKNOWLEDGEMENTS
First we would like to acknowledge our gratitude for the late Prof. Nguyen
Thanh Do who was the national coordinator of the project. We further would like
to thank the participating private pharmacy staff, the Health Strategy and Policy
Institute, the College of Pharmacy in Hanoi, the Hanoi Medical University, the
Hanoi Health Bureau and the Hanoi Pharmacy Association. The project was financially
supported by the European Union DG XII, INCO-DC, ERB3514PL950674. The WHO Essential
Drugs and other Medicines (EDM) program provided funds for drug purchases. We
thank the drama-pedagogue Katarina Falkenberg for the training of the SCM clients
and Dr. Hiep for organising and monitoring of the SCM process. We also thank
core members of the EU-GPP project, Drs. Yupadee Javrongrit and Sauwakon Ratanawijitrasin
at the Health System Research Institute in Thailand, Prof. Gill Walt and Dr.
John Chalker at the London School of Hygiene and Tropical Medicine as well as
all team members of the EU-GPP consortium for being partners in design and method
development.
|
References |
1. Stenson B, Tomson G, Syhakhang L. Pharmaceutical regulation in context: the case of Lao People's Democratic Republic. Health Policy Plan 1997;12:329-40. [ Links ]
2. Syhakhang L. The quality of private pharmacy services in a province of Lao PDR: Perceptions, practices and regulatory enforcements. (Thesis). Academic. Department, Karolinska Institutet, Stockholm, 2002. [ Links ]
3. Hongoro C, Kumaranayake L. Do they work? Regulating for-profit providers in Zimbabwe. Health Policy Plan 2000;15:368-77. [ Links ]
4. Wolffers, I. The role of pharmaceuticals in the privatization process in Vietnam's health-care system. Soc Sci Med 1995;41:1325-32. [ Links ]
5. World-Bank. Vietnam: Growing Healthy - A Review of Vietnam's Health Sector. World Bank Publications. 2001 [ Links ]
6. Chalker J. Viet Nam: profit and loss in health care. World Health Forum 1995;16:194-5. [ Links ]
7. Witter S. 'Doi moi' and health: the effect of economic reforms on the health system in Vietnam. Int J Health Plann Manage 1996;11:159-72. [ Links ]
8. Phuong D. Towards rational use of antibiotics in Vietnam: present status of infectious diseases in Vietnam. Australian prescriber 1997;20:134-5. [ Links ]
9. Goel P, Ross-Degnan D, Berman P, Soumerai S. Retail pharmacies in developing countries: a behavior and intervention framework. Soc Sci Med 1996;42:1155-61. [ Links ]
10. Tomson G, Sterky G. Self-prescribing by way of pharmacies in three Asian developing countries. Lancet 1986;2:620-2. [ Links ]
11. Kamat, V. R. and Nichter, M. (1998). Pharmacies, self-medication and pharmaceutical marketing in Bombay, India. Soc Sci Med, 47, 779-94. [ Links ]
12. FIP. The Tokyo Declaration : Standards for quality of pharmacy services. Federation Internationale Pharmaceutique. Tokyo, 1993. [ Links ]
13. WHO. Role of the pharmacist in support of the WHO revised drug strategy. Geneva: World Health Organisation;1994. [ Links ]
14. MOH. The third list of essential drugs in Vietnam. Hanoi: Ministry of Health; 1995. [ Links ]
15. MOH. Strategic orientation for people's health care and protection in the period of 1996-2000 and Vietnam's national drug policy. Hanoi(Vietnam): Ministry of Health; 1996. [ Links ]
16. Chuc NT, Larsson M, Falkenberg T, Do NT, Binh NT, Tomson GB. Management of childhood acute respiratory infections at private pharmacies in Vietnam. Ann Pharmacother 2001;35:1283-8. [ Links ]
17. Chuc NT, Tomson G. "Doi moi" and private pharmacies: a case study on dispensing and financial issues in Hanoi, Vietnam. Eur J Clin Pharmacol 1999;55:325-32. [ Links ]
18. Lam L, Tien L, Chuc N, Yen N. Study on rational and safe use of drug in Vietnam. Hanoi: MOH; 1997. [ Links ]
