Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Pharmacy Practice (Granada)
versión On-line ISSN 1886-3655versión impresa ISSN 1885-642X
Pharmacy Pract (Granada) vol.5 no.3 Redondela jul./sep. 2007
| Original Research |
Evaluation of thiazide diuretic use as preferred therapy in uncomplicated essential hypertension patients
Ronald S. GREENE, Marissa ESCOBAR QUINONES, Krystal L. EDWARDS.
| ABSTRACT Thiazide diuretics are effective antihypertensive medications shown to reduce the risk of cardiovascular events and stroke. Despite being the preferred choice for uncomplicated essential hypertension, thiazide diuretics continue to be underutilized. Key words: Hypertension. Economics, Pharmaceutical. Sodium Chloride Symporter Inhibitors. United States. | RESUMEN Los diuréticos tiazídicos son medicamentos antihipertensivos que demostraron reducir el riesgo de eventos cardiovasculares e infartos. A pesar de ser la elección preferida para hipertensión arterial no complicada, los diuréticos tiazídicos continúan infrautilizados. Palabras clave: Hipertensión. Economía, Farmacéutica. Inhibidores del transporte de cloruro sódico. Estados Unidos. |
Ronald S. GREENE, PharmD, BCPS, CDE. Assistant Professor of Pharmacy Practice/Advanced Practice Pharmacist in Primary Care. School of Pharmacy, Texas Tech University Health Sciences Center; and Veterans Affairs North Texas Health Care System. Dallas, TX (USA).
Marissa ESCOBAR QUINONES. PharmD. Assistant Professor of Pharmacy Practice. School of Pharmacy, Texas Tech University Health Sciences Center. Dallas, TX (USA).
Krystal L. EDWARDS, PharmD, BCPS. Assistant Professor of Pharmacy Practice/Advanced Practice Pharmacist in Primary Care. School of Pharmacy, Texas Tech University Health Sciences Center; and Veterans Affairs North Texas Health Care System. Dallas, TX (USA).
INTRODUCTION
In 2007, the American Heart Association estimated that 1 in 3 adults in the United States have hypertension with 37.4% of Americans greater than 20 years old having "prehypertension".1 Additionally, the annual direct and indirect cost of managing hypertension was approximately US$66.4 billion.1 Studies have reported that appropriate treatment of hypertension has reduced the average incidence of stroke by 35-40%, myocardial infarction (MI) by 20-25% and heart failure by more than 50%.2 Despite these compelling statistics, of the 65.1% of patients treated for hypertension, only 36.8% are controlled according to data from the National Health and Nutrition Examination Survey (NHANES) between 2003-2004.3
Several large studies have been published supporting the use of thiazide diuretics for the treatment of hypertension to reduce cardiovascular clinical events and stroke.4-7 Thiazide diuretics are also generally well tolerated and inexpensive.4-9 These reasons have led the Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure (JNC VII) and the Department of Veterans Affairs and Department of Defense (VA/DOD) to recommend the use of thiazide diuretics as the preferred choice for the treatment of uncomplicated hypertension.10,11 However, thiazide diuretics are still underutilized as preferred agents.9,12,13
Therefore, the primary purpose of this study was to determine how often thiazide diuretics were being underutilized as preferred therapy in patients diagnosed with uncomplicated essential hypertension requiring only single antihypertensive therapy at the Veterans Affairs North Texas Health Care System (VANTHCS). We additionally evaluated clinician prescribing habits of antihypertensive therapy and estimated the medication acquisition cost savings that would result if thiazide diuretics were prescribed at our institution as recommended by the VA/DOD guidelines.
METHODS
Patient charts at the VANTHCS were evaluated retrospectively from October 2003 to September 2005. Patients included in this study were those greater than 18 years of age, had a diagnosis of uncomplicated essential hypertension (ICD-9 codes of 401.1 or 401.9) and were prescribed only one antihypertensive medication upon entry into the VANTHCS (pre-existing treated hypertension) or upon new hypertension diagnosis at our facility. Patients were excluded if they had a contraindication to thiazide diuretic therapy or had a compelling comorbidity where another class of antihypertensive was warranted. These included a history of gout, renal disease or insufficiency defined as having a creatinine clearance of less than 30 mL/min or a serum creatinine greater than or equal to 2.5 mg/dL, diabetes mellitus or a hemoglobin A1c greater than 6.5%, congestive heart failure, myocardial infarction, angina, coronary artery disease, heart arrhythmias, stroke, hypertriglyceridemia greater than or equal to 200 mg/dL, benign prostatic hypertrophy, a potassium less than 3.3 mmol/L or a sodium less than 133 mmol/L.
