Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Pharmacy Practice (Granada)
versión On-line ISSN 1886-3655versión impresa ISSN 1885-642X
Pharmacy Pract (Granada) vol.5 no.2 Redondela abr./jun. 2007
| Original Research |
Eliciting comprehensive medication histories in the emergency department: the role of the pharmacist
Meredith CROOK, Maya AJDUKOVIC, Christopher ANGLEY, Natalie SOULSBY, Christopher DOECKE, Ieva STUPANS, Manya ANGLEY.
| ABSTRACT The Australian Pharmaceutical Advisory Committee guidelines call for a detailed medication history to be taken at the first point of admission to hospital. Accurate medication histories are vital in optimising health outcomes and have been shown to reduce mortality rates. Key words: Medication Errors. Pharmaceutical Services. Medical Records. Australia. | RESUMEN Las guías del Comité Consultivo Farmacéutico Australiano piden que se realice un historial de medicación detallado en el punto de ingreso del hospital. Para optimizar los resultados en salud son vitales los historiales de medicación fiables que han demostrado reducir las tasas de mortalidad. Palabras clave: Errores de medicación. Servicios farmacéuticos. Historiales médicos. Australia. |
Meredith CROOK. B.Pharm (Hons). School of Pharmacy and Medical Sciences, University of South Australia. Adelaide (Australia).
Maya AJDUKOVIC. B.Pharm (Hons). School of Pharmacy and Medical Sciences, University of South Australia. Adelaide (Australia).
Christopher ANGLEY. MBBS FACEM, Senior Consultant in Emergency Medicine, Emergency Department, Royal Adelaide Hospital. Adelaide (Australia).
Natalie SOULSBY. M.Pharm, PhD Candidate. Quality Use of Medicines and Pharmacy Research Centre, Sansom Institute, School of Pharmacy and Medical Sciences, University of South Australia. Adelaide (Australia).
Christopher DOECKE. B Pharm, PhD. Director of Pharmacy Services, Royal Adelaide Hospital and School of Pharmacy and Medical Sciences, University of South Australia. Adelaide (Australia).
Ieva STUPANS. B.Pharm(Hons), PhD. Dean Teaching and Learning, Division of Health Sciences, University of South Australia. Adelaide (Australia).
Manya ANGLEY. B.Pharm, PhD. Quality Use of Medicines and Pharmacy Research Centre, Sansom Institute, School of Pharmacy and Medical Sciences, University of South Australia. Adelaide (Australia).
INTRODUCTION
An accurate medication history is a vital part of any hospital admission process. Currently in Australian Emergency Departments (EDs) and in most EDs around the world this task is undertaken by junior doctors.1,2 A number of studies have shown that pharmacists record a more comprehensive medication history than other health professionals.3-7 Medication histories are an effective way of contributing to the decrease of medication errors and identifying medication related hospital admissions.8 In a number of Australian studies conducted between 1988 and 1996, medication related hospital admissions were shown to account for up to 22% of Emergency Department (ED) admissions involving the elderly.9 In response to these alarming trends the Australian Pharmaceutical Advisory Council (APAC) has developed guidelines to achieve a continuum for the quality use of medicines during the period of a patient's entry into, and treatment within hospital and re-entry into the community or residential care.10 Mant et al 2001 have shown via descriptive surveys from general practitioners (GPs) that there is currently poor compliance and inconsistent implementation of the APAC guidelines.11
Principle four of the APAC guiding principles12, based on the APAC guidelines 1998,10 states that an accurate and complete medication history should be obtained and documented at the time of presentation or admission, or as early as possible in the episode of care. An initial medication history is essential to ensure continuity and accuracy of treatment. It has been suggested that if the initial medication history is inaccurate or incomplete, patients are put at risk.13 Medication errors, including omission of regular medications, may occur, which may cause the patient's condition to deteriorate and result in a longer hospital stay. Inaccurate or incomplete histories may also lead to inappropriate prescribing causing unintended drug interactions, and adverse drug events may be unnoticed.5
Pharmacists are especially suited to recording medication histories, as they are more likely recognise the importance of recording these histories and are potentially able to allocate a greater proportion of their time to this task.4 They are more familiar with drug names, effects, dosage forms, strengths and routes of administration than any other health care professional.7 As a result of this familiarity, pharmacists may efficiently be able to identify medications from a description of size and colour, if the medications have not been brought in with the patient.13 They are also ideally placed to identify medication related problems at the point of admission and have a positive impact on patient care.8
