INTRODUCTION
Type 2 diabetes mellitus (T2DM) is a prevalent condition with a high economic burden. According to the most recent Centers for Disease Control and Prevention National Diabetes Statistics Report, there are over 29 million people in the United States with diabetes mellitus, leading to an estimated economic burden of USD240 billion annually.1 There are many oral and injectable options for the management of T2DM, making clinical decisions regarding selection of therapy increasingly complex. Each medication has specific patient considerations, including average hemoglobin A1c (HbA1c) reduction, adverse effect profile, administration method, potential for drug-drug interactions, and cost.2,3,4
The American Association of Clinical Endocrinologists (AACE) and American Diabetes Association (ADA) guidelines both aid in selection of therapy for patients with T2DM.2,3 The alpha-glucosidase inhibitors are not listed in the ADA guidelines as a recommended oral option for patients with T2DM, and are noted to be generally unfavored. However, the AACE guidelines rank the alpha-glucosidase inhibitors as an option for monotherapy or add-on therapy, with a lower preference as compared to other antihyperglycemic medications.2 However, acarbose may be used more commonly internationally as evidenced by the International Diabetes Federation Global Guidelines recommendation of acarbose as an alternative first-line option to metformin, or as a second-line add on therapy.4
The mechanism of alpha-glucosidase inhibition occurs within the gastrointestinal (GI) tract.5 Alpha-glucosidase is the enzyme responsible for the breakdown of complex oligosaccharides and polysaccharides to monosaccharides, allowing for absorption. Inhibition of alpha-glucosidase limits breakdown to absorbable monosaccharides, thus decreasing postprandial blood glucose. Acarbose, an alpha-glucosidase inhibitor, results in an average HbA1c lowering of 0.5-0.8%.6,7 A limitation to its use is intolerability due to GI adverse effects, including flatulence, abdominal cramps, diarrhea, and nausea.
Acarbose is included on the Veterans Affairs National Formulary and may be added in T2DM patients that have not reached their HbA1c goal with an existing regimen. In this Veterans Affairs Medical Center, acarbose may be added to an existing oral regimen in patients with uncontrolled T2DM who are hesitant to initiate insulin therapy. Due to significant GI adverse effects, dose titrations are often limited or the medication may need to be discontinued. Thus, the efficacy of acarbose in our patient population is unknown. This study sought to determine the average HbA1c reduction with addition of acarbose to insulin and non-insulin regimens, as well as to assess for tolerability of the medication. We also determined how many patients were initiated on insulin despite addition of acarbose to an existing oral regimen for T2DM.
METHODS
Study objectives
The primary objective of the study was to assess average change in HbA1c with addition of acarbose to insulin and non-insulin regimens in patients with T2DM. Secondary objectives were to evaluate the discontinuation rate of acarbose, and to assess the number of patients who were placed on insulin despite addition of acarbose.
Study design
This study was approved by the Baylor College of Medicine Institutional Review Board under expedited review. A retrospective chart review was conducted on veterans with T2DM initiated on acarbose between October 1, 2013 and December 31, 2013. To be included, patients must have had prescription refill data indicating at least 3 months of acarbose use. In order to assess for average HbA1c reduction, patients must have had at least one HbA1c reading within 6 months prior to initiation of acarbose, and one reading after at least 3 months of treatment. Hemoglobin A1c results prior to the intervention were restricted to the previous 6 months in order to limit impact from other variables. Excluded patients were those with contraindications to acarbose use, including type 1 diabetes mellitus, serum creatinine of 2 mg/dL or greater at time of acarbose initiation, or a diagnosis based on ICD-9 codes for an existing GI condition (irritable bowel disease, colonic ulceration, or partial intestinal obstruction) or liver cirrhosis. To assess the primary objective of mean change in HbA1c, the most recent HbA1c within 6 months prior to addition of acarbose and the most recent HbA1c after at least 3 months of treatment were compared. Secondary outcomes were assessed through chart review of outpatient prescription history.
