INTRODUCTION
Aldosterone antagonists are commonly prescribed medications to reduce blood pressure while optimizing potassium level.1 Numerous studies have demonstrated the cardio-protective effects of aldosterone antagonists on cardiac patients2,3,4, this therapy may have a significant clinical impact on patients’ health outcomes independent of its effects on blood pressure.1
Current guidelines support the use of aldosterone antagonists in patients with moderate to severe HF and reduced left ventricular ejection fraction (LVEF).5 Aldosterone antagonists are considered as class IA, “useful and recommended” within the American Heart Association and the American College of Cardiology (AHA/ACC)5,6,7, and the European Society of Cardiology.8 While spironolactone is the most commonly used drug in this class, eplerenone is increasingly used in patients with HF following acute MI. Despite their recommendations by international guidelines, the use of aldosterone antagonists remains suboptimal in eligible patients. Previous studies revealed modest use in patients with HF.9 A large study from 219 hospitals in the USA suggested widespread under-use of aldosterone antagonists post MI, with only 9% of eligible patients receiving them.10 Recently, a national large cohort study revealed that aldosterone antagonists prescription decreased over time in patients with HF.11 Factors contributing to the discrepancy between current practice and evidence-based guidelines are unclear. The assessment of physicians and pharmacists’ knowledge of guidelines is important to narrow the treatment gap for use of aldosterone antagonists. In Jordan, awareness of evidence based guidelines among health care providers and practice of aldosterone antagonists in HF and post MI patients has not yet been explored.
The primary aims were to evaluate prescription of aldosterone antagonists in HF and MI patients, and to determine and compare physicians and pharmacists’ practices, and awareness of current guidelines pertaining to use of aldosterone antagonists in post-MI and HF patients.
METHODS
Ethical Approval
The study was approved by the institutional review board of King Abdullah University Hospital (KAUH) and Jordan University of Science and Technology (JUST). Individual approvals from included hospitals were obtained following approval from Ministry of Health and Royal Medical Services. The procedures followed were in accordance with the ethical standards of the Helsinki Declaration.
Eligibility and use of aldosterone antagonists in HF and MI patients
In an evaluation of current clinical practice, 408 patients who presented to the cardiology clinic at KAUH with history of HF, coronary artery disease (CAD), diabetes (DM), and hypertension (HT) were prospectively reviewed for eligibility and prescription of aldosterone antagonists. Use of all medications was evaluated at both admission and discharge after optimization of medical therapy.
Study Participants
Physicians and pharmacists working in major Jordanian hospitals were voluntarily invited to complete a cross sectional survey investigating their practices and awareness of guidelines related to use of aldosterone antagonists post MI and in HF. The study was performed between June 2013 and June 2014. A self-completed questionnaire specifically designed for this study was used. The questionnaire was assessed for content and face validity by academic experts and piloted by 10 participants at our institution (KAUH). A reliability test was carried out and produced a Cronbach’s alpha coefficient of >0.7.
Invited participants included all physicians (consultants, fellows and residents) and pharmacists/clinical pharmacists (pharmacists with BSc degree and PharmDs) working in cardiology and cardiac surgery departments who are involved in the care of cardiovascular disease patients. Cardiologists/internal medicine residents and cardiac surgeons/surgery residents were surveyed, as they guide the follow up care of post MI and HF patients and are responsible for medication prescriptions. Among residents, only those in the last 2 years of their residency in the surgery or internal medicine program, and who had finished their rotations or were rotating at the cardiology or cardiac surgery departments were included in this study. A written consent was obtained from all participants.
The questionnaire (online appendix) is comprised of 30 questions in four sections,regarding 1) demographics, 2) awareness and perceptions, 3) practice, and 4) awareness of current guidelines. Physicians and clinical pharmacists completed all sections; pharmacists working in pharmacies of cardiovascular departments who were less actively involved in practice omitted items 17-25 (practice).
