INTRODUCTION
In hospital setting in Thailand, patients play a limited role in administration of their own medications while in the hospital as medication administration is mainly responsible by nurses.1 Pharmacists' roles for in-patient service are restricted to medication review, drug use evaluation, monitoring, and discharge counseling. In comparison with nurse-administered medication, self-administered medication (SAM) reduces omitted dosing and medication errors in hospitals and increases patient medication knowledge, adherence, and satisfaction; therefore, it has been encouraged in many hospitals worldwide.2 3 4-5 Patient's self-administration could save 70 minutes/day for nurses to spend their time in informing patients on their medication.6 Despite evidence on benefits, SAM implementation among in-patient service has still been limited, including in Thailand.4,7 8-9 It was, therefore, not surprising that patients were lacking knowledge on medication side effects and on how to take medication after hospital discharge which could lead to non-adherence, drug related problems, or readmission.3,10 11-12 A study conducted phone interview within 48 hours after discharge from a medical ward reported that only 43% of patients could specify the name of all medications received and 36% could specify the indications of the prescribed medications.13 SAM program may involve pharmacists, nurses, or both to educate medication administration to the patient on a case-by-case basis.4,14,15 SAM education conducted by clinical nurses often only provides simple drug-related information, but simplifying the drug regimen, an important component of the program's success, is more likely to occur if a pharmacist has participated in the multidisciplinary medication education program.14,16The national statistical office of Thailand recently reported that Thailand would become a complete aged society in the year 2021, and a super aged society in the year 2031.17 In an aging society, patients are more likely to have chronic health problems, thus requiring more long-term medication than ever.18 Effective medication management may reduce unnecessary treatment episodes and hospital readmissions.12 A large systematic review evaluating the effects of SAM confirmed that patients participated SAM program increased medication knowledge, but the effects on side effects, compliance or medication errors, were inconclusive.19This might be a result of limited number of high quality studies and substantial methodological and clinical diversities across studies. This study, therefore, aimed to evaluate the efficacy of SAM education, mainly performed by a pharmacist, compared with routine nurse-administered medication among limited literacy patients with chronic diseases using a PROBE design. The primary objective was to compare patient knowledge about medication between the study group and the control group at hospital discharge. The secondary objectives were to compare (1) patient knowledge about prescribed medications measured at the first two follow-up visits, (2) adherence to prescribed medications measured at the first two follow-up visits, (3) medication error (administration error) while in hospital, and (4) hospital readmission within 60 days after discharge between the study group and the control group. The time nurses and pharmacists required for medication management was compared between groups.
METHODS
This was a controlled, parallel trial using PROBE (prospective randomized, open-label, blinded endpoint evaluation) design. The study protocol was approved by the Ethics Committee, Faculty of Pharmaceutical Sciences, Prince of Songkla University (reference no. 0521.1.07/1523, approval date was August 27, 2018). The study protocol had not been registered in clinical trial registries.
Participants
This study was conducted in a 60-bed community hospital located in southern Thailand near the Malaysian border, where 96.7% of population were Muslims and most of them used the local Malay language. Most of them were limited literacy in Thai and English. Patients admitted to male or female medical wards between October 2018 and March 2019 were the accessible population. The adult patients (aged 18 to 75 years old) diagnosed with at least one chronic disease (acute coronary syndrome, stroke, atrial fibrillation, heart failure, hypertension, diabetes mellitus, dyslipidemia, gout, chronic kidney disease, asthma, chronic obstructive pulmonary disease, thyroid dysfunction, thalassemia, HIV, or tuberculosis) were eligible for enrollment in the study. Patients were excluded if they met any of the following: Glasgow coma scale score less than 15 points, history or evidence of suicide, drug/alcohol abuse or uncontrolled psychiatric disorders.
Prior to participation to any study procedure, each patient was given a participant information sheet (PIS) which provided detailed information about the study. Written informed consent was obtained if the patient was willing to participate in the study after they thoroughly understood the information in the PIS, or the information was clearly explained as required by the research pharmacist.
Interventions
Study (SAM) group: Patients in the study group received in-patient SAM education. On the first day of hospital admission, the research pharmacist provided medication information (i.e. medication name, purpose, dose, frequency, dosing time related to meal, and side effects) to each patient on a one-to-one basis. The teaching materials as well as the medication labels were available in both text and symbols/images, instead of using only text, to increase patient understanding. Symbols/images included were: a circle (whole tablet), a semi-circle (half-tablet), one fourth-circle (one quarter-tablet), a star-shape (at bedtime), and a water glass (before meals). After the consultations, patients administered the prescribed medications on their own while in the hospital under the supervision of a multidisciplinary team consisting of medical, pharmacy and nursing staff. An alarm prior to each dosing notified a registered nurse to reach the patient's bed within 10 minutes. The patient was allowed to call the nurse if she did not arrive within 10 minutes after the alarm. Prior to each dosing, a registered nurse checked whether the patient picked up the medications correctly as prescribed. The role of nurses was to ensure that patients could administer medications safely. If the patient picked up the dose or the medications incorrectly, the attending nurse notified the patient to replace the incorrect dose or medications with the correct ones before dosing. The nurse subsequently consulted the research pharmacist to intervene with that patient thereafter. It was possible that some patients required consultation regarding the drug regimens with the research pharmacist more than once. Self-administered medications were limited to oral medications only. All oral dosing medications were placed in a box with a lid at a bedside locker. IV medications, PRN or opioid medications were stored in the medication cabinet in the ward and were administered by the nurses if required. The number of dosages per dispense was 4 days. If there were any changes of the regimens the patient was firstly notified by the medical doctor and subsequently educated by the research pharmacist prior to self-administration of the relevant medications. The pharmacy immediately managed the pill box according to the doctor's order. At each dosing time, the nurse checked the remaining tablets to monitor patient adherence. Patient self-administration medication as well as dosing time was recorded in the medication administration record (MAR) immediately after each dosing by an attending nurse. This information was subsequently verified for identification of medication administration errors by the research pharmacist.