An accurate record of non-prescription and complementary or alternative medications is also important, as these products can have significant side effects and drug interactions, particularly in the elderly.7,14 The risk of side effects and drug interactions is increased when patients do not tell their doctors that they are taking non-prescription or complementary or alternative medications. Patients may not think the information is relevant, or are afraid of the doctor's opinion on such medications. Patients may also not consider creams, eye drops, inhalers or patches to be medications. In many cases patients need to be guided to disclose their use these types of medications.5
A pharmacist-conducted medication history service has been shown to be economically viable. A large American study involving 1016 hospitals reported this service to save seven million dollars per hospital per year.15 This service has also been shown to decrease mortality rates.16
In Australia, a study by McCrudden 3 examined the benefits of pharmacist-acquired medication histories and compared the activities in three teaching hospitals in NSW. Over a 4 week period, 580 medication histories were compiled and discrepancies and their clinical significance were assessed. Other Australian studies have focused on the role of a clinical pharmacist in the ED, describing medication history taking as a key clinical activity.17,18
The patient group most likely to experience medication misadventure and therefore most likely to benefit from having a comprehensive medication history documented at the point of admission are the elderly.19 The elderly are also predisposed to adverse drug events as they have physiological differences associated with ageing and often multiple co-morbidities resulting in multiple medications.20 Patients taking multiple medications and those who have multiple co-morbidities have been associated with a higher incidence of adverse drug events and also medication-related problems.19,21 Also patients who have had a recent hospital admission are considered to be at higher risk.22
The aims for this study were to:
1. Compare medication histories recorded by the pharmacy researcher, a pharmacy honours student, with medication histories recorded by ED doctors.
2. Compare adverse drug reactions (ADRs) recorded by the pharmacy researcher with ADRs recorded by ED doctors. The term ADR incorporates ADR-related to the drug's pharmacology, allergies, idiosyncratic reactions and drug intolerances.
3. Record the time taken for the pharmacy researcher to compile and record the medication history.
4. Perform a review of each patient's current list of medications by pharmacy researcher for medication related problems.
5. Record pharmacists' interventions in the ED following pharmacist-acquisition of medication histories.
METHODS
This study was conducted at the Royal Adelaide Hospital (RAH), a teaching hospital with 640 beds. It was carried out in the RAH ED from May 26th 2005 to July 6th 2005. During the study period there were 2560 emergency patients triaged, 639 of whom were aged over seventy years. A convenience sample of 206 patients was considered as appropriate to participate as they were considered to be at high risk of medication misadventure. 106 patients were excluded for reasons including: not wishing to participate; unable to communicate due to language difficulties when an interpreter could not be employed; unable to give consent; (reasons included; severe dementia, deaf, too ill and psychosocial issues); extra precautions required (such as for a patient with multi resistant Staphylococcus aureas infection)
One hundred patients met the following criteria for inclusion in the study:
1. were 70 years or older
2. taking five or more medications
3. had three of more clinical co-morbidities or
4. have had at least one previous hospital admission within the past three months
Medication histories were compiled by the process described below. Patients were selected by evaluating the information provided by the ED patient-tracking screen. This tracking program revealed the triaged patients, their presenting complaints, previous presentations and demographics. Patients were chosen by selecting the lowest triage category (most urgent) and most recent time of presentation. The patient or carer was approached and asked to be involved in the study and asked to sign a consent form. The medication history forms that were used included issues that may influence medication use effectiveness, adult vaccinations, social drug history and medications aids used. There were also sections devoted to current health conditions and medication allergies and ADRs.
After the patient interview the patient's nominated pharmacy and GP practitioner were contacted and notified of the patient's admission. A faxed copy of their medication history was requested. A comprehensive medication history was compiled and attached to the patient's case notes.