The hospitals included in the survey were the main tertiary hospitals (public and private) in the north and middle of Jordan that provide cardiac care (# 8 hospitals). The same research assistant invited participants in all hospitals to avoid participant duplication. Survey non-responders were sent reminders by email, phone call or personal interaction.
Statistical Analysis
Data are presented as mean and standard error of the mean for continuous variables and percentages for categorical variables. Responses were entered into JMP 11 software (USA). Descriptive statistics were used to analyze proportions and frequencies. Statistical differences among groups were evaluated using Pearson’s chi-squared test. Graph Pad prism 5 was used to prepare figures. A p-value <0.05 was considered statistically significant.
RESULTS
We prospectively reviewed data for 408 patients who presented with HF, DM, HT, and CAD (Table 1). Among these, 97 patients (23.7%) presented with MI, 156 patients with DM (38.2%), 53 patients (12.9%) with moderate to severe HF (Stage C / D, or NYHA classes III / IV), and 270 (68%) presented with HT. Of the 408 reviewed patients, 30 patients (7.5%) were eligible for aldosterone antagonist treatment; among these, 22 patients were post-MI with HF or DM and reduced LVEF (≤40%)), and 8 were non-MI patients presenting with moderate to severe HF and reduced LVEF (EF≤35%). Of the eligible patients, only 4 patients received spironolactone at discharge (13.3%); 2 post-MI patients, and 2 non-MI patients with HF. One patient was on spironolactone at admission and remained on it at discharge. Most eligible patients were on and/or received at discharge guideline-based therapies for management of HF or MI (ACEIs/ARBs, aspirin, statins, and beta-blockers, Table 1).
Table 1 Patients characteristics
| All patients | n= 408 | |
|---|---|---|
| Demographics | ||
| Age, y | 56.46 [0.56] | |
| Male sex, n (%) | 289 (70.8) | |
| Body Mass Index, n (%) | 29.06 [0.29] | |
| Smoking | 171 (41.9) | |
| CAD ≥50% stenosis, n (%) | 231 (56.6) | |
| Myocardial infarction (MI) | 97 (23.7) | |
| Hypertension, n (%) | 270 (66.2) | |
| Heart Failure (NYHA class III/IV), n (%) | 53 (12.9) | |
| Diabetes mellitus, DM (%) | 156 (38.2) | |
| Ejection Fraction (%) | 51.8 [0.6] | |
| Aldosterone antagonist eligible | n=30 | |
| Age, y | 60.4 [2.04] | |
| Male sex, n (%) | 27 (90) | |
| HF with LVEF ≤35% | 8 (26.6) | |
| MI with LVEF≤40% and DM or HF | 22 (73.3) | |
| Potassium level (mmol/L) | 4.32 [0.08] | |
| Creatinine level (mmol/L) | 82.1 [1.7] | |
| Contraindication to aldosterone | 1 (3.2) | |
| Medication use in eligible patients (%) | Admission | Discharge |
| Aspirin | 18 (60%) | 29 (96.6) |
| ACEIs/ARBs | 10 (33.3) | 21 (70) |
| Beta-adrenergic receptor blockers | 13 (43.3) | 22 (73.3) |
| Aldosterone antagonists | 0 (0) | 4 (12.9) |
| Diuretics | 11 (36.6) | 9 (30) |
| Statins | 9 (30) | 27 (90) |
| Calcium channel blockers | 2 (6.6) | 2 (6.6) |
| Oral hypoglycemic drugs | 8 (26.6) | 8 (26.6) |
Values are expressed as mean [SEM], unless otherwise indicated. MI; myocardial infarction, CAD: coronary artery disease, HF: heart failure, DM: diabetes mellitus, ACEIs: angiotensin converting enzyme inhibitors, ARBs: angiotensin receptor blockers.