Control group: Pharmacists dispensed unit dose medications that were stored at the medication carts in the ward. Dispensing from the pharmacy department was done once a day. At the time of dosing, the nurse arrived at the patient's bed with the MAR and delivered a unit dose of prescribed medications to each patient in the control group, as routine practice. The nurse provided both written (texts only) and verbal essential medication information needed for dosing to each patient (dose, purpose, time related to meal, and side effects). The research pharmacist, was accessible to patients in the control group, but extra medication information, other than that provided by nurses, was not provided to the patients. Medication administration was recorded in the same manner as described above.
Outcomes
Primary outcome was knowledge of the prescribed medications measured at hospital discharge. Secondary outcomes were (1) prescribed home medication knowledge measured at the first two follow-up visits; (2) patient medication adherence measured at the first two follow up visits; (3) medication errors (administration errors) while in hospital, and (4) hospital readmission over 60 days after discharge. Effects of SAM on nurse and pharmacist workload regarding medication dispensing, checking, and administering/supervising were measured as time required for performing these activities.
Assessment of medication knowledge: At discharge, patients in both groups were given the same medication packages i.e., blisters of individual medications put in separate zip-locked bags labelled with texts and symbols/images, which were the same as those dispensed for the in-patients in the study group. The labels of discharged medications were different from those the patients received prior to admission that contained only texts. Patients in both groups were allowed to use medication information labelled on the packages while answering the questions about their medications. Medication regimen data were retrieved from the computerized hospital database, printed out and reviewed by outcome assessors. Medication-related knowledge was assessed by asking each patient about their medication name, indication, dose, dosing frequency, dosing time related to meal, and side effects. Each question was given a weighted score based on its safety-related importance; medication name and side effects was given 1 point each, and the others (indication, dose, dosing frequency, and dosing time related to meals) were given 2 points each. The possible maximum score was 10. For 2-point questions, the patient received 2 points for the correct and complete answer, 1 point for partially correct answer and zero points for wrong answer. The 1-point question was rated in the same manner, i.e. 1 point for the correct and complete answer. In patients receiving more than one medication, the average score was used for analysis. Assessment of medication knowledge at each of the first two follow-up visits after discharge was done in the same manner.
Assessment of patient medication adherence: Patient adherence to medication was assessed using the pill count method. The percentage of the number of tablets/capsules consumed from the total amount prescribed was calculated for each patient. Medication adherence was assessed at the first and at the second follow-up visits after hospital discharge.
Assessment of medication errors: The study measured only administration errors, which might be classified as any of the following: omission dose, wrong drug, unordered drug, wrong patient, wrong-dose or wrong-strength, wrong-route, wrong-time, extra-dose, or wrong dosage-form. Wrong-time error was defined as a deviation of administration time more than 30 minutes from the scheduled time. The clinical risk of the event was rated into 9 levels (Level A to Level I) according to National Coordinating Council for Medication Error Reporting and Prevention (NCC MERP) Index.20
Hospital readmission after discharge: To measure the effect of SAM intervention on therapeutic outcome, hospital readmission was collected over 60 days after discharge. The length of time selected was related to the time the patients completed the second follow-up visit. The dates and causes of hospital readmission were recorded.
Staff workload and time spent on medication management: Data about staff (nurses and pharmacists) workload and time spent on medication management, based on 15 beds per day in each group, were measured. Nurse workload was measured as the time required for medication checking (for all patients in each of the two groups), administering (the control group), and supervising (the study group). Pharmacist time included the time spent on medication dispensing (for all patients in each of the two groups), and inpatient SAM educating (the study group).
Randomization
Patients were randomly allocated to either the study (SAM) group or the control group using stratified block randomization. Randomization was stratified by educational level (not higher than primary school or secondary school or higher) and age groups (<40 years, 40-60 years, or >60 years). These two stratifying variables were considered potential confounders for the outcomes measured and thus required to be balanced at baseline. The blocks of size 4 and 6 were used for generating the random allocation sequence for each of 6 strata, (allocation ratio 1:1), the sequences were put in sequentially numbered opaque containers until interventions were assigned. Random allocation sequence was generated manually by the co-investigator. Participant enrollment and assignment to intervention were performed by principal investigator. The randomized sequence was securely stored in the locker located in the in-patient pharmacy room and maintained by the third party. Allocation of the patients could not be influenced by the investigator, and selection bias was unlikely to occur.
Sample size
The variance of the estimate (mean difference) was not identified from previous studies. The difference of 1.5 points out of 10 in medication knowledge, and 12% in medication adherence were considered clinically significant. The sample size calculation assumed the effect size (group mean difference/standard deviation) of 0.75, with a power of 80%, and type I error at 5% (two-sided test). The study assumed a dropout rate of 20%; therefore, seventy (35 per group) patients were required for the study.
Blinding
The study was designed as a single blinded trial, i.e. only outcome assessors were blinded to the treatment status. There were 2 independent outcome assessors, one working in the in-patient pharmacy service and the other working in the out-patient pharmacy service. These two assessors were not involved in the intervention process. They were well trained on how to assess the outcomes and how to use the research tools. Blinding to patients' treatment status was successful as computerized hospital prescription database did not indicate the way the medications were supplied to each patient, either the 4-day dispensing or the daily unit-dose dispensing. Outcome assessors did not involve in the dispensing process done for the patients participated in the present study. In addition, identification of the treatment groups could not be identified by discharge medications as they were packed and labeled in the same manner.
