HEALTHCARE DELIVERY IN THE US
The United States (US) has a population of approximately 330 million people from diverse backgrounds and cultures.1 The US spends nearly 17% of its gross domestic product (GDP) on healthcare at over USD 10,000 per capita, which is twice the average compared to other developed countries.2 Yet, the US is among the worst performers compared to other developed countries in key health outcomes, including life expectancy at birth, infant mortality, safety during childbirth, and unmanaged chronic conditions like asthma and diabetes.
The US is one of the few developed countries without universal healthcare coverage; it does not have a single payer healthcare system or a national pharmaceutical benefits scheme/plan. The healthcare system includes a mix of public, private, nonprofit, and for-profit insurers, healthcare institutions and organizations, and providers. Modern healthcare coverage in the US began in the 1920s when hospitals offered pre-paid services to individuals, and a group of teachers in Dallas, Texas joined the first employer-sponsored hospitalization plan in 1929. During World War II, employer-sponsored health insurance became more popular in response to freezes on wage increases by the federal government. Employers could provide non-wage benefits (e.g., health insurance, sick leave) which were considered tax exempt, instead of increasing wages. Today, half of Americans receive health insurance coverage from their employer.3
The first major step toward government-sponsored healthcare coverage came with an amendment to the Social Security Act in 1965, which created Medicare and Medicaid and provides healthcare benefits to select groups of individuals. Medicare covers individuals age 65 years or older, those under age 65 who are disabled, and select disease states (e.g., end-stage renal disease), while Medicaid applies to eligible low-income individuals, pregnant women, children under 18 years of age, and those with disabilities. In 1997, federal legislation increased the number of children covered with the Children’s Health Insurance Programs, also administered via Medicaid. Importantly, each state is responsible for administering Medicaid programs and providing a safety net for those who do not qualify for Medicaid, and this state-level administration results in different coverage across states. Medicare Part D is the federal-government program initiated in 2006 that subsidizes the costs of prescription drug coverage to Medicare enrollees via contracts with numerous insurance companies (Part D sponsors), and it was enacted via the Medicare Prescription Drug, Improvement, and Modernization Act in 2003.4 While optional, all states currently provide coverage for outpatient prescription drugs to categorically eligible individuals, as well as most other enrollees.5
Yet, given the nearly 46.5 million individuals that remained uninsured in 2010, the Patient Protection and Affordable Care Act (ACA, also known as “Obama care”) was passed in 2010 and implemented in 2014 to expand healthcare coverage.6 The ACA created health insurance exchanges, or marketplaces, where low- and middle-income individuals could purchase their own insurance and receive government subsidies to offset the costs. States also received additional federal funding if they agreed to expand eligibility for Medicaid; however, not all states took advantage of this. Young people can also remain covered under their parent’s plan until age 26.7 Debate continues in the US regarding the role of government in providing healthcare insurance.
Demand on the US healthcare system has led to a significant expansion of jobs in healthcare. Between 2006 and 2016, jobs in healthcare settings increased by 20%, compared to only 3% job growth in the general economy.8 The job growth has been primarily in personal care aides, registered nurses, nursing assistants, and home health aides, likely due to the rapidly aging population in the US. Physician shortages, especially in primary care, are a key issue in the US with a projected shortage between 21,400 and 55,200 by 2033.9 In response, there has been a sharp increase in the number of nurse practitioners in the US, which are now approaching 300,000.10 Likewise, the number of physician assistants is increasing with expected job growth of 30% through 2028. With full prescribing privileges (unlike pharmacists), nurse practitioners and physician assistants are well positioned to fill gaps in the US primary care system.
The projected outlook for pharmacists in the US is widely debated. The optimistic outlook suggests that evolving practice roles for pharmacists will create new opportunities for employment in direct patient care roles. This is evident by the increased demand for specialty trained pharmacists to work in health systems and clinics.11 On the other hand, there is no doubt that the exponential growth in the number of graduating pharmacists provides increased supply and that overall demand for pharmacists is shrinking, especially in the traditional community pharmacy sector. This can largely be due to losses of revenue, attributable to decline in reimbursement for dispensing medications and lack of significant reimbursement for clinical services. The US Bureau of Labor Statistics projects 0% growth for pharmacists through the year 2028.12 The surplus of US pharmacists is largely related to the 38% increase in the number of pharmacy schools and 48% increase in the number of graduates over the past decade. It is possible, however, that this issue may correct itself as the mean number of applications per pharmacy school has declined over 50% in the past decade.13
Primary care in the US
Primary care in the US is delivered by three medical specialties: family medicine, general internal medicine, and general pediatrics. Additionally, other non-physician primary care providers (e.g., registered nurses, nurse practitioners, physician assistants, pharmacists) provide care alongside physicians.14,15 To further the objective of improving primary care, the American Academy of Family Physicians proposed the Health Care for All framework whose goal is to “ensure healthcare coverage for everyone in the United States through a foundation of comprehensive and longitudinal primary care”.16
Since the passage of the ACA, there has been a shift toward transforming primary care to provide patient-centered, coordinated, comprehensive care focused on providing proactive, rather than reactive, population health management. One such approach is the patient-centered medical home (PCMH) which facilitates partnerships between individual patients, their families, and their personal physicians.17 The main principles of the PCMH outlined by the Agency for Healthcare Research and Quality are that: 1) it provides comprehensive care by a multidisciplinary team being accountable for meeting physical and mental healthcare needs; 2) it is patient-centered, in that it considers the patients’ and their families’ unique needs, culture, values and preferences, and it promotes patients’ involvement in their care and disease management; 3) care is coordinated or integrated across specialty care, hospitals, home healthcare, and community services and supports, especially during transitions of care; 4) it offers accessible services wherein urgent needs are addressed, hours of operation are expanded, a member of the care team is available electronically or via the telephone, and there are alternative methods of communication such as email and telephone; 5) it is committed to quality and safety by engaging in performance measurement and continuous quality improvement, and adopting a population health management approach to care. In the PCMH model, payment recognizes patient-centered care management work beyond face-to-face visits, supports the use of health information technology for quality improvement, recognizes remote monitoring of clinical data using technology, allows additional payments for achieving quality improvement measures, and allows practices to share in savings generated from reduced hospitalizations.18
Another approach to improve primary care delivery is through accountable care organizations (ACOs), which are groups of providers who share the joint responsibility for the costs and quality of care provided to an assigned group of Medicare patients.19 In addition to receiving reimbursement based on the traditional fee-for-service model, ACOs are eligible to voluntarily participate in the Centers for Medicare & Medicaid Services (CMS) Shared Savings Program, a program that focuses on value and patient outcomes, rather than the number of encounters or procedures. As of January 1, 2020, there were 517 ACOs participating in the Shared Savings Program that provided care to 11.2 million (16.5%) Medicare beneficiaries.20
The PCMH and ACO are complementary approaches to reformed care delivery. Despite notable progress in the past years, not all primary care in the US is provided through PCMH and ACOs. There are still many independent primary care physician practices and large health systems that do not provide care by either of these models.
Finally, primary care is also provided in an array of other clinics focused on specific populations. Federally qualified health centers (FQHCs) are community-based health centers that provide primary care in underserved areas.21 The Indian Health Service provides care in federal facilities to American Indian and Alaska native peoples.22 As well, the VeteransHealth Administration serves about 9 million veterans yearly.23 Each of these systems is funded by the federal government. In addition, many communities also have free clinics that use volunteer/staff to provide healthcare services to disadvantaged individuals.24
In summary, primary care is provided in many different types of clinics and the providers are paid from numerous sources. Three medical specialties, advanced practice providers, and other clinicians support the delivery of primary care, and there is no single model of practice or reimbursement.
COMMUNITY PHARMACY IN THE US
Community pharmacy in the US is comprised of a number of sub-types of practice settings including independent, traditional chain, supermarket, and mass merchant pharmacies (Figure 1). The National Community Pharmacists Association (NCPA) reported that there were 61,800 community pharmacies in the US in 2018.25 Of the 314,300 pharmacists in the US in 2018, more than 135,000 (43%) worked as community pharmacists.26 Substantial differences in the number of pharmacies by county and region of the country have been identified with counties possessing the highest density of pharmacies per population having nearly three times as many pharmacies compared to those with the lowest density of pharmacies.27 Thus, where a patient lives in the US greatly impacts their access to community pharmacy services.

Figure 1. Sub-types of community pharmacies in the US and estimates for each type based on NCPA data25
Some pharmacies are able to generate revenue via clinical services (described below), but the primary business model for community pharmacies continues to focus on dispensing prescription medications to patients. In 2019, almost 3.8 billion prescriptions were filled in US pharmacies.28 While the majority (about 1.9 billion) were paid for by commercial insurers, which includes some government programs like the Children’s Health Insurance Program, Veterans Administration, and Indian Health Service, approximately 1.67 billion prescriptions were paid for, at least in part, by either Medicare or Medicaid, with patients being responsible for a co-payment.28 Payers’ coverage of prescriptions varies greatly across community pharmacy sub-type.25 In 2019, prescription dispensing revenues in the US reached a record USD 446 billion, with the top seven dispensing pharmacies (i.e., CVS Health, Walgreens Boots Alliance, Cigna, UnitedHealth Group, Walmart, Kroger, and Rite Aid) accounting for about 70% of the market.29 Detailed data from 2018 showed that independent pharmacies represented a USD 75.8 billion in prescription revenue, while CVS represented USD 102 billion, followed by the Walgreens Boots Alliance at USD 74.4 billion, Walmart at USD 20.9 billion, Kroger at USD 13.4 billion, and Costco at just USD 2.6 billion.30
In the US, medications are typically dispensed inside prescription vials or bottles that are filled at the pharmacy from bulk containers, rather than in individual blisters within boxes sold by the pharmaceutical industry, as is the case in Europe. Thus, the primary role of pharmacy technicians is to fill prescriptions and label medications in prescription bottles that the pharmacist then verifies. A growing body of literature supports expanding the role of technicians to administrative roles such as managing patient appointments, collecting comprehensive medication histories, and collecting clinical data to be reported to the pharmacist.31 The Pharmacy Technicians Certification Board provides national standards for technicians. Regulations and requirements for certification, registration, and licensure vary by state. To date, 24 states require pharmacy technicians to attain national certification, either as a requirement to be registered or licensed, or to perform certain duties.32
Policy considerations affecting community pharmacy in the US
One of the most significant barriers to advancing community pharmacy practice in the US is the current payment structure. When the Social Security Act was passed in 1965, pharmacists were omitted from the definition of healthcare providers, resulting in pharmacists not being able to be paid by the Federal government for most services under Medicare Part B (i.e., while Medicare Part A covers hospital care, Medicare Part B covers services provided by physicians and other providers in outpatient settings). Because other payers generally follow Medicare payment policies, there are limited opportunities for pharmacists to receive reimbursement from public, private or commercial payers. Being recognized by CMS as a provider would enable pharmacists to use existing fee-for-service health insurance billing codes when they provide non-dispensing services. Some exceptions exist for specific services provided to Medicare beneficiaries in Part D programs, such as medication therapy management (MTM) and immunizations.
Achieving this objective requires working with the federal government to develop and pass legislation to add pharmacists to its list of providers.33 To that end, 11 pharmacy organizations and other stakeholders are working together towards achieving provider status for pharmacists and studying possible options for legislative language that are primarily focused on amending the Social Security Act.34 Given the myriad pharmacy organizations in the US prioritizing their own agenda (e.g., American Pharmacists Association, American College of Clinical Pharmacy, American Society of Health-System Pharmacists, Academy of Managed Care Pharmacy, American Society of Consultant Pharmacists, among others), having a unified voice for the pharmacy profession is a challenge. The fact that 11 organizations have united efforts to advocate for provider status underscores the importance of such legislation for the profession.
Passing such federal legislation is likely to take considerable time, and several individual states (e.g., California, Washington) have passed provider status legislation for pharmacists, though they continue work on how these statutes will be implemented.35,36 Achieving provider status at the state-level, in theory, may allow pharmacists to negotiate reimbursement for services directly with insurance companies; however, payment may still not follow provider status recognition at the state level.
Community Pharmacy Enhanced Services Network
The Community Pharmacy Enhanced Services Network (CPESN) is a clinically integrated network of community pharmacies (mostly independent), that resulted from the expansion of the Community Care of North Carolina in 2014 with funding from a 3-year grant by the Centers for Medicare and Medicaid Innovation (CMMI). The goal was to provide a structure for community pharmacies to expand primary care efforts, as well as a means to negotiate reimbursement for services with payers as a group.37,38 This model has now spread to 44 states and includes 2,700 community pharmacies that offer enhanced services for high-risk patients. The core services that pharmacists are required to offer to be a part of the network include medication reconciliation, medication synchronization, immunizations, comprehensive medication reviews, face-to-face access to a pharmacist, and creating a comprehensive medication list. Additional enhanced services provided by select pharmacies comprise: 24-hour emergency services, collection of vital signs, home delivery/home visits, tobacco cessation program, durable medical equipment, point-of-care testing, long-acting injections, naloxone dispensing, nutritional counseling, and specialty medication compounding.39 To the best of our knowledge, no public information exists regarding the percentage of pharmacies providing each of the services and the reimbursement rates negotiated (if any) for each service across states. Several challenges were reported by pharmacists in the North Carolina CPESN offering medication management services related with initiating services, accessing internal and external information, documenting, among others. This same study found that 73 (59.3%) of the 123 participating pharmacies did not complete service requirements within the first 3 months.40
In 2019, the Community Pharmacy Foundation and CPESN partnered to fund the Flip the Pharmacy initiative which aims to transform community pharmacy practice, moving away from point-in-time and prescription-level to longitudinal and patient-level care processes and business models.41 Six transformation domains comprise the initiative, namely: leveraging the appointment-based model, improving patient follow-up and monitoring, developing new roles for non-pharmacist support staff, optimizing the utilization of technology and electronic care plans, establishing working relationships with other care team members, and developing the business model and expressing value.42 The initiative is currently underway, thus limited evidence regarding its impact on community pharmacy processes, volume and payment of services, or patient outcomesexists.43 The ultimate goal is togather evidence of the contribution of community pharmacists to improved patient care to serve as a means to negotiate reimbursement for pharmacist services with payers.
Pharmacy education and training in the US
Since 2000, the recognized professional degree that can be obtained from schools of pharmacy in the US is the Pharm.D. (doctoral degree). However, there remain a significant number of practicing pharmacists who were not trained at the doctoral level and have bachelor’s or master’s degrees.44 The 2016 American Council on Pharmaceutical Education’s set of educational standards were designed to ensure that all graduating pharmacists were prepared to contribute meaningfully to patient-centered care and interdisciplinary team practice, use evidence-based practice, apply quality improvement strategies, and utilize informatics.44 While community-based pharmacy residencies are not currently required, the number of such residencies has grown in the last 20 years to more than 130 accredited post-graduate year 1 (PGY1) programs.45 However, this growth has not kept pace with demand by student pharmacists or professional organizations such as the American College of Clinical Pharmacy, which previously advocated that starting in 2020 all pharmacists involved in direct patient care complete an accredited residency.45
Integration of community pharmacy and primary care
Pharmacists are integrated into primary care in a number of important ways, which continue to evolve over time. In support of better coordination between community pharmacy and primary care, the Centers for Diseases Control and Prevention (CDC) Division for Heart Disease and Stroke Prevention developed a practitioner and a pharmacist guide for “Creating Community-Clinical Linkages Between Community Pharmacists and Physicians” in collaboration with the American Pharmacists Association and the American Medical Association.46,47 Community-clinical linkages are defined as connections between the community, clinics, and other settings where primary care is provided to improve population health.46 The pharmacist guide provides a framework called LINKAGE outlining how community pharmacists and physicians can develop community-clinical linkages.47 Suggested activities to be performed by both parties as part of these linkages include: pharmacists conducting health assessments and referring patients to physicians for diagnosis or treatment; pharmacists triaging patients with medication-related problems or new/worsened health conditions into primary care; and physicians referring patients to pharmacists for medication and chronic conditions management.47
One way for community pharmacists to provide services and be reimbursed is by extending beyond the walls of the pharmacy and establish collaborations with primary care clinics. An example of such a model is pharmacists from an independent community pharmacy in the state of North Carolina providing services at an independent primary care clinic three days a week.48,49 Over and above improving patient outcomes, this service also gained the clinic an additional USD 16,920 in annual reimbursement.49 Pharmacists provide chronic care management services (i.e., services aiming to improve health outcomes by enhancing care coordination for patients with multiple chronic conditions) to Medicare beneficiaries, reimbursable since January 2015 via the Medicare fee-for-service program.50 The goal is to help the primary clinic achieve the quality measures set by CMS, while also arranging a way for both parties (physician and pharmacists) to be reimbursed, even if billing is under the physician’s fee schedule. This model is by no means widespread in the US and requires collaboration with a provider.50
Primary care is also moving inside pharmacies. Several community pharmacy chains and mass merchants have opened walk-in clinics inside their stores as a means to increase access to care. For example, CVS has co-located Minute Clinics that provide walk-in care for minor illnesses, minor injuries, skin conditions, travel health, vaccinations and injections, wellness and physicals, women’s services, and screenings and monitoring. Cost of services can be covered by insurance plans or paid out-of-pocket. Treatment for minor illnesses, minor injuries, skin conditions, wellness and physicals, and screenings and monitoring cost between USD 99-139/visit; cost for travel health related items ranges between USD 59-142; women’s services cost between USD 59-250; and vaccinations and injection administration between USD 50-250.51 Care is provided by nurse practitioners and physician assistants (not pharmacists) to both adults and children.52,53 The CEO of CVS Health has publicly stated that “retailization of healthcare” will continue to evolve, with service convenience being a top priority.54 Walgreens had a similar arrangement up until 2019, but decided to outsource the service to VillageMD, a group of primary care physicians, in July 2020. They plan to open 500-700 “Village Medical at Walgreens” physician-led primary care clinics in more than 30 US markets in the next five years. The press release mentions that pharmacists will be integrated as a critical member of the VillageMD’s multi-disciplinary team, but no further details are provided.55
Pharmacist prescriptive authority
In the US, pharmacists who are able to prescribe, monitor, and adjust medications independent of or in collaboration with physicians can generally provide associated clinical services. The National Alliance of State Pharmacy Associations (NASPA) is a trade association that tracks pharmacy legislation and regulations across all 50 states and the District of Columbia.56 NASPA and the Idaho State Board of Pharmacy proposed a framework to characterize existing models of pharmacist prescriptive authority along a continuum from most restrictive to least restrictive (Figure 2).57 At present, 49 states and the District of Columbia have passed legislation that allows pharmacists to prescribe medications under CPAs, standing orders, or statewide protocols.
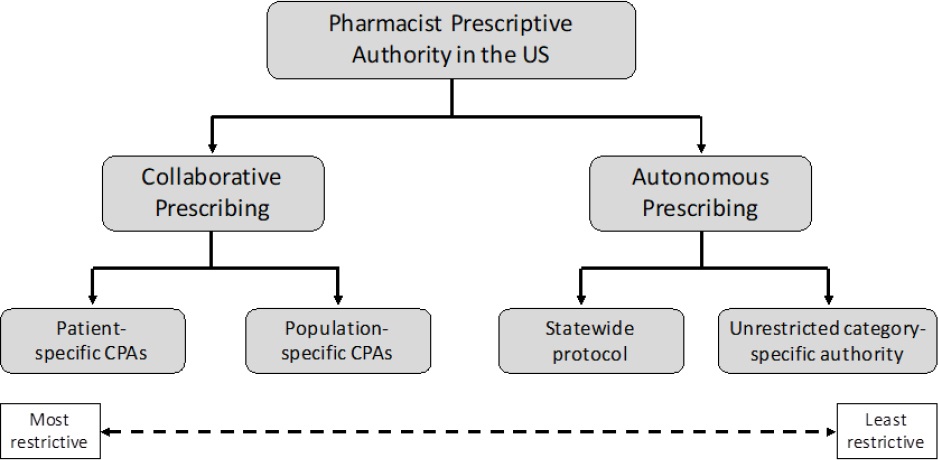
Figure 2. Summary of available practice models adopted by states that allow pharmacists to prescribe in the United States (CPAs, collaborative practice agreements)
(CPAs, collaborative practice agreements)
In a collaborative prescribing model, pharmacists and prescribers create formal relationships through the establishment of collaborative practice agreements (CPAs) wherein the latter grant prescriptive authority to the former.58,59 CPAs can be patient-specific (i.e., individual patients or a collaborating prescriber’s patient panel) or population-specific (i.e., categories of patients). While population-specific CPAs are commonly used for acute care (e.g., treatment of influenza in patients with certain characteristics that do not meet criteria for automatic referral), both patient- and population-specific CPAs are established for chronic disease management (e.g., diabetes, hypertension, hyperlipidemia, asthma).57
Autonomous prescribing can occur via statewide protocols or unrestricted category-specific prescribing. In these situations, CPAs are not required to be in place for pharmacists to prescribe; however, pharmacists are still responsible for coordinating care with the primary care provider. Statewide protocols are set by an authorized body or state government (e.g., Board of Pharmacy, Department of Health) and allow pharmacists to prescribe medications that are intended for preventive care or for acute or self-limiting conditions that require a limited process to diagnosis. The scope of statewide protocols isgenerally narrow and often arises in response to a public health crisis. Any pharmacist who fulfills the requirements specified in the protocol is authorized to prescribe without supervision from a collaborating physician, unlike CPAs.57 Unrestricted category-specific prescribing applies to a limited range of medications for which no specific diagnosis is needed. Instead of following a state-derived protocol, states refer pharmacists to other authority documents, such as practice guidelines, to guide prescribing. Autonomous and collaborative prescribing supplement each other, rather than being mutually exclusive.57
A standing order is a statewide prescription issued by a state designated prescriber under which pharmacists are allowed to fill a prescription to dispense a product (e.g., naloxone, smoking cessation products). In this model, pharmacists are not the prescribers.
Community pharmacy services
As described above, pharmacy practice legislation varies across all 50 states and the District of Columbia. Likewise, reimbursement for specific services also differs at the state level, unless reimbursement is based on federal legislation, as is the case of services for Medicare beneficiaries. In the US, there is a history of pharmacy services innovations, but state fragmentation and the lack of a single payer system and a single vision and voice for the pharmacy profession prevent scaling these innovations at the national level. Chain pharmacies play a pivotal role in scaling service innovation in community pharmacy beyond dispensing services through counseling, MTM services, and several disease state management initiatives.60,61 Due to their dissemination across the country, scale up of services is maximized. For example, reports demonstrate chain pharmacies positioning themselves to meet demand for convenience in offering immunization services.62 However, work in a busy chain pharmacy can lead to pharmacist burn out, which in turn compromises patient safety.63,64
The services described below represent the mainstream services that pharmacists currently provide and, in particular circumstances, for which they can obtain reimbursement (Table 1). Due in part to the fragmented nature of the healthcare system in the US, it is not currently possible to report the extent to which these services are provided. Existing evidence usually derives from research studies that academics conduct with data obtained from either local Boards of Pharmacy or state-wide surveys, the latter usually limited by a low response rate. More recent reports of MTM have used Medicare Part D claims to examine some services.
Table 1. Pharmacist services available in the community pharmacy setting
| Service/Activity | Availability status (date) | Regulation level | Reimbursement |
|---|---|---|---|
| Immunizations | • All 50 states and the District of Columbia (Jun. 2020) • 1 state (Alabama) only by prescription (Jun. 2020) • 6 states allow pharmacy technicians with required training to administer vaccines under the supervision of a certified pharmacist (Jun. 2020) |
State | • Via contract with the appropriate payers (i.e., pharmacy benefits managers, Medicare, Medicaid, third-party medical plans) • Bill payers for both the vaccine and administration service (varies between USD 15 - 40) or paid by patients out-of-pocket |
| Medication Therapy Management (MTM) program | • All 649 Medicare Part D contracts use pharmacists to provide MTM (2019) | Federal | • Reimbursement provided by CMS • Billing in 15-minute increments using current procedural technology codes |
| Medication packaging | • Implementation status unknown | N/A | • Paid by customers out-of-pocket or offered as part of a medication synchronization program |
| Medication synchronization | • 22,000 community pharmacies (2015) | N/A | • No reimbursement. MTM billing codes apply if offered as part of the service |
| Hormonal contraception prescribing | • 9 states and the District of Columbia (Dec. 2019) | State | • Reimbursement varies by state |
| Point-of-care (POC) testing | • All 50 states and the District of Columbia - for approved tests with pharmacy CLIA waiver from CMS (1988) | Federal | • Paid by customers out-of-pocket |
| Naloxone prescribing or dispensing | • All 50 states and the District of Columbia (Jan. 2019) ○ 17 states and the District of Columbia - statewide protocol/pharmacist prescribing (Jan. 2019) ○ 12 states - statewide standing order (Jan. 2019) ○ 4 states - dispense without a prescription (Jan. 2019) ○ 17 states - standing order (Jan. 2019) |
State | • Variable out-of-pocket costs depending on the patient’s health insurance • Pharmacist counseling not reimbursable |
| Tobacco cessation aid prescribing | • 37 states (Nov. 2019) ○12 states - statutes or regulations allowing pharmacists to prescribe (Nov. 2019) ○ 17 states - prescribe under population-based CPAs (Nov. 2019) ○ 7 states - prescribe via autonomous prescribing (Nov. 2019) ○ 1 state - independent prescribing (Nov. 2019) |
State | • Reimbursement varies by state |
Immunizations
All 50 states and the District of Columbia have legislation allowing pharmacists (and student pharmacist interns operating under the supervision of the pharmacist) to administer immunizations. States allow vaccine administration via any of the prescribing mechanisms described above, except one (Alabama) which only allows vaccine administration by prescription. The types of vaccines that pharmacists can administer and the minimum age of patients to whom they are allowed to administer also vary across states. While some allow any vaccine to be administered to any patient regardless of age, others do not allow pharmacists to administer certain vaccines (e.g., human papillomavirus vaccine) or restrict administration to adults or children older than a certain age.65 Immunization administration in some states also extends to CDC-recommended travel vaccinations. As of June 2020, six states allowed pharmacy technicians who completed immunization certificate training to administer vaccines under the direct supervision of a certified pharmacist.65
The 2019 National Pharmacist Workforce Study reported that 90% of community pharmacists administered vaccines.66 In Westrick et al.’s study of a nationally representative sample of 292 community pharmacies, 80% reported that they had provided immunization services in 2016, the most common vaccines being influenza, herpes zoster, pneumococcal 13-valent conjugate (PCV13) and pneumococcal polysaccharide (PPSV23).67 Pharmacy-based immunization services have been associated with an increase in the likelihood of being immunized.68 As an example, influenza vaccinations dispensed in community pharmacies increased from 3.2 to 20.9 million between 2007 and 2013.69
In order to bill for immunization administration, pharmacies need to contract with the appropriate payers (i.e., pharmacy benefits managers, Medicare, Medicaid, third-party medical plans). Pharmacies bill for both the product and the administration service. Administration