Outpatient pharmacy prescription records were used to identify patients prescribed a single antihypertensive medication during the defined study period. Patient charts were then reviewed using the electronic medical records system to determine those who met the inclusion criteria by evaluating active problem and past medical history lists in the patient's progress notes.
Patient data were divided into two groups to analyze clinician prescribing habits. The conversion group consisted of individuals with pre-existing hypertension that were prescribed an antihypertensive medication at the time of entry into the VANTHCS. The decisions made by the clinicians to continue the patient's current treatment or convert to another medication were evaluated. The new therapy group either had pre-existing hypertension and was not taking an antihypertensive medication upon entry into the VANTHCS or was diagnosed with hypertension after enrolling into the system. For this group, we evaluated the clinician's initial antihypertensive medication choices.
The monthly acquisition cost for each antihypertensive medication was retrieved from the outpatient pharmacy drug database. These costs were then compared to the preferred thiazide diuretic at the VANTHCS, hydrochlorothiazide. This medication, administered as 25 mg orally every day, was used for the cost savings analysis in the study. It was assumed that the efficacy of the initially prescribed medication was equal to the conversion dose of hydrochlorothiazide. The reported savings are in 2005 US dollars.
The investigational review boards of the VANTHCS and the Texas Tech University Health Sciences Center approved the protocol before data collection began. Patient informed consent and approval of the Health Insurance Portability and Accountability Act were not required. Descriptive statistical analyses were used to summarize the data.
RESULTS
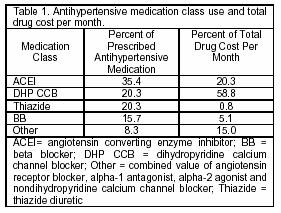
A total of 478 patients met the inclusion criteria and were reviewed for this study. The average age was 57.2 (SD=12.2) years old and 84.3% of the population was male. ACE inhibitors (ACEI) were the most commonly prescribed antihypertensive medication class at 35.4% (n=169) followed by the dihydropyridine calcium channel blockers (DHP CCB) and the thiazide diuretics (thiazide) each at 20.3% (n=97). Beta blockers (BB) represented 15.7% (n=75) of the total prescriptions with the remaining 8.3% of patients (n=40) prescribed other therapy. Other therapy consisted of nondihydropyridine calcium channel blockers, alpha-1 antagonists, angiotensin receptor blockers and alpha-2 agonists in order of decreasing frequency (Table 1).
Clinician prescribing
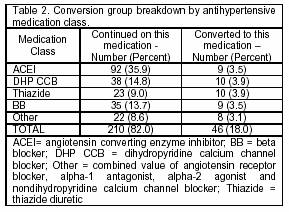
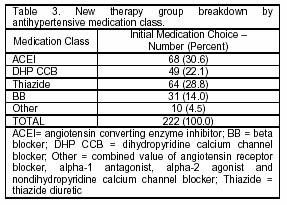
Of the 478 patients, 256 (53.6%) were classified into the conversion group (Table 2). This study found 12.9% of these patients presenting to the VANTHCS requiring single antihypertensive therapy were prescribed a thiazide diuretic as the initial antihypertensive medication. However, only 3.9% (n=10) were actually converted to a thiazide diuretic with the remaining 9.0% (n=23) continued on the thiazide diuretic therapy originally prescribed outside the VANTHCS. In fact, 82.0% of patients within the conversion group were continued on their therapy from outside clinicians without any medication class change. The new therapy group was comprised of the remaining 222 patients (46.4%). Thiazide diuretics were chosen as the initial medication in only 28.8% (n=64) of these patients (Table 3).