Research tools
The case record form and outcome assessment manual were approved by the Ethics committee. It recorded patient identification numbers, socio-demographic data (i.e., sex, age, education level), inclusion and exclusion criteria checklist, main diagnosis, main cause of admission, underlying diseases, number of medication items before admission, number of home medication items, visual capability, hearing capability, language, caregivers, and length of hospital stay. The number of times each patient in the study group was given counseling by the research pharmacist was also recorded. Outcome data for each patient were recorded as specified in the outcomes section.
Statistical analysis
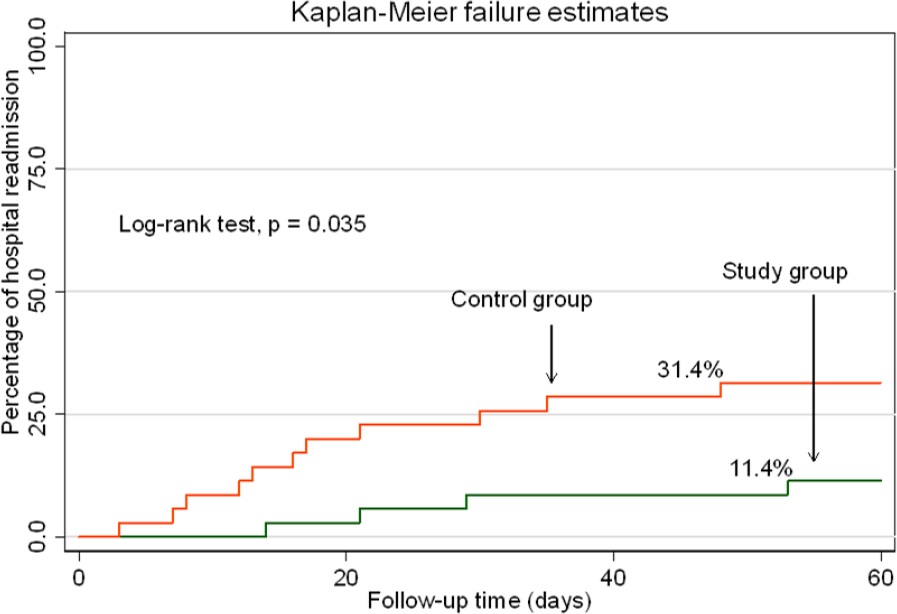
Descriptive statistics were used to summarize patient baseline characteristics. All analyses were based on intention-to-treat population. For comparison of the study outcomes, an unpaired t-test was used if the data were normal; otherwise Mann-Whitney U-test was used instead. Group mean difference and 95%CI were estimated where appropriate. Adjusted analysis was performed, if required, to examine the effects of the differences in baseline variables. Kaplan-Meier failure estimate was performed posteriori to examine the probability of hospital readmission over 60 days after hospital discharge. P-values <0.05 were considered statistically significant. All analyses were performed using Stata SE (Version 15.0), StataCorp LP, USA).
RESULTS
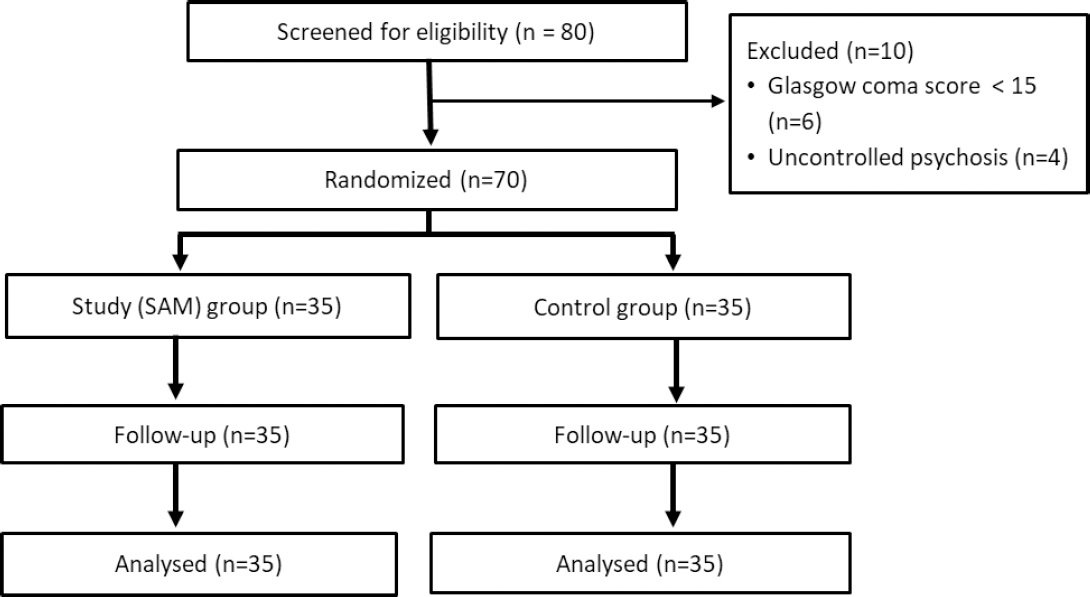
Eighty in-patients admitted to male or female medical wards were screened between October 2018 and March 2019. Seventy patients were eligible and randomized, 35 patients in each group; all received complete follow-up (Figure 1). Ten patients were excluded due to a Glasgow coma score less than 15 (n=6) and uncontrolled psychosis (n=4). The time from hospital discharge to the first follow-up visits was approximately 2 weeks. Average time from hospital discharge to the second follow-up visit was slightly longer in the study group (68.8 days) than in the control group (55.0 days).