When the patient's medication profile was complete each patient's medication profile was reviewed for medication related problems (MRPs). Each MRP was categorised according to a classification system previously used by Beilby et al23 based on the classification system developed by Cipolle et al.24 The pharmacy researcher medication history was then compared to the initial ED doctor medication history recorded in the ED admission form for each patient. When appropriate, the ED doctor was alerted to any discrepancies, MRP or presence of a suspected medication related admission with subsequent medication reconciliation. If a Pharmacist Intervention occurred this was noted and categorised according to a classification system that was also adapted from Beilby et al.23
For the purposes of this study, a medication discrepancy was considered to be any aspect of medication prescribing not recorded by the ED doctor but was recorded in the pharmacy researcher-acquired medication history. It was assumed that the extensive information gathering method used by the pharmacy researcher resulted in an accurate and comprehensive medication history. The discrepancies that were noted between the ED doctor and pharmacy researcher-acquired medication history were classified into one of nine types of discrepancies. For completeness, if the ED doctor had not documented a medication history in the ED admission form and had only referred to a medication "list", "sheet" or a residential care facility medication chart that accompanied the patient on presentation, each of the drugs was classified as an omitted drug.
This study was granted ethics approval from the University of South Australia and The Royal Adelaide Hospital.
RESULTS
There were 58 females and 42 males in the patient group examined and their mean age was 80.1 (SD=5.7) (range, 70 - 96) years. The mean number of medications taken per patient was 11.5 (SD=4) (range, 5 – 23). Of the complete medication histories that were compiled for 100 patients, the mean time taken for the medication history interviews was 13.9 (SD=6.3) minutes (range 4 – 40 minutes).
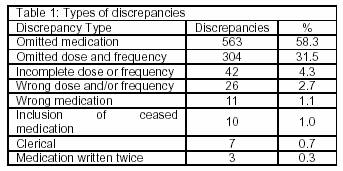
A total of 1152 medications were recorded by the pharmacy researcher and of those 189 (16.4%) medications recorded by the ED doctors were equivalent to those recorded by the pharmacy researcher. In total, there were 966 discrepancies. The majority (90%) of the discrepancies were 'omitted medication' and 'omitted dose and frequency' (See Table 1). The mean number of discrepancies per patient was 9.7 (SD=4.7).
Clerical discrepancies occurred on 7 occasions (i.e. <1%). The term 'clerical discrepancy' was assigned when the patient was receiving the appropriate amount of the drug but the wrong tablet strength was recorded. For example the term clerical discrepancy was used if a patient was taking two 500 mg of metformin tablets twice daily and the ED doctor specified the dose to be 1000 mg bd.
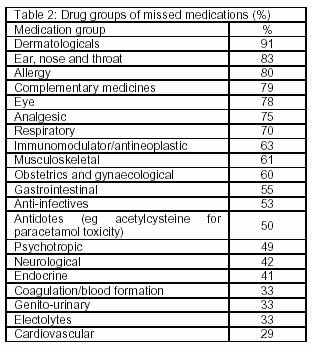
The 563 medications that were omitted by ED doctors were categorised into therapeutic groups according to the Australian Medicines Handbook.25 The most poorly recorded group of medications were those used for dermatological disorders and the most accurately recorded were those used for cardiovascular disorders (see Table 2).
In total there were 79 ADRs recorded by the pharmacy researcher for the 100 patients (some patients had more than one ADR recorded). For 22 (28%) of these ADRs, the ED doctor had recorded the name of the drug and description of the nature of the ADR. For 38 (48%) patients, ADRs were not recorded by the ED doctor. For these ADRs, in 19 (24%) of the cases the name of the medication was recorded by the ED doctor but not a description of the nature of the ADR. In 30 out 100 patients there was no ADR history recorded, in 10 of these patients, were there no known ADRs.
The pharmacy researcher recorded a description of nature of the ADR on 45 occasions. Often the description of the nature of the ADR given by the patient was vague and in fact may have occurred many years prior. Allergies were generally obtained from a patient's personal medication 'list' they carried with them on presentation or from the faxed GP medication history. When questioned on the nature the allergic reaction, patients often could not remember what had happened, or in some cases never heard of the medication. The most commonly allergy reported involved antibiotics. The incidence of reported allergy to penicillin antibiotics was high i.e. 17% in our study population.
Ninety six community pharmacists were contacted and the relevant patient's medication history was requested. Eight pharmacists did not fax back a medication history. Hence, 88 pharmacy medication histories were received in a mean time of 30.2 minutes (range 1 – 334 minutes). Eighty three GPs were contacted and the relevant patient's medication history was requested. Eighteen GPs did not fax back a medication history (Table 2). Hence, 65 GP histories were received in a mean time of 322.2 minutes (range 1 – 7192 minutes (5 days).