Statistical analysis
The two-tailed, paired t-test was used to assess change in HbA1c with the addition of acarbose. Subgroup analyses of the primary outcome were performed for those with and without active prescriptions for insulin at time of acarbose initiation. Descriptive statistics were used for all other outcomes. Microsoft Excel was used for all analyses.
RESULTS
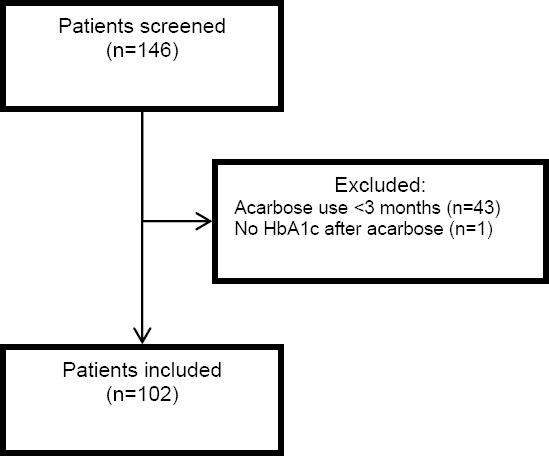
Of the 146 patients screened, 102 patients were included in the study (Figure 1). Exclusions were primarily a result of patients not continuing acarbose for at least 3 months (n=43), as well as not having a HbA1c result after acarbose initiation (n=1). The majority of patients in the study were male (93.2%) and Caucasian (51%), with an average age of 63 years (Table 1).
Table 1 Baseline Characteristics
| Characteristic | Value |
|---|---|
| Male | 95 (93.2%) |
|
| |
| Mean age (years) | 63.2 (SD=9.4) |
|
| |
| Race | |
| Caucasian | 52 (51%) |
| Black or African-American | 25 (24.5%) |
| Hispanic or Latino | 12 (11.5%) |
| Asian | 4 (4%) |
| Native Hawaiian or Pacific Islander | 4 (4%) |
| American Indian or Alaskan Native | 1 (1%) |
| Not reported | 4 (4%) |
|
| |
| Baseline T2DM medications | |
| Oral agents alone | 29 (28.5%) |
| Receiving insulin | 73 (71.5%) |
The results for the primary objective are summarized in Figure 2. In the total study population, the average HbA1c before and after acarbose initiation was 9.08% (SD=1.74) and 8.43% (SD=1.74) respectively, with an average HbA1c reduction of 0.65% (n=102, p=0.0005). A subgroup analysis was performed to evaluate differences between those with or without concurrent insulin use at the time of acarbose initiation. In those on insulin therapy, the average HbA1c before and after acarbose initiation was 9.38% (SD=1.7) and 8.28% (SD=1.46) respectively, with an average HbA1c reduction of 1.1% (n=29, p=0.002). In patients on non-insulin therapies at the time of acarbose initiation, the average HbA1c before and after acarbose initiation was 8.97% (SD=1.75) and 8.48% (SD=1.82) respectively, with an average HbA1c reduction of 0.49% (n=73, p=0.012).
Acarbose tolerability was evaluated by assessing the discontinuation rate and reasons for discontinuation. Of the 102 patients included in the study, 40 patients (39.2%) discontinued acarbose after at least 3 months of use. The primary reasons for discontinuation of therapy were GI intolerance (n=11, 27.5%) or an expired prescription order that was never renewed (n=7, 17.5%). Five patients (12.5%) had prescriptions for acarbose discontinued per the facility’s “Polypharmacy Policy”, which implies that the prescription had not been refilled for at least 7 months. Regarding the secondary outcome of insulin initiation in insulin naïve patients, 73 of the 102 patients in the study were not on insulin at the time of acarbose initiation. Of those patients, 19 (26%) were started on insulin therapy despite addition of acarbose (Table 2).