Patients in both groups were balanced at baseline (Table 1). Mean (SD) age (years) were 59.2 (11.0) for the study group and 58.3 (12.0) for the control group. Percentages of females were 54.3 and 60.0 in the study group and the control group, respectively. The major causes of hospital admission were hyperglycemia, acute exacerbation of COPD, and hypertensive urgency. Most of them had comorbidities; approximately a half of participants in both groups had at least two comorbidities. Two-thirds of both groups were educated not higher than primary school. However, they had fair medication knowledge at baseline, group means 6.4 and 6.6 (of maximum possible score 10) for the study group and the control group, respectively. The numbers of medication items before admission in both groups were similar, with the average being approximately 5 items. Most had good visual and hearing capabilities. The majority were Muslim. All, except one in the study group, speak Malay, and approximately half speak Thai. A higher percentage of self-care was noted in the study group, the difference was only borderline. The average length of hospital stay were 3.0 (SD=2.5) and 3.2 (SD=2.4) days in the study group and the control group, respectively. The average number of times drug administration counseling was provided to the patients in the study group was 1.4 times (median 1, range 1-3). The number of doses administered by patients in the study group while in the hospital had a mean of 8.3 (SD=7.3) doses, a median of 6, and a range of 1-42. The number of doses administered by nurses in the control group while in hospital had a mean of 9.9 (SD=8.5) doses, a median of 6, and a range of 1-36.
Table 1. Baseline characteristics of study sample
| Variable | Statistic | |
|---|---|---|
| Study group (n=35) | Control group (n=35) | |
| Sex, n (%) | ||
| Female | 19 (54.3) | 21 (60.0) |
| Age, mean (SD), years | 59.2 (11.0) | 58.3 (12.0) |
| Cause of admission, n (%) | ||
| Hyperglycemia | 8 (22.9) | 7 (20.0) |
| Acute exacerbation of COPD | 7 (20.0) | 5 (14.3) |
| Hypertensive urgency | 7 (20.0) | 8 (22.9) |
| Congestive heart failure | 5 (14.3) | 4 (11.4) |
| Chronic kidney disease | 3 (8.6) | 5 (14.3) |
| Others | 5 (14.3) | 6 (17.1) |
| Number of comorbidities, n (%) | ||
| 0 | 1 (2.9) | 4 (11.4) |
| 1 | 13 (37.1) | 12 (34.3) |
| 2 | 19 (54.3) | 17 (48.6) |
| 3 | 2 (5.7) | 2 (5.7) |
| Education level, n (%) | ||
| Primary School or lower | 21 (60.0) | 21 (60.0) |
| Secondary School or higher | 14 (40.0) | 14 (40.0) |
| Number of Drug items before admission, mean (SD), [median, range] | 4.9 (2.0), [5, 2-11] | 4.66 (2.2), [4, 1-10] |
| Visual capability, n (%) | ||
| Normal | 27 (77.1) | 29 (82.9) |
| Myopia or Presbyopia | 8 (22.9) | 6 (17.1) |
| Hearing capability, n (%) | ||
| Normal | 33 (94.3) | 34 (97.1) |
| Poor | 2 (5.7) | 1 (2.9) |
| Language, n (%) | ||
| Thai | 1 (2.9) | 0 (0) |
| Malay | 19 (54.3) | 13 (37.1) |
| Thai and Malay | 15 (42.9) | 22 (62.9) |
| Caregiver, n (%) | ||
| Self-care | 32 (91.4) | 26 (74.3) |
| Spouse | 1 (2.9) | 3 (8.6) |
| Daughters or sons | 2 (5.7) | 6 (17.1) |
| Medication knowledge before admission, mean (SD) | 6.4 (1.2) | 6.6 (0.7) |
| Length of hospital stay (days), mean (SD), [median, range] | 3.0 (2.5), [2, 1-14] | 3.2 (2.4), [2, 1-10] |
Abbreviations: SD=Standard Deviation
Patient medication knowledge at hospital discharge in the study group was significantly higher than that in the other (median 8.56 vs 6.18, respectively, p<0.001) (Table 2). The study group achieved a higher score in every aspect measured, except medication name (mean 0.05 (SD=0.15) point for the study group and zero points for the control group) which might be due to the medication labels usually being presented in English while nearly all of the patients were unable to read English. All patients in the SAM group reached the maximum score (2 points) regarding knowledge about medication dose and dosing frequency at hospital discharge (Table 2). Likewise, knowledge on medication indication and time of dosing related to meals reached the maximum score in most patients. SAM slightly increased knowledge on medication side effects (mean 0.47 out of 1 score). The patients had knowledge about common side effects, but they did not know all the side effects that were measured for their medications. Knowledge of medication among patients in the control group (mean 6.40 (SD=0.78)) was similar with that measured at baseline (mean 6.56 (SD=0.67)). It was noted that patients in the control group had quite good knowledge on medication dose, dosing frequency, and time of dosing related to meals (Table 2). Discharged medications were very similar to those patients had received before admission in both groups. Although patients in both groups were allowed to use medication information labelled on the discharged medication packages, those in the control group were not familiar with symbols/images added as they had never seen and could not use the information properly.