We designed a questionnaire to evaluate factors related to use of aldosterone antagonists in HF and post-MI patients. A total of 201 participants were eligible to complete the survey; 153 participants completed the survey and 48 did not (76.1% response rate). Respondents to the survey included 14 consultants: 7 cardiac surgeons and 7 cardiologists (groups 1, 2), 106 residents and fellows: 77 in the internal medicine program, 29 in the general surgery program, (groups 3, 4), 12 pharmacists (group 5) and 21 clinical pharmacists (group 6) (Table 2).
Table 2 Study Groups
| Groups | Number (%) | Age range (Years) | Males (%) | Experience (Years) |
|---|---|---|---|---|
| 1. Consultants, cardiac surgeons | 7 (4.6) | 40-60 | 7 (100) | 13.6 [1.7] |
| 2. Consultants, cardiologists | 7 (4.6) | 40-60 | 6 (85.7) | 10.3 [4.2] |
| 3. Residents/fellows, internal medicine | 77 (50.4) | <30-39 | 58 (75.3) | 3.1 [0.18] |
| 4. Residents/fellows, general surgery | 29 (18.9) | <30-39 | 22 (75.8) | 4.6 [0.57] |
| 5. Pharmacists | 12 (7.8) | <30-50 | 1 (8.3) | 7.2 [1.2] |
| 6. Clinical Pharmacists | 21 (13.7) | <30-50 | 1 (4.7) | 5.9 [1.0] |
Experience is presented as mean [standard error of the mean]
We evaluated participants’ awareness and perceptions regarding use of aldosterone antagonists (Table 3). A total of 111 participants (72.5%) were aware of studies regarding the cardio-protective use of aldosterone antagonist in HF and MI. Cardiologists, internal medicine residents/fellows, and clinical pharmacists were more aware than other groups (p= 0.0005, Figure 1 (A)).
Table 3 Knowledge and beliefs regarding use of aldosterone antagonists (%)
| Strongly agree | Agree | Neither agree nor disagree | Disagree | Strongly disagree | |
|---|---|---|---|---|---|
| In your opinion, is the use of aldosterone antagonists in post-MI patients with left ventricular dysfunction who also have HF or diabetes mellitus useful? | |||||
| 22.8 | 54.2 | 21.5 | 0.65 | 0.65 | |
| In your opinion, is the use of aldosterone antagonist in patients with moderately severe to severe HF (NYHA class III &IV) and reduced left ventricular ejection fraction (LVEF) useful? | |||||
| 25.5 | 54.9 | 16.9 | 1.3 | 1.3 | |