Medication acquisition cost
The total cost for one month of antihypertensive drug therapy of all 478 study patients was US$1,873. Fifty-nine percent of this total was from the dihydropyridine calcium channel blockers. Added to the ACE inhibitors and beta blockers, these three classes accounted for 71.4% of the total number of prescriptions written and 84.2% of the total antihypertensive drug cost. The thiazide diuretics, in contrast, were responsible for 0.8% of the total cost. If all patients not initially prescribed a thiazide diuretic were converted to hydrochlorothiazide 25 mg orally every day, it would have resulted in a cumulative medication acquisition cost savings of US$1,795. This results in a total cost of about US$0.17 per patient per month of therapy.
DISCUSSION
The VA/DOD and JNC VII guidelines recommend the use of thiazide diuretics as the preferred agent for the treatment of uncomplicated essential hypertension without compelling indications.10,11 Those compelling indications outlined in the VA/DOD guidelines include diabetes mellitus, systolic heart failure, chronic kidney disease, post stroke and post myocardial infarction.11 We designed our criteria to exclude those meeting the above compelling indications and extended the criteria to exclude patients with heart arrhythmias, gout, hypertriglyceridemia and abnormal laboratory values (low potassium and sodium).
Results of this study indicate that only 20.3% of the identified uncomplicated essential hypertensive patients either received a thiazide diuretic as the initial antihypertensive medication chosen or were changed to such upon entry into the VANTHCS. Morgan and colleagues conducted a similar study in which they evaluated utilization trends of thiazide diuretics as preferred therapy in seniors with hypertension in Canada.9 Their eight year retrospective study found that on average only 38% of uncomplicated hypertensive patients received a thiazide diuretic as the preferred therapy. Together, these studies suggest an underutilization of thiazide diuretics.
Clinician prescribing
Several reasons could explain why clinicians chose other therapies instead of thiazide diuretics. Generally, patients at the VA are older with multiple complicated medical problems, including diabetes, heart failure, coronary artery disease, chronic angina and kidney disease. Clinicians may not be accustomed to treating uncomplicated essential hypertension and thus are not as likely to prescribe thiazide diuretics as the preferred therapy. Also, as patients with hypertension enroll into the VANTHCS, many times therapy prescribed by an outside clinician is successfully controlling the blood pressure. Since several of the antihypertensive medications are on formulary, clinicians are often hesitant to convert to a new medication like a thiazide diuretic and elect to continue the successful regimen.
Clinician knowledge and interpretation of the literature may also provide reasons for not preferentially choosing thiazide diuretics. The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT) found no difference in the primary outcome of combined fatal coronary heart disease or nonfatal MI among individuals treated with chlorthalidone (thiazide), amlodipine (DHP CCB) and lisinopril (ACEI).5 However, the researchers concluded that thiazide diuretics were superior to the other two agents based on secondary endpoints and cost. This trial had a significant influence on the JNC VII guidelines and subsequently on the VA/DOD guidelines. Therefore, the clinician may question the strength of the VA/DOD recommendations depending in part on their interpretation of the ALLHAT results. This question was posed by Petitti and colleagues who retrospectively evaluated prescribing patterns for antihypertensive agents in seven different classes within four different regions of their healthcare system.14 Two of the regions reviewed participated in the ALLHAT study and two did not. The authors hypothesized that participation in the study would be associated with a quicker and greater implementation of the study recommendations utilizing thiazide diuretics as the preferred antihypertensive therapy. They found an increase, although not statistically significant, in the percentage of thiazide diuretic prescriptions in all four regions. There was also a non-significant increase in new thiazide prescriptions among all regions. This study suggests that increased awareness of ALLHAT and JNC VII guidelines does not influence prescribing habits as hypothesized.