Table 2. Patient medication knowledge, adherence, and medication errors
| Mean (SD) [Median (range)]* | Study group (n =35) | Control group (n =35) | mean difference (95% CI)* | p-value |
|---|---|---|---|---|
| Primary outcome | ||||
| Medication knowledge at hospital discharge | 8.59 (0.38) [8.56 (8.00-9.48)] | 6.40 (0.78) 6.18 (5.00-8.00) | < 0.001a | |
| Name | 0.05 (0.15) | 0.00 (0.00) | ||
| Indication | 1.96 (0.13) | 0.94 (0.57) | ||
| Dose | 2.00 (0.00) | 1.88 (0.26) | ||
| Frequency | 2.00 (0.00) | 1.70 (0.38) | ||
| Time related to meals | 1.97 (0.12) | 1.70 (0.33) | ||
| Side effect | 0.47 (0.32) | 0.04 (0.13) | ||
| Secondary outcomes | ||||
| Medication knowledge at the first follow-up visit | 8.46 (0.42) [8.40 (7.66-9.45)] | 6.52 (0.72) [6.53 (5.00-8.00)] | < 0.001a | |
| Name | 0.04 (0.11) | 0.00 (0.00) | ||
| Indication | 1.96 (0.13) | 0.96 (0.60) | ||
| Dose | 2.00 (0.00) | 1.90 (0.20) | ||
| Frequency | 2.00 (0.00) | 1.75 (0.36) | ||
| Time related to meals | 1.98 (0.08) | 1.70 (0.42) | ||
| Side effect | 0.34 (0.35) | 0.02 (0.07) | ||
| Medication knowledge at the second follow-up visit | 8.28 (0.46) [8.25 (7.20-9.16)] | 6.30 (0.77) [6.26 (4.50-7.89)] | ||
| Name | 0.00 (0.00) | 0.00 (0.00) | ||
| Indication | 1.93 (0.17) | 0.76 (0.59) | ||
| Dose | 2.00 (0.00) | 1.90 (0.20) | ||
| Frequency | 2.00 (0.00) | 1.75 (0.40) | ||
| Time related to meals | 1.99 (0.06) | 1.71 (0.29) | ||
| Side effect | 0.20 (0.36) | 0.01 (0.08) | ||
| Adherence to medications at the first follow-up visit | 92.50% (5.33%) | 79.60% (5.96%) | 12.90% (10.20%:15.60%) | < 0.001b |
| Adherence to medications at the second follow-up visit | 91.19% (6.24%) | 79.14% (7.97%) | 12.05% (8.64%:15.46%) | < 0.001b |
| Medication (administration) errors while in hospital, n/Nc(%, 95%CI) | 0/701 (0.00%, 0.00%:0.52%)d | 13/877 (1.48%, 0.79%:2.52%) | 1.48% (0.68%:2.28%)e | 0.001b |
| Hospital readmission within 60 days after discharge, n/N (%, 95%CI) | 4/35 (11.4%, 3.2%:26.7%) | 11/35 (31.4%, 16.9%:49.3%) | 20.0% (1.4%:38.6%) | 0.039f |
| Nursing time on medication checking, ming | 15.5 (1.9) [14.9 (13.8-18.3)] | 40.5 (2.8) [40.5 (37.2-43.8)] | -25.0 (-29.1:-20.9) | < 0.001b |
| Nursing time on medication supervising, ming | 124.0 (4.8) [125.3 (117.4-128.0)] | 205.1 (5.6) [204.6 (199.0-212.4)] | -81.1 (-90.2:-72.0) | < 0.001b |
| Pharmacist time on medication supply, ming | 92.6 (4.3) [93.0 (87.5-96.7)] | 181.0 (4.0) 180.9 (176.5-185.6)] | -88.4 (-95.7:-81.1) | < 0.001b |
| Pharmacist time on SAM education, ming | 33.2 (4.8) [33.2 (27.7-38.5)] | - | - | - |
*Otherwise specified;
aMann-Whitney U test;
bUnpaired t-test;
cNumber of administration errors/number of total administered doses;
dOne-sided 97.5%;
ePercentage mean difference (95% CI);
f1-sided Fisher exact test;
gBased on 15 beds in each group.
Patient medication knowledge measured at the first follow-up visit after hospital discharge remained significantly higher in the study group than that in the control group (medians 8.40 and 6.53, respectively, p<0.001), and sustained at the second follow-up visit (Table 2). The knowledge about medication remained the same in both groups compared with that measured at hospital discharge. The knowledge on medication name was still low in both groups and unchanged compared with those measured at hospital discharge. No intervention other than routine counseling practice was provided at each visit. Medication knowledge was not systematically assessed to identify the areas of knowledge that the patients should be improved during the routine counseling process. In-patient SAM intervention provided additional medication knowledge that could not be obtained from the routine practice.
Patient adherence at the first follow-up visit after discharge was higher in the study group than that in the control group. Percentage means were 92.50 (study group) and 79.60 (control group), percentage mean difference 12.90, [95%CI 10.20:15.60], p<0.001 (Table 2). Similarly, the corresponding figures at the second follow-up visit were 91.19, 79.14, and 12.05 [95%CI 8.64:15.46], p<0.001. Medication adherence was expected to maintain over time in the SAM group. Medication adherence in the control group that was relatively high at the first follow-up visit, no change was observed at the second follow-up visit. As a higher percentage of self-care was noted in the study group, an adjusted analysis was done to examine the effect of the difference in percentages of self-care between groups on medication adherence. However, imbalanced distribution of self-care in the two groups did not significantly confound the results.