| In your opinion, is the use of aldosterone antagonists in HF or post-MI (patients of the above Qs) useful when patients are normotensive? | |||||
| 10.5 | 53.6 | 24.2 | 9.8 | 1.9 | |
| Are you aware of studies in the literature regarding cardio-protective use of aldosterone antagonists in patients with post -myocardial infarction (MI) or heart failure (HF)? | |||||
| Yes | No | Others | |||
| 72.5 | 27.5 | ||||
| Are you aware of studies which showed that use of aldosterone antagonists improves cardiac remodeling/oxidative stress, ventricular dysfunction and mortality? | |||||
| 55.5 | 39.2 | 5.2 | |||
| Are you aware of studies in the literature regarding use of aldosterone antagonists to prevent or treat cardiac arrhythmia? | |||||
| 12.4 | 87.6 | ||||
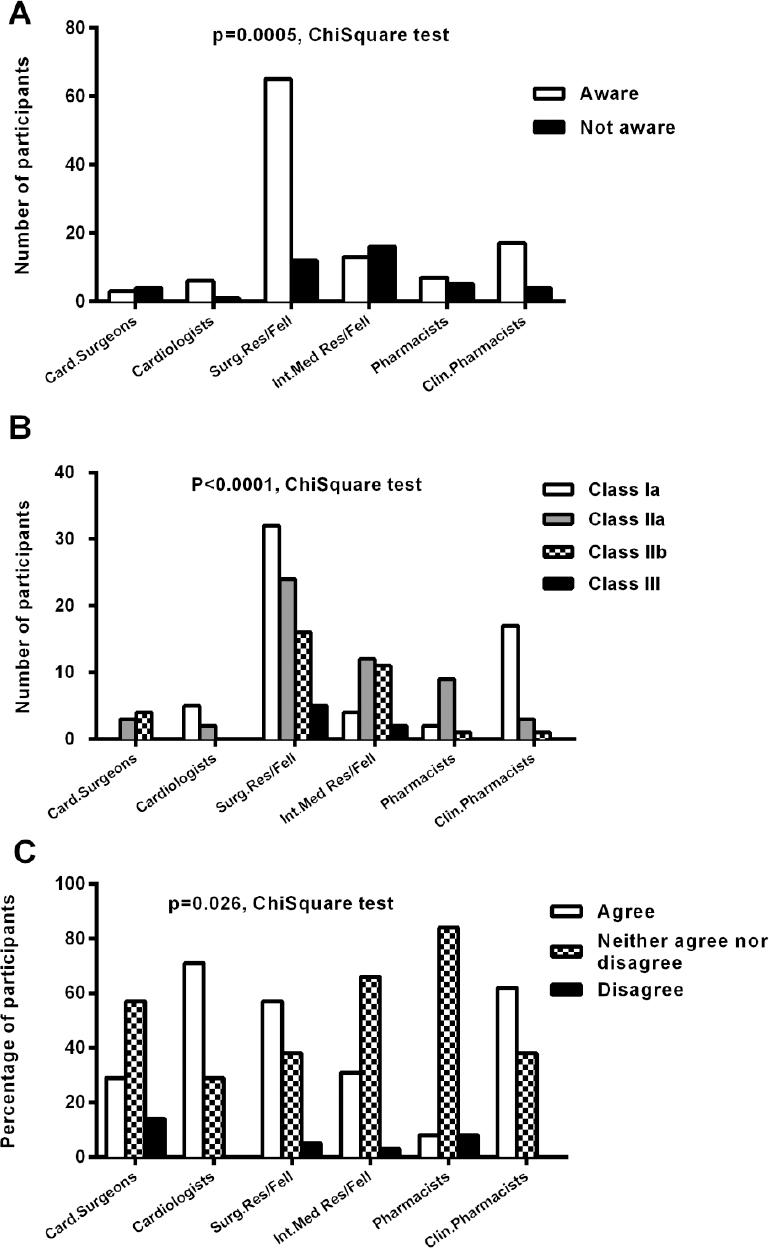
Figure 1 Awareness and knowledge of current guidelinesFigure 1-A summarizes responses to the question “Are you aware of studies in the literature regarding cardio-protective use of aldosterone antagonists in patients with post-myocardial infarction (MI) or heart failure (HF)?” among study groups (Gps).Figure 1-B summarizes responses to the question “The American College of Cardiology and the American Heart Association (ACC/AHA) consider adding spironolactone to standard therapy in moderately severe to severe HF patients (stage C or D) with reduced LVEF (EF≤35%) as?”Figure 1-C summarizes responses to the guideline “The AHA/ACC recommends adding eplerenone to standard therapy directly (within 2 weeks) post-MI in patients with reduced LVEF (EF≤40%) who also have HF or diabetes mellitus?” Card: Cardiac, Surg.Res/Fell: General surgery residents/fellows, Int.Med.Res/Fell: Internal medicine residents/fellows, Clin: clinical.
About 22.8% and 54.2% of participants either strongly agreed/agreed with the usefulness of aldosterone antagonist post-MI in patients with HF and/or DM (Table 3), without significant differences across the groups (p= 0.1487). Similar responses were reported on the utility of aldosterone antagonists in treating moderate-severe HF (Table 3). Consultants and pharmacists/clinical pharmacists were more aware than residents/fellows (p=0.0493). Only 10.4% strongly agreed that these agents are useful in HF and MI patients when they are normotensive (p=0.1155, Table 3).