19. Ferraz MB, Pereira RB, Paiva JG, Atra E, Dos Santos JQ. Availability of over-the-counter drugs for arthritis in Sao Paulo, Brazil. Soc Sci Med 1996;42:1129-31. [ Links ]
20. Rang HP, Dale M, Ritter JM. Pharmacology. Churchill Livingstone; 1995. [ Links ]
21. Davidson's. Davidson's Principles & Practice of Medicine. Churchill Livingstone; 1999. [ Links ]
22. Prakash O, Mathur G, Singh Y, Kushwaha K. Prescription audit of under six children living in periurban areas. Indian Pediatr 1998;26:900-4. [ Links ]
23. Borenstein DG. Chronic low back pain. Rheum Dis Clin North Am 1996;22:439-56. [ Links ]
24. Ernst E, White A. Life-threatening adverse reactions after acupuncture? A systematic review. Pain 1997;71:123-6. [ Links ]
25. Madden JM, Quick JD, Ross-Degnan D, Kafle KK. Undercover careseekers: simulated clients in the study of health provider behavior in developing countries. Soc Sci Med 1997;45:1465-82. [ Links ]
26. Bartoloni A, Cutts F, Leoni S, Austin CC, Mantella A, Guglielmetti P, Roselli M, Salazar E, Paradisi F. Patterns of antimicrobial use and antimicrobial resistance among healthy children in Bolivia. Trop Med Int Health 1998;3:116-23. [ Links ]
27. Thamlikitkul V. A correlation of clinical performance on written test and standardised patient. J Med Assoc Thai 1991;74:513-7. [ Links ]
28. MOH. Prescription and dispensing drug regulation No 488. Hanoi: Ministry of Health; 1995. [ Links ]
29. Brugha R, Zwi A. Improving the quality of private sector delivery of public health services: challenges and strategies. Health Policy Plan 1998;13:107-20. [ Links ]
30. Paredes P, de la Pena M, Flores-Guerra E, Diaz J, Trostle J. Factors influencing physicians' prescribing behaviour in the treatment of childhood diarrhoea: knowledge may not be the clue. Soc Sci Med 1996;42: 1141-53. [ Links ]
32. Tran Q. Some results from inspections to private medical and pharmaceutical practices and solutions for fostering the effect and effectiveness of inspections. The State Health Inspectorate, Hanoi: Ministry of Health; 2001. [ Links ]
33. Chuc NTK. Towards good pharmacy practice in Hanoi: A multi-intervention study in private sector (Thesis). Academic. Department, Karolinska Institutet, Stockholm, 2002 [ Links ]
33. Chuc NT, Larsson M, Do NT, Diwan VK, Tomson GB, Falkenberg T. Improving private pharmacy practice: a multi-intervention experiment in Hanoi, Vietnam. J Clin Epidemiol 2002;55:1148-55. [ Links ]
34. Lalvani P, Murray M, Olsson S, Quick J, Tomson G, Wibulpolprasert S. Report of a Ministry of Health/WHO/SIDA. Joint Mission for Development of a Masterplan for the National Drug Policy of Vietnam. WHO and Indevelop Uppsala AB; 1996. [ Links ]
35. Ross-Degnan D, Soumerai SB, Goel PK, Bates J, Makhulo J, Dondi N, Sutoto AD, Ferraz-Tabor L, Hogan R. The impact of face-to-face educational outreach on diarrhoea treatment in pharmacies. Health Policy Plan 1996;11:308-18. [ Links ]
36. Chalker J, Chuc NT, Falkenberg T, Do NT, Tomson G. STD management by private pharmacies in Hanoi: practice and knowledge of drug sellers. Sex Transm Infect 2000;76:299-302. [ Links ]
37. Kroeger A, Ochoa H, Arana B, Diaz A, Rizzo N, Flores W. Inadequate drug advice in the pharmacies of Guatemala and Mexico: the scale of the problem and explanatory factors. Ann Trop Med Parasitol 2001;95:605-16. [ Links ]
38. Lönnroth K. Public health in private hands: studies on private and public tuberculosis care in Ho Chi Minh City, Vietnam (Thesis). Academic. Department, Nordic School of Public Health, Goteborg; 2000. [ Links ]
39. Sjöqvist, F. Drug safety in relation to efficacy: the view of a clinical pharmacologist. Pharmacol Toxicol 2000;86(Suppl 1):30-2. [ Links ]
40. Fass. The Swedish pharmacopeia. Läkemedelsinformation LINFO, Stockholm; 2001. [ Links ]











 texto em
texto em