Only administration errors were measured in this study. The estimate was the mean percentage of the doses administered where administration errors occurred while in the hospital. Very few administration errors were identified (Table 2). No administration errors were found in the study group, while 13 events were reported in 4 patients in the control group. All administration errors were “wrong time” medication administration initiated by nurses. For determining “wrong time” administration errors, the study allowed half an hour time deviation from that specified in the doctor's order sheet. Having the patients initiated their medication management and the nurses' role was as supervisory to correct any potential errors that were about to be made and therefore preventable. In the present study, patients in the study group were allowed to alert nurses in case nurses were engaged with an urgent task and did not arrived at the patients within 10 minutes of the scheduled time for dosing, wrong-time medication administration errors were therefore preventable. While all wrong-time administration errors found in the control group were originated by the nurses as they were being interrupted by unexpected and urgent tasks at the time of dosing. Eight events were classified as level C regarding NCC MERP index, but none caused harm to patients.20The remaining 5 events were level D medication errors (skipping the doses) which caused minor harm and required safety monitoring for patients.
Hospital readmission after discharge Impact of the intervention on therapeutic outcome, a percentage of readmission within 60-days after hospital discharge was performed. A significantly lower readmission among patients in the study group compared with that in the control group 11.4% (4/35) versus 31.4% (11/35), p=0.039, one-side Fisher's exact test) was observed (Table 2). The cause of hospital readmission was the same as that leading to previous admission in each and every patient. Kaplan-Meier curves showed that patients in the control group were readmitted earlier (the first case on day 3 after discharge) than patients in the SAM group (the first case on day 14 after discharge) (Figure 2). Within 20 days after discharge, 7 (20.0%) of patients in the control group and 1 (2.9%) of the SAM group were re-hospitalized. The results confirmed a positive effect of SAM on clinical outcomes.
SAM substantially reduced the amount of time nurses spent on medication management (checking, administering, and supervising). Based on 15 beds in each group, nurses required 25 minutes per day less on medication checking process for patients in the SAM group than that for the control group, p<0.001 (Table 2). Additionally, prior to each medication administration, time spent each day for supervising/ensuring patients taking self-managed medications in the SAM group was 81.1 minutes less, compared with that spent for medication distributing and dosing for patients in the control group, p<0.001. Overall, time nurses required for medication administration process was 2.3 hours per day for the SAM group and 4.1 hours per day for the control group. SAM saved overall nursing time on medication management 1.8 (95%CI 1.7:1.9) hours each day, p<0.001. Furthermore, time (minutes per day) pharmacists spent on medication dispensing process were 92.6 (4.3) for the study group, and 181.0 (4.0) for the control group, p<0.001. However, time the ward pharmacist required for educating patients on self-managed medication was 33.2 (4.8) minutes per day. Overall time (hours per day) pharmacists spent on medication dispensing and educating were 2.1 (study group) and 3.0 (control group). SAM significantly saved overall pharmacist time on medication management 0.9 (95%CI 0.7:1.1) hours each day, p<0.001. Time the pharmacist spent on educating the patients about their medications was relatively short as all patients were familiar with most of their medications they had previously used before admission. However, time needed for educating patients on new medication regimens might be greater. The present study demonstrated that SAM intervention significantly reduced nurse and pharmacist time spent on medication management, staff workload might not be the barriers on implementation of the SAM program.
DISCUSSION
SAM education significantly increased in-patient medication knowledge at hospital discharge compared with nurse administered medication (routine practice). The effect retained over the first two follow-up visits, approximately 2 months after hospital discharge. SAM also increased home medication adherence measured at the first follow-up visit and sustained at the second follow-up visit. Medication errors, focusing on administration errors, initiated by patients were not found in the study group, while wrong time medication errors originated by the healthcare personnel were found occurred in 4 patients (overall 13 events) in the control group.
Hospital readmission over 60 days after discharge was lower in the study group compared with the control group. Lastly, the time nurses and pharmacists spent on medication management was reduced in the study group.
SAM substantially increased knowledge of medications, especially indication and side effects, that was unchanged in the control group throughout the study. Knowledge of dose, dosing frequency, and dosing time related to meals only slightly increased because they were relatively high at baseline, but all patients in the study group reached the maximum score (2 points for each aspect, except 1 patient did not get full score on the dosing time related to meals). This could partly be a result of incorporating the understandable symbols/images in the teaching materials or medication label. As most patients did not know Thai or English, the languages commonly used on the medication labels, symbols/images helped these patients pick up medication correctly. Thus, it could be seen that after being taught and counseled about medications by pharmacists using innovative symbols/images labels during hospitalization, the patients were more knowledgeable and able to take medication on their own more correctly as prescribed than they were with nurse-administered medication. At the time of knowledge assessment, although patients in both groups were allowed to use information labelled on the medication packages, patients in the study group should use the information more effectively as they were more familiar with the symbols/images than those in the control group. Knowledge on medication side effects in the SAM group that was less increased, compared with knowledge about medication indication at discharge might be related to inability to understand or remember medication side effect information or unable to distinguish side effects of individual drugs. Nevertheless, knowledge about common side effects the patients received from the intervention might help them manage their medications and improve medication adherence. However, SAM could not increase knowledge about medication names which was zero in both groups at baseline. This might be a result of patients' inability to read medication labels that were presented in English. Therefore, additional readable labels (in Thai or Malay) are suggested to increase patient knowledge of medication names. It was observed that the percentage of adherence was relatively high in both groups, lack of knowledge on medication name was