Another trial supporting thiazide diuretic use is the Systolic Hypertension in the Elderly Program (SHEP) trial.4 This trial evaluated the use of thiazide diuretics in elderly patients with isolated systolic hypertension (ISH) and found a 36% reduction in the incidence of total stroke. Similar to thiazide diuretics, DHP CCB also have data supporting their use in ISH. The Systolic Hypertension in Europe (Syst-Eur) trial concluded that the use of nitrendipine resulted in a 33% reduction in nonfatal cardiac endpoints and a 31% reduction in nonfatal cardiovascular endpoints in elderly patients with ISH.15 Blood pressure levels were not evaluated in this trial, so it is unknown if patients had isolated systolic hypertension (ISH). Therefore, if patients had ISH, a calcium channel blocker would have been a reasonable preferred agent in the primarily elderly population at the VANTHCS and may explain the 20.3% DHP CCB use.
Clinicians may have also prescribed non-thiazide diuretic therapy based on risk factors for the development of other compelling indications. This use would not have been captured in this retrospective study. For example, the Heart Outcomes Prevention Evaluation (HOPE) trial found that when comparing ramipril to placebo, the use of ramipril significantly reduced the rate of death, myocardial infarction and stroke in high-risk patients who were not known to have a low ejection fraction or heart failure.16 Additionally, angiotensin receptor blockers have also shown benefits in stroke protection as noted by the Losartan Intervention For Endpoint reduction in hypertension study (LIFE).17
The JNC VI guidelines considered BB to be a preferred agent for treatment of uncomplicated hypertension.18 This trial reviewed patient charts starting in October 2003, shortly after the release of the JNC VII guidelines in May 2003, which removed BB as a preferred therapy. The current VA/DOD guidelines were not updated until August 2004 and this may explain the 15.7% use of BB in this study.
Medication acquisition cost
Only medication acquisition costs to the facility were included in the cost analysis. If all patients had been prescribed hydrochlorothiazide 25mg administered orally every day, the facility would have saved 95.8% per month in medication acquisition costs. Fischer and Avorn conducted a cost analysis which evaluated potential saving with appropriate thiazide diuretic use.8 They found thiazide utilization to be 4.3% (total antihypertensive prescriptions, both complicated and uncomplicated patients). They also determined that US$4.32 million and US$2.05 million could be saved yearly if 27.6% (n=140,600) of the prescribed calcium channel blockers and 23.0% (n=94,060) of the prescribed ACE inhibitors were converted to a thiazide diuretic. Collectively, data from this study and from Fischer and Avorn proposes a significant medication acquisition cost savings potential when thiazide diuretics are used appropriately.
CONCLUSION
This study found that thiazide diuretics were underutilized as preferred therapy in patients with pre-existing or newly diagnosed uncomplicated essential hypertension at the VANTHCS. There are several reasons clinicians may have chosen a non-thiazide diuretic regimen; however, thiazide diuretics remain an important antihypertensive class and are considered the preferred agent for uncomplicated essential hypertension in the VA/DOD guidelines.11 Finally, while cost of therapy should not be the sole reason for medication selection, thiazide diuretics are an attractive option and should be considered as a preferred therapy in this patient population.
ACKNOWLEDGEMENT
The authors of this study would like to acknowledge Holly Hoffman-Roberts, Pharm.D. and Brian K. Irons, Pharm.D., BPCS for their critical review of this manuscript. The funding for this study was provided by salary support via Texas Tech University Health Sciences Center
CONFLICT OF INTEREST
None declared.