Table 2 Acarbose discontinuation (N=40)
| Reason for discontinuation | Patients (%,) |
|---|---|
| Gastrointestinal intolerance | 11 (27.5%) |
| Prescription expired and never renewed | 7 (17.5%) |
| Discontinued per “Polypharmacy Policy”* | 5 (12.5%) |
| Non-compliance of unknown reason | 3 (7.5%) |
| Starting insulin | 3 (7.5%) |
| Discontinued by outside provider | 2 (5%) |
| Undocumented | 9 (22.5%) |
*Polypharmacy Policy: Medications have not been refilled in the previous 7 months are discontinued from the patient profile
DISCUSSION
The patient population in this study is similar to that of other Veterans Affairs Medical Center study populations, consisting of primarily middle-aged Caucasian males. However, many other racial groups were represented in the study population. No exclusions were due to contraindications to use of acarbose, thus prescribing practices for acarbose appear appropriate in terms of safety.
In regards to the primary outcome, a statistically significant decrease in mean HbA1c was seen with the addition of acarbose to both insulin and non-insulin regimens. The average HbA1c reduction for the total study population was 0.65%, which is comparable to the 0.5-0.8% seen in previous studies. In the subgroup analyses, reductions in HbA1c remained statistically significant. In the subgroup of patients on insulin at time of acarbose initiation, higher initial HbA1c results were seen as well as a greater mean reduction in HbA1c, which is likely due to concurrent insulin dose titrations.
When evaluating secondary objectives, it was found that acarbose was discontinued after at least 3 months of use in nearly 40% of the patients included in the study, with a majority discontinuing due to GI intolerance. A limitation to the study design is that discontinuation rates due to GI intolerance may be falsely low, as patients had to tolerate therapy for at least 3 months in order to be included in the study. Thus, it is noteworthy that 43 patients were initially excluded from the study due to insufficient acarbose use and it is unknown if this was due to adverse effects.
Selection of the optimal oral agent for patients with elevated HbA1c results who are hesitant to start insulin is challenging. At our institution, acarbose is often added as a last-line, formulary agent. In this study, 26% of patients who were not on insulin at the time of acarbose initiation were eventually prescribed insulin therapy. By providing a trial of acarbose in patients with uncontrolled diabetes, time to appropriate therapy may be delayed, increasing risk for microvascular complications. Selection of therapy in patients with T2DM should be made with consideration of ability to reach HbA1c targets. Since the study timeframe, the oral formulary options within the Veterans Affairs system have expanded with the addition of saxagliptin to the national formulary. Thus, providers may now prescribe saxagliptin as an alternative to acarbose in patients on maximum doses of other formulary oral options who are hesitant to start insulin.
In addition to previously mentioned limitations of this study, others were also identified. Regarding the primary outcome, confounding variables may also have contributed to changes in HbA1c. Other medication changes for the management of T2DM that occurred during the study timeframe were not assessed. As a greater HbA1c reduction of 1.1% was seen in the subgroup analysis of patients on insulin compared to the 0.49% in patients not on insulin, it is likely that insulin dose adjustments were made within the timeframe of acarbose initiation. These dose adjustments in addition to any other medication changes that were not accounted for may have affected the HbA1c reduction seen with acarbose. Medication compliance was not assessed for acarbose or other medications for T2DM. Based on the evaluation of reasons for discontinuation of acarbose therapy, non-compliance appeared to be a contributing factor as many prescriptions were stopped due to not refilling the prescription, as evidenced by documentation of “Polypharmacy Policy” as reason for discontinuation of acarbose. This may have limited the HbA1c reduction seen in the study and may be a marker of medication intolerance. In addition, lifestyle changes were not assessed. Any improvement or worsening of lifestyle, including diet changes and amount of physical activity, could have impacted HbA1c results.
CONCLUSIONS
Hemoglobin A1c reduction with the addition of acarbose in patients at our institution is 0.65%, which is similar to the 0.5-0.8% decrease seen in previous trials. Acarbose can be considered as a last-line option in patients requiring minimal HbA1c reduction to reach their goal HbA1c. However, adverse effects often limit ability to titrate medication doses and may lead to discontinuation. Thus, the patient population where acarbose is an appropriate selection is limited. Potential risks and benefits of use should be assessed and discussed with the patient prior to prescribing acarbose.