unlikely to affect medication use, given that patients had knowledge about medication indication and dosage administration of individuals drugs. In the present study, patients in both groups were comparable in medication knowledge, and the numbers of drugs received prior to admission. Education level that might be associated with patient health literacy was used as a stratifying variable in the randomization process to generate the groups that were balanced in educational status (and health literacy). The greater in medication knowledge outcome in the study group should be the effect of SAM intervention. In a previous study involving 24 elderly in-patients, knowledge of medication name, dose, and dosing frequency slightly increased but significantly from 89.2% to 98.8% (p<0.001) at hospital discharge after using the SAM program.21 SAM program provided by registered nurses increased patient knowledge of their drug regimen, dosing time and side-effect.15 In addition, a systematic review reported consistent results that patients in the SAM group had higher knowledge about name, frequency, and dose of medications compared with nurse-administered medication group.8,16
Knowledge at the first follow-up visit after discharge from the hospital, an average of two weeks apart, remained the same in both groups compared with that at hospital discharge. In Thailand, patients are not registered to general practitioners (GPs), no appointments are made for patients to see GPs after discharge. The effect was therefore not influenced by GP visits. This effect was sustained at the second follow-up visit measured approximately 2 months after discharge. It was not surprising that knowledge on medication names was not improved as no additional readable labels were provided for patients after hospital discharge. A non-RCT reported the percentage of patients knowing about indication of drugs measured 10 days after hospital discharge was significantly higher in the SAM group (38/42, 90%) than that in the control group (17/37, 46%).22
In the present study, SAM program significantly increased patient adherence compared with nurse-administered medication measured at the first follow-up visit. This might be related to the knowledge received after SAM intervention, especially that regarding medication indication and side effects mentioned earlier. Knowledge about medication side effects that temporarily occurred and ceased over continuing use would enhance medication adherence. While patients in the control group were lack of awareness on medication indication and side effects that potentially affect the adherence and clinical consequences. Similar results were reported from a non-RCT that the SAM program provided by pharmacists significantly increased patient adherence to medications measured at 10 days after hospital discharge compared with nurse-administered medication group (95% vs 83%, respectively, percentage difference 12%, [95%CI 4%:21%], p<0.02).22 Increased patient compliance by the SAM program was confirmed by an RCT, although a qualitative systematic review revealed diverse results among included trials.19,23 However, results on compliance might be compromised in the validity as most of studies used pill count conducted by staff, very few used more reliable methods, such as urine tests or disguised observation. The present study also used pill count method, as no sensitive or specific methods were available in the study hospital. Medication adherence was retained at the second follow-up visit in both groups. The effects of SAM on adherence were expected to sustain over time.
The present study found a few administration errors in the control group (13 events out of 877 nurse-administered medication doses) and all were wrong time dosing (defined as the doses were not administered within 30 minutes of the scheduled time). Of these, 8 were clinical risk level C, and the remainders were clinical risk level D. Factors contributing to wrong-time administration errors were staff working overload, being interrupted by emergency care or nursing staff forgetting to provide medications to the patients. The 5 missed doses of antihypertensive agents occurred in 2 patients and subsequently resulted in uncontrolled blood pressure. However, the problems were not clinically significant, and were resolved after administration of the missed doses with closely monitoring. This study found no “wrong time” administration error in the study group, because nurses were notified by the patients if they did not arrive at patient' bed within 10 minutes. Grantham, et al. Also reported no patient-initiated administration errors among patients in the SAM group during the 6-month study period, compared with one medication error occurred in the previous six-month historical data.15Two administration errors during the study were due to nursing staff.15 A critical review confirmed that the proportion of medication errors in the SAM group was significantly lower when compared with healthcare personnel-administered medication group (0.045 versus 0.086, p<0.001).23 In addition, patients practicing SAM in hospitals had fewer medication errors and medication-related problems post discharge.5,24Medication errors attributable to patients receiving SAM program were less than that attributable to nursing staff, equipment defects, or pharmacists.15,24
In the present study, increasing patients' medication knowledge and adherence were in accordance with a reduction in hospital readmission among patients in the SAM group. Hospital readmission occurred earlier, a few days after hospital discharge, in the control group. The result was, however, observed in a relatively short follow-up period and the impact measured in a longer period is required. The results confirmed the reduction in hospital readmission after the SAM program reported previously.12
SAM substantially reduced nursing time and nurse workload on medication checking, distributing, and administering. The present study demonstrated that SAM level 2 reduced nursing staff workload and saved 1.8 hours for nurse to spend on medication management each day. Similarly, SAM decreased overall pharmacist workload and saved 0.9 hour per day. SAM intervention consequently provided sufficient resource available for SAM implementation. The time nurses required for checking whether medications delivered from the pharmacy department were consistent with that appeared in the doctor's order sheet was reduced in the study group. The medication checking process required every 4-day for patients in the SAM group and less time was required if any changes of the regimens were made during the 4-day course. While medication checking process for patients in the control group was repeatedly performed and consumed similar time each day. SAM implementation, however, increased workload of the ward pharmacists on educating patients about their medications, but it greater reduced the workload in the 4-day medication dispensing process and decreased overall pharmacist workload. In addition, as patients in the SAM group had already known their medications during admission, time spent on counseling and dispensing medications at discharge would be reduced or eliminated. The impact on pharmacist workload was consistent with that reported in a systematic review.19The benefits of SAM in reduction of workload and time spent on medication management should promote SAM implementation.