In treating moderate to severe HF patients or post-MI patients with HF or DM, 75.2% reported that ACEIs/ARBs are usually prescribed as part of standard therapy, 70.6% reported routine use of beta-blockers, and 41.8% reported use of aldosterone antagonists. Interestingly, 35.9% were not aware if their institutions had a protocol for use of aldosterone antagonists in patients, and only 11.7% reported that they do have a protocol. Spironolactone was reported by 92.1% to be the most commonly prescribed drug. With respect to clinical indication, 54.5% consider prescribing aldosterone antagonists in HT patients with hypokalemia, 67.1% for cardio-protection in HF, and 47.7% post-MI (Table 4).
Table 4 Practice regarding use of aldosterone antagonists in HF and MI. (%)
| When do you consider using aldosterone antagonists? | |||||||
| In hypertensive patients with hypokalemia | 54.5 | ||||||
| In hypertensive patients in which diuretics are not sufficient or intolerant | 29.8 | ||||||
| In moderately severe to severe HF patients with low LVEF | 67.1 | ||||||
| For cardio-protection in post-MI patients with HF or diabetes | 47.7 | ||||||
| In patients with hyper-aldosteronism | 42.5 | ||||||
| I do not use these agents | 5.9 | ||||||
| If you are planning to use aldosterone antagonist in post-MI patients with HF and left ventricular dysfunction, when do you generally consider it? | |||||||
| Directly (within 2 weeks) following MI | 30.8 | ||||||
| A month after MI | 20.3 | ||||||
| Whenever use of standard therapy is insufficient to control LV dysfunction | 25.9 | ||||||
| Whenever blood pressure is not controlled by standard therapy | 4.2 | ||||||
| Others | 4.9 | ||||||
| I do not use it | 13.9 | ||||||
| If you plan to use aldosterone antagonist for cardio-protection in HF or post-MI, and the patient is taking ACEI or ARB, how would you use it? | |||||||
| Replace it with ACEI/ARBs | 5.6 | ||||||
| Add it to ACEI/ARB | 58.0 | ||||||
| Replace it with diuretic if the patient is taking diuretic | 11.9 | ||||||
| I do not consider patient drug therapy | 7.0 | ||||||
| I do not consider use of aldosterone antagonist | 17.5 | ||||||
| How often are aldosterone antagonists used as a routine care in your patients (regardless of the purpose, diuretic or non-diuretic indications)? | |||||||
| Always | Usually | Sometimes | Seldom | Never | |||
| 2 | 17.6 | 67.3 | 7.8 | 5.3 | |||
| Approximately, how many times do you consider aldosterone antagonist per week as a diuretic to lower blood pressure or optimize K+ levels? | |||||||
| 0 time | 1-2 times | 3-5 times | 5-10 times | >10 times | |||
| 16.1 | 34.2 | 22.4 | 19.6 | 7.7 | |||
| How many times do you consider using aldosterone antagonist per week as a cardio-protective drug but not diuretic in patients with HF or post MI? | |||||||
| 0 time | 1-2 times | 3-5 times | 5-10 times | >10 times | |||
| 18.9 | 44.0 | 13.3 | 16.1 | 7.7 | |||
| When you use aldosterone antagonist, do you use the same dose regardless of the indication (diuretic or cardio-protective indication)? | |||||||
| Yes | No | Others | |||||
| 25.9 | 68.5 | 5.6 | |||||
| Spironolactone is associated with increased risk of gynocomastia and hyperkalemia more than eplerenone? | |||||||
| Strongly agree | Agree | Neither agree nor disagree | Disagree | Strongly disagree | |||
| 13.3 | 62.2 | 21.7 | 2.1 | 0.70 | |||
With respect to the frequency of prescription, most participants (67.3%) reported that they sometimes prescribe aldosterone antagonists in practice (regardless of the indication, Table 4). Specifically, 34.2% reported that they consider aldosterone antagonists as diuretics once or twice per week, whereas 42% prescribe them 3-10x/week (Table 4). In contrast, aldosterone antagonist’ use as a cardio-protective medication in HF or post-MI is less frequent (Table 4); 44% reported prescribing it 1-2x/week and 29.4% prescribe it 3-10x/week. With respect to dosing, 25.9% reported that they consider the same dose of aldosterone antagonist regardless of the indication, Table 4.