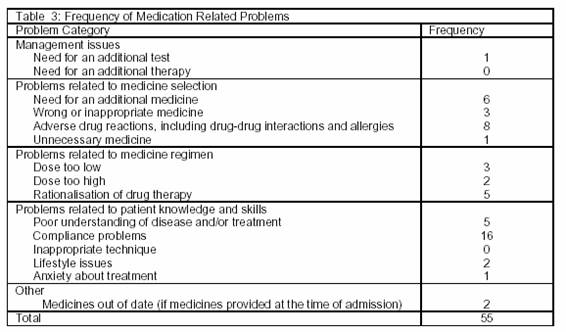
Fifty five MRPs were identified within patients' medication regimens and categorised as 'need for additional drug therapy', 'unnecessary drug therapy', 'wrong drug', dosage too low', adverse drug reaction', 'dose too high' and 'compliance' as described by Cipolle et al.24 The most frequent MRP was 'Compliance problems' (see Table 4).
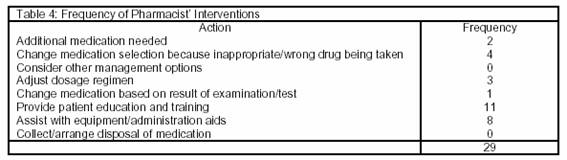
Twenty nine pharmacist interventions were recorded. The most frequent interventions were providing patient education and training and assisting with equipment and administration aids (See Table 4).
DISCUSSION
This study has demonstrated the value of pharmacists compiling the medication histories of patients on admission to the ED of a hospital. The pharmacy researcher was a pharmacy honours student under the supervision of an academic pharmacist with extensive clinical experience. The experience of the research team was considered as being approximately representative of the level of professional functioning typically observed in a hospital pharmacist, and hence the results are generalisable to that population. Being a specific part of their role, pharmacists have more time to spend on the compilation of these histories and are able to contact alternative information sources such as community pharmacists and/or GPs. Indeed, lack of time was identified by the RAH ED doctors as the major barrier to compiling a complete medication history.
Not one initial medication history by the ED doctor was found to be complete. Of particular note, was the reference to 'lists' or 'charts' by ED doctors. Such references are not ideal as the 'list' or photocopy of a medication chart (which is often hard to read) may be lost or damaged, meaning that no complete medication history would be available.5 However, it should be noted that in standard clinical practice at the RAH, initial medication histories are not considered as final by the ED staff. This informal treatment of the document may compromise its accuracy in a number of ways. Anecdotally, it was reported that the admitting doctor for a given specialty would compile another medication history for use on the ward.
To enable the capture of more data in the study reported in this paper, it was considered appropriate to compare the pharmacy researcher history with the ED admission form as the ED admission form is completed for all patients presenting to the ED, not only those admitted.
Furthermore as patients can remain in the ED for up to a day, doctors can make an informed decision regarding the patient's medication regime. When drugs were omitted, which occurred for 48% of the total drugs recorded, there is the potential for drug interactions or ADRs to be undetected. These omissions also have the potential to cause significant harm. For example, if the medications are not administered in hospital, they will not be included in the discharge summary that is sent to GPs. Such omissions have been associated with patients having an increased risk of hospital admission or adverse event.26,27
As discussed above, the largest number of discrepancies was for 'omitted medication' (58.3% of all discrepancies). Previous studies have also shown a high prevalence of this type of discrepancy.3,28,29 In addition 23% of patients' medication histories contained at least one wrong dose and or/frequency and 10% of patients had one wrong drug specified. If a medication history had not been taken by the pharmacy researcher, these errors may not have been noticed and corrected in a timely fashion during the patient's admission. In an Australian study reviewing GP and hospital communications, Wilson et al.30 reported that 17.3% of discharge summaries contained medication errors. If medication errors made on admission are not corrected during admission, they will be perpetuated on the discharge summary rendering the patient at risk of medication misadventure post-discharge.31
The most poorly recorded groups of medications were dermatological, followed by ear, nose and throat medications, allergy, complementary or alternative medications, eye and analgesics. The groups of medications that contained fewer omissions were more likely to be considered important by the medical staff and included cardiovascular, electrolytes, coagulation/blood formation and endocrine medications. The number of omissions in these groups were still of concern, for example 29% of cardiovascular drugs and 41% of endocrine drugs were not recorded by the ED doctors. These results are comparable with a similar study by Lau32 where amongst 304 patients, the highest category of omissions in medication histories were analgesics. Lau also found significant omissions in important groups of medications such as those used to manage cardiovascular and endocrine disorders.