Although components or intensity of SAM program might be divided up to 9 levels, probably depending on the level of patient independence, responsibility, and the safety policies of the study hospitals, it is generally divided into 3 levels. Level 1, medication counseling and administration, is provided by a nurse (current usual practice in hospitals in Thailand); level 2, in-patient self-administered medications, is under the supervision of nurses or pharmacists; and in level 3, in-patients are totally responsible for their own medication administration.15,19,21 22-23 In this study, SAM level 1 (control group) which was a standard practice, was compared with SAM level 2 (study group) under supervision of the multidisciplinary team. Utilization of SAM should be individualized to match patients' ability to promote their responsibility, dependency, and convenience while patient safety is reserved or maximized.22 Presently, the study hospital provides medication labels presented in Thai (medication name, indication and dosing information); only the medication names are available in both Thai and English. Nonetheless, the pronunciation of the medication name was usually a technical term or generic name that was difficult for lay persons to remember. A supplementary label in Malay was provided for patients in the study who could read Malay, unfortunately very few were able to do so. The use of SAM level 2 for patients in the study group seemed to be appropriate and patient safety was reserved. Hospital safety policies stated in the latest revision of in Thailand Hospital Accreditation standards preclude the use of SAM level 3, as patient safety might be compromised. In a study that SAM was divided into 3 levels according to patient responsibility, only half of patients achieved the SAM level two or level three, mostly within 5 days of hospital admission. Achievement of SAM level might be limited by age (as patients in the study were relatively old, mean age 68.3 years), and limited literacy.15 Similar results were recently reported that four-stage SAM program improved rehabilitation patients' understanding and ability to self-managed medications in 14 out of 20 (70%) participants.25 SAM has been recommended worldwide to promote patients' abilities in self-managed medications.2 3 4-5 It has been implemented in acute hospitals in the United Kingdom and Belgium.7,26,27The Society of Hospital Pharmacists of Australia (SHPA) Committee of Specialty Practice in Rehabilitation and Aged Care has recommended SAM as a part of the discharge planning process in rehabilitation wards.28The program suggests that providing patients an opportunity to self-medicate in a supervised setting with education and support promotes patient confidence and competence in self-medication management at home after discharge.
Strengths and limitations
The strengths of this study were the use of randomized controlled blinded design, and all patients were completely followed-up. Stratified-blocked randomization gave nicely balanced (age, education level, and participant number) samples at baseline. In addition, other variables that might affect the outcomes, such as the present illness, comorbidities, number of prescribed medications, and visual or hearing capabilities were similar between groups. Blinding outcome assessors to treatment status helped prevent/minimize detection biases. Complete measurement of outcome data gave rise to valid results. Assessment of the outcome variables was done at hospital discharge and extended until all patients completed the first two follow-up visits, while a systematic review revealed that less than a half of included studies did.19 Furthermore, the benefits of SAM on improvement of medication knowledge and adherence was confirmed by a lower hospital readmission. Nevertheless, this study had some limitations. Firstly, most patients in the study hospital are unable to read Thai, and only some can speak or understand Thai language. Language barrier limited patient learning abilities in some areas, such as medication names and side effects, and thus the maximum effects of the intervention could not be reached. Therefore, additional educational materials understandable or readable for patients should be provided to maximize the intervention effects. Secondly, short-term follow-up at least confirmed the retention of intervention effects, but could not measure maximal long-term effects that should be achieved among those with chronic diseases. Thirdly, the present study did not assess satisfaction from either patient's or staff's perspectives, and financial costs, yet these data are important to be considered for implementation of SAM program. Further researches of good methodological quality are required to evaluate the effect of SAM schemes on a variety of patient, staff, setting, and clinical outcomes.
Implications
The results confirmed that SAM program among patients with chronic diseases increased medication knowledge, adherence and reduced administration errors. The effects of the SAM program on improvement of these surrogate outcomes were confirmed by a lower hospital readmission, which implicitly indicated a reduction in resource utilization. The study results were internally valid and consistent with those reported from studies different in methodologic aspects (patients, setting, SAM component, etc.).19,25The results, however, would be well generalizable to other settings with similar contexts. Generalizability of the results to other settings depends much on patient characteristics (competency and/or acuity), healthcare system, health personnel, and potential barriers. The treatment effects of a single staged SAM shown in the present study might be minimized in the setting of well literate or competent patients, as their baseline medication knowledge is expected to be adequate, unless the lacking knowledge area are identified and an appropriate intervention performed by a skillful personnel (educator) are provided to promote patients' success in self-managed medication. A recent study conducted out hospital in the US reported that QR code-based information (graphic and text) significantly increased patient safety of self-administered medications in both younger adults and the senior citizens compared with current bottle labelling, but the effect was greater in younger adults than the older.29The use of IT technologies, such as electronic health records, computerized order entry systems, bar-code medication administration systems, and electronic medication administration records effectively reduced medication errors, but not eliminated the potential for errors.30 In addition, IT systems provide accurate and standardized measuring, and reporting, application of IT in SAM implementation should enhance the success of the SAM program. SAM reduced nurse and pharmacist workload in the present study, but this effect may be attributable to many factors such as SAM components, roles and responsibilities delegated to individuals in the team, patient competence, as well as hospital environment. In Thailand, where resource constraints are the leading problems especially in healthcare services, wide implementation of SAM might reduce utilization of healthcare resources as a whole. However, patients' views or responsibilities, as well as hospital policies should be considered in planning and implementation of SAM program. Medication regimens should be simple and flexible enough to adapt to patients' lifestyles and usual routines. Nurses and or pharmacists should also take responsibilities to support and facilitate patient autonomy, to enable more effective management of health care needs when patients return home.31 Long term monitoring is suggested for evaluation and improvement of the SAM program. Further studies designed ad hoc are needed to confirm the effects of SAM on clinical outcomes such as long-term hospital readmission, resource utilization, ER visits, as well as drug-related problems.
CONCLUSIONS
In-hospital SAM education mainly performed by a pharmacist under a multidisciplinary team increased medication knowledge and adherence, and decreased medication errors among patients with chronic diseases. SAM extended the duration of out-patient status and decreased hospital readmission within 60 days after discharge, and reduced nurse and pharmacist time spent on medication management for in-patients. SAM contents and medication labels suitable with patient's learning ability were important components for the success of SAM program.