| References |
1. Rosamond W, Flegal K, Friday G, Furie K, Go A, Greenlund K, Haase N, Ho M, Howard V, Kissela B, Kittner S, Lloyd-Jones D, McDermott M, Meigs J, Moy C, Nichol G, O'Donnell CJ, Roger V, Rumsfeld J, Sorlie P, Steinberger J, Thom T, Wasserthiel-Smoller S, Hong Y; American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics--2007 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation 2007;115(5):e69-171. [ Links ]
2. Neal B, MacMahon S, Chapman N. Effects of ACE inhibitors, calcium antagonists, and other blood-pressure-lowering drugs: results of prospectively designed overviews of randomised trials. Blood Pressure Lowering Treatment Trialists' Collaboration. Lancet 2000;356(9246):1955-64. [ Links ]
3. Ong KL, Cheung BM, Man YB, Lau CP, Lam KS. Prevalence, awareness, treatment, and control of hypertension among United States adults 1999-2004. Hypertension 2007;49(1):69-75. [ Links ]
4. Prevention of stroke by antihypertensive drug treatment in older persons with isolated systolic hypertension. Final results of the Systolic Hypertension in the Elderly Program (SHEP). SHEP Cooperative Research Group. JAMA 1991;265(24):3255-64. [ Links ]
5. Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). JAMA 2002;288(23):2981-97. [ Links ]
6. Psaty BM, Lumley T, Furberg CD, Schellenbaum G, Pahor M, Alderman MH, Weiss NS. Health outcomes associated with various antihypertensive therapies used as first-line agents: a network meta-analysis. JAMA 2003;289(19):2534-44. [ Links ]
7. Psaty BM, Smith NL, Siscovick DS, Koepsell TD, Weiss NS, Heckbert SR, Lemaitre RN, Wagner EH, Furberg CD. Health outcomes associated with antihypertensive therapies used as first-line agents. A systematic review and meta-analysis. JAMA 1997;277(9):739-45. [ Links ]
8. Fischer MA, Avorn J. Economic implications of evidence-based prescribing for hypertension: can better care cost less? JAMA 2004;291(15):1850-6. [ Links ]
9. Morgan S, Bassett KL, Wright JM, Yan L. First-line first? Trends in thiazide prescribing for hypertensive seniors. PLoS Med 2005;2(4):e80. [ Links ]
10. Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, Jones DW, Materson BJ, Oparil S, Wright JT Jr, Roccella EJ; Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. National Heart, Lung, and Blood Institute; National High Blood Pressure Education Program Coordinating Committee. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension 2003;42(6):1206-52. [ Links ]
11. Group VDE-BCPGW. Diagnosis and Management of Hypertension in the Primary Care Setting. In: Veterans Health Administration DoVA, and Health Affairs, Department of Defense, ed. Washington, DC: Office of Quality and Performance November 1999 (Updated August 2004). [ Links ]
12. Fretheim A, Aaserud M, Oxman AD. The potential savings of using thiazides as the first choice antihypertensive drug: cost-minimisation analysis. BMC Health Serv Res 2003;3(1):18. [ Links ]
13. Psaty BM, Manolio TA, Smith NL, Heckbert SR, Gottdiener JS, Burke GL, Weissfeld J, Enright P, Lumley T, Powe N, Furberg CD; Cardiovascular Health Study. Time trends in high blood pressure control and the use of antihypertensive medications in older adults: the Cardiovascular Health Study. Arch Intern Med 2002;162(20):2325-32. [ Links ]
14. Petitti DB, Xie F, Barzilay JI. Prescribing patterns for thiazide diuretics in a large health maintenance organization: relationship to participation as an ALLHAT clinical center. Contemp Clin Trials 2006;27(5):397-403. [ Links ]
15. Staessen JA, Fagard R, Thijs L, Celis H, Arabidze GG, Birkenhager WH, Bulpitt CJ, de Leeuw PW, Dollery CT, Fletcher AE, Forette F, Leonetti G, Nachev C, O'Brien ET, Rosenfeld J, Rodicio JL, Tuomilehto J, Zanchetti A. Randomised double-blind comparison of placebo and active treatment for older patients with isolated systolic hypertension. The Systolic Hypertension in Europe (Syst-Eur) Trial Investigators. Lancet 1997;350(9080):757-64. [ Links ]
16. Effects of ramipril on cardiovascular and microvascular outcomes in people with diabetes mellitus: results of the HOPE study and MICRO-HOPE substudy. Heart Outcomes Prevention Evaluation Study Investigators. Lancet 2000;355(9200):253-9. [ Links ]
17. Dahlof B, Devereux RB, Kjeldsen SE, Julius S, Beevers G, de Faire U, Fyhrquist F, Ibsen H, Kristiansson K, Lederballe-Pedersen O, Lindholm LH, Nieminen MS, Omvik P, Oparil S, Wedel H; LIFE Study Group. Cardiovascular morbidity and mortality in the Losartan Intervention For Endpoint reduction in hypertension study (LIFE): a randomised trial against atenolol. Lancet 2002;359(9311):995-1003. [ Links ]
18. The sixth report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure. Arch Intern Med 1997;157(21):2413-46. [ Links ]