Aldosterone antagonists are recommended directly (within 2 weeks) post MI.5 Only 30.7% (p<0.0001) consider adding aldosterone antagonist directly post MI (Table 4).
With respect to side effects, 13.3% and 62.2% strongly agreed / agreed that spironolactone is associated with gynecomastia more than eplerenone (p=0.1028, Table 4). In addition, 67.8% of participants reported that they monitor both [K+] and creatinine level when using aldosterone antagonists.
Current guidelines recommend adding aldosterone antagonists to standard therapy, including ACEIs or ARBs and recommend against adding them to combination of ACEIs and ARBs.5-8 Interestingly, 64.3% of participants reported that patient use of ACEIs/ARBs influenced their decision about whether or not to use aldosterone antagonists. Only 58% of participants consider adding aldosterone antagonists when their patients are on ACEIs/ARBs, whereas 17.5% do not consider aldosterone antagonist if their patients are already on ACEIs/ARBs (Table 4).
We evaluated the awareness of physicians and clinical pharmacists of recent guidelines5 regarding appropriate use of aldosterone antagonists in post-MI and in HF patients, Table 5. Only 39.2% of participants consider adding spironolactone to standard therapy in moderately severe to severe HF patients with reduced LVEF (≤35%) as class Ia (useful and recommended). On the other hand, 34.6% consider this practice as class IIa (most of the time useful), 21.6% as class IIb (not sure if useful), and 4.5% as class III (not useful and not recommended). Cardiologists and clinical pharmacists were most aware of this guideline (p<0.0001, Figure 1 (B)). On the other hand, 48.3% agree that eplerenone should be added to standard therapy directly (within 2 weeks) post-MI in patients with reduced LVEF (EF≤40%) who also have HF or DM, Table 5. Cardiologists, internal medicine residents and clinical pharmacists were most aware of this guideline (p=0.0266, Figure 1 C). With respect to dose, 55.6% agreed that the recommended daily dose of spironolactone in congestive HF or post MI is 25-50 mg, but higher doses are typically used in HT, Table 5.
Table 5 Knowledge of guidelines regarding use of aldosterone antagonists. (%)
| Agree | Neither agree nor disagree | Disagree | |
|---|---|---|---|
| Aldosterone antagonists should not be used in patients with significant renal dysfunction (e.g. creatinine >2.5 in men or >2.0 mg/dl in women) or hyperkalemia (K+ level >5.0 mEq/L)? | |||
| 80.4 | 16.3 | 3.3 | |
| Risk of hyperkalemia increases with concomitant use of aldosterone antagonists with ACE inhibitors/ARB or Non-Steroidal Anti Inflammatory Drugs (NSAID) | |||
| 77.8 | 19.6 | 2.6 | |
| The recommended cardio-protective daily dose of spironolactone in congestive HF or post-MI is 25-50 mg, but the dose used in hypertension is usually 50-100 mg? | |||
| 55.6 | 37.9 | 6.5 | |
| The AHA/ACC recommends adding eplerenone to standard therapy directly (within 2 weeks) post-MI in patients with reduced LVEF (EF≤40%) who also have HF or diabetes mellitus? | |||
| 48.3 | 47.1 | 4.6 | |
Most of participants were aware of contraindications of aldosterone antagonists in significant renal dysfunction, Table 5.