Compiling an accurate history from multiple sources proved time consuming. Pharmacists were frequently more readily available to validate our medication histories. GPs were often out of the surgery, and receptionists often screened their calls. Leaving messages was often unsuccessful. Not only did more GPs not fax the medication history, when they did it took considerably longer than pharmacists. Also some receptionists, GPs and pharmacists were reluctant to fax medication histories due to patient confidentiality issues. This delay was overcome by faxing the patient's consent form. In practice a consent form could be used to overcome these barriers, and hospital protocols should cover emergencies or situations where consent cannot be obtained.12
This study reinforced that currently there is poor documentation of patients ADR history. Information that would be deemed helpful when recording ADRs includes: date of reaction, specific drug, type of reaction and who documented the reaction were often not available. As a result of this lack of detail, the incidence of true allergies is often overstated.33
The MRP rate was found to be 0.55 per patient. This is considerably lower than other studies of similar high risk populations19 and may be lower because identifying MRPs was not the primary focus of the study. The most frequent intervention was patient education and training, this occurred mainly in response to 24% of patients experiencing problems relating to patient knowledge and skills, which directly or indirectly caused compliance problems. It has been estimated the portion of non-compliant elderly patient varies from 26 – 59%.34 In order to improve compliance, patient education and follow up is essential. One way to ensuring follow up is to develop a Medication Action plan as referred to in the APAC guiding principles 2005 and send it in a timely manner to the patient's GP.12
A further study is currently underway examining the uptake of pharmacists' recommendations during admission following identification of discrepancies in the medication histories and will be measured by comparing medication discharge summaries with the initial doctor acquired ED medication histories.
CONCLUSION
A pharmacist's training in pharmacology and familiarity with the appearance and dosage forms of medications, places them in an ideal position to elicit a more accurate medication history. 13 Pharmacists should play a proactive role in compiling medication histories and conducting a clinical pharmacy review at the first point of presentation to hospital. This would lead to a reduction in the number of medication errors as well as enable early identification of MRPs therefore minimising subsequent adverse drug events. Ultimately a pharmacist-acquired medication history and review can potentially minimise medication misadventure and have a positive impact on patient outcomes.
ACKNOWLEDGEMENT
The assistance provided by Dr Barbara Anderson with the preparation of this article is acknowledged with gratitude.
| References |
1. McFadzean E, Isles C, Moffat J, Norrie J, Steward D. Is there a role for a prescribing pharmacist in preventing prescribing errors in a medical admission unit? The Pharmaceutical Journal. 2003;270:896-9. [ Links ]
2. Taylor D McD, Bennett DM, Cameron PA. A paradigm shift in the nature of care provision in emergency departments. Emerg Med J. 2004;21:681-4. [ Links ]
3. McCrudden EA, Paloumis S, Tao MM, Burke RA, Pulver L, Meyer E, et al. Review of Pharmacist-Conducted Medication Histories at Three Teaching Hospitals. Australian Journal of Hospital Pharmacy. 1995;25:261-3. [ Links ]
4. Cavin A, Sen B. Improving medication history recording and the identification of drug related problems in and A&E department. Hospital Pharmacist. 2005;12:109-12. [ Links ]
5. Collins DJ, Nickless GD, Green CF. Medication histories: does anyone know what a patient should be taking? International Journal of Pharmacy Practice. 2004;12:173-8. [ Links ]
6. Gurwich E. Comparison of medication histories acquired by pharmacists and physicians. Am J Hosp Pharm. 1983;40:1541-2. [ Links ]
7. Nester TM, Hale LS. Effectiveness of a pharmacist-acquired medication history in promoting patient safety. Am J Health Sys Pharm. 2002;59:2221-5. [ Links ]
8. Slee A, Farrar K, Hughes D, Constable. Optimising medical treatment - how pharmacist-acquired medication histories have a positive impact on patient care. Pharmaceutical Journal. 2006;277:737-9. [ Links ]
9. Roughead EE, Gilbert AL, Primrose JG, Sansom L N. Drug-related hospital admissions: a review of Australian studies published 1988-1996. Med J Aust. 1998;168:405-8. [ Links ]
10. Australian Pharmaceutical Advisory Council. National guidelines to achieve the continuum of quality use of medicines between hospital and community. Canberra: Commonwealth Department of Health and Family Services; 1998. [ Links ]
11. Mant A, Rotem WC, Kehoe L, Kaye KI. Compliance with guidelines for continuity of care in therapeutics from hospital to community. Med J Aust. 2001;174:277-80. [ Links ]
12. Australian Pharmaceutical Advisory Council. Guiding Principles to achieve continuity in medication management. Canberra: Commonwealth of Australia; 2005. [ Links ]
13. Dutton K, Hedger N, Wills S, Brown D, Davies P. Prevent medication errors on admission. Clinical Governance: An International Journal. 2003;8(2):128-37. [ Links ]
14. Peterson G. The hidden dangers of complementary medicine in the elderly. Australian Pharmacist. 2004;23(9):662-4. [ Links ]
15. Bond CA, Raehl CL, Franke T. Clinical Pharmacy Services, Pharmacy Staffing, and the Total Cost of Care in United States Hospitals. Pharmacotherapy. 2000;20(6):609-21. [ Links ]
16. Bond CA, Raehl CL, Franke T. Clinical Pharmacy Services and Hospital Mortality Rates. Pharmacotherapy. 1999;19(5):556-64. [ Links ]
17. Harding A. The role of an Emergency Department Pharmacist. Austr J Hosp Pharm 2001;27:325-7. [ Links ]
18. Welch S. The Evolving Area of Emergency Medicine Pharmacy. Austr J Hosp Pharm 1997;27:325-7. [ Links ]
19. Gilbert AL, Roughead EE, Beilby J, Mott K, Barratt JD. Collaborative medication management services: improving patient care. Med J Aust. 2002;177:189-92. [ Links ]
20. Chan M, Nicklason F, Vial J. Adverse drug events as a cause of hospital admission in the elderly. Intern Med J. 2001;31:199-205. [ Links ]
21. Rothschild J, Bates D, Leape L. Preventable medical injuries in older patients. Arch Intern Med. 2000;160:2717-28. [ Links ]
22. March G, Gilbert A, Roughead E, Quintrell N. Developing and evaluating a model for pharmaceutical care in Australian community pharmacies. Int J Pharm Pract 1999;7:220-9. [ Links ]
23. Wilkinson D, McElroy H, Beilby J, Mott K, Price K, Morey S, et al. Uptake of health assessments, care plans and case conferences by general practitioners through the Enhanced Primary Care program between November 1999 and October 2001. Aust Health Rev. 2002;25(4):1-11. [ Links ]
24. Cipolle RJ, Strand LM, Morley PC. Pharmaceutical Care Practice. New York: McGraw-Hill; 1998. [ Links ]
25. Rossi S, editor. Australian Medicines Handbook. Adelaide: Australian Medicines Handbook; 2005. [ Links ]
26. Stowasser DA, Collins DM, Stowasser M. A Randomised Controlled Trial of Medication Liaison Services - Patient Outcomes. J Pharm Prac Res 2002;32(2):133-40. [ Links ]
27. Stowasser DA, Collins DM, Stowasser M. A randomized controlled trial of medication liaison services - acceptance and use by health professionals. J Pharm Prac Res 2002;32:221-6. [ Links ]
28. Lazarou J, Pomeranz BH, Corey PN. Incidence of adverse drug reactions in hospitalized patients: a meta analysis of prospective studies. JAMA 1998;279(1):1200-5. [ Links ]
29. Drewett M. Stop regular medication errors. Pharmacy in Practice. 1998;8(5):193-6. [ Links ]
30. Wilson S, Ruscoe W, Chapman M, Miller R. General practitioner-hospital communications: A review of discharge summaries. J Qual Clin Pract 2001;21(4):104-8. [ Links ]
31. Yu DSF, Thompson DR, Lee DTF. Disease management programmes for older people with heart failure: crucial characteristics which improve post-discharge outcomes. Eur Heart J 2006;27:596-612. [ Links ]
32. Lau HS, Florax C, Porsius AJ, de Boer A. The completeness of medication histories in hospital medical records of patients admitted to general internal medicine wards. Br J Clin Pharmacol 2000 Jun;49(6):597-603. [ Links ]
33. Wyer S. Documentation of Penicillin Allergy in a Veterans' Hospital. Austr J Hosp Pharm 1997;27(4):296-301. [ Links ]
34. Malhoutra S, Karan RS, Pandhi P, Jain S. Drug related medical emergencies in the elderly: role of adverse drug reactions and non-compliance. Postgrad Med J 2001;77:703-7. [ Links ]