DISCUSSION
In this study, we sought to evaluate prescription of aldosterone antagonists in HF and post-MI patients, and compare awareness and practices regarding the cardio-protective use of aldosterone antagonists among physicians and pharmacists working in cardiovascular departments of major hospitals in Jordan. This study revealed a general lack of awareness of current guidelines, which might affect the use of aldosterone antagonists and the primary care of cardiac patients.
Recent ACC/AHA guidelines recommend use of spironolactone in stage C and D HF (NYHA class III and IV) and eplerenone directly post MI in patients with HF or DM and low LVEF.5-8. At a major hospital in Jordan, we found that spironolactone is under prescribed in eligible patients, with only 13.3% of those eligible receiving it. This usage rate is similar to the rate previously reported in the USA.10 Most of health care providers reported use of aldosterone antagonist sometimes in practice; their use as diuretics to optimize [K+] was more frequent than their use as cardio-protective medications post MI and in HF. We observed a lack of awareness regarding their usefulness in normotensive MI or HF patients, with only 10.5% / 53.6% strongly agreeing / agreeing on their usefulness in this subpopulation. This suggests that appropriate aldosterone antagonist use is perceived to require the presence of HT. In addition, 25.9% of participants reported the use of the same dose, regardless of the indication, suggesting a lack of knowledge regarding dosing of these medications. This was also confirmed by their responses to current dosing guidelines. Additional important aspects of dosing include the timing and possibility of drug-drug interaction. Around 52% of participants were unaware that these agents should be added to standard therapy within 2 weeks post-MI, even when the patient is taking an ACEI. In addition, most participants were unaware about how to prescribe aldosterone antagonists when a patient is on an ACEI, with many suggesting replacing it with ACEI or not using aldosterone antagonist if the patient is taking ACEI/ARBs, suggesting that some participants think that both agents have similar effects and mechanisms.
Despite that 72% of participants have general awareness of studies investigating the utility of aldosterone antagonists post-MI and in HF, there was a significant lack of detailed awareness of current guidelines. In particular, only 39.2% agreed on the current AHA/ACC classification of aldosterone antagonists in HF as “useful and recommended.” In contrast, there was greater awareness of their contraindication in the setting of significant renal insufficiency and hyperkalemia.
This study revealed that cardiologists, internal medicine residents and clinical pharmacists were significantly more aware of current guidelines than cardiovascular surgery consultants/residents and pharmacists. The low prevalence of eligible patients, the lack of clinical experience and infrequent interaction of surgery residents or cardiac surgeons with such patients, lack of time to filter the literature, and the lack of detailed knowledge of usage indications, dosing and timing might contribute. In addition, the lack of written protocols on how to use these agents may play a major role, as only 11.7% reported the presence (or awareness) of local usage protocols. Reservations about risk due to hyperkalemia and polypharmacy may also contribute to low prescription rates.12 In this setting, it may be helpful for clinical pharmacists and pharmacists to take a more active educational and professional role. Clinical pharmacists may improve patient outcomes by discussing the recommended medications and doses with physicians that may have been overlooked. Establishing detailed protocols based on evidence-based medicine, clinical experience therapeutic interchange, and professional judgment could also help.13
Limitations
This study is limited by the relatively small number of consultants who participated. To our knowledge, this is the first study in Jordan and the Middle East to investigate current practice and knowledge among health care providers of aldosterone antagonists’ use in post-MI and HF. Collaborative international studies with larger sample size are required to evaluate the prescription of aldosterone antagonists among eligible patients. The findings of this study call for educational programs that emphasize the benefit of aldosterone antagonists, disseminating current guidelines, and encouraging other healthcare professionals to collaborate and prescribe them when needed.
CONCLUSIONS
There is an under-use of aldosterone antagonists in post-MI and HF patients and a lack of detailed awareness of current guidelines related to use of aldosterone antagonists among health care providers. Cardiologists and clinical pharmacists are most aware of guidelines. By more actively disseminating appropriate use of guidelines during their interactions with health care professionals, they may significantly improve patient management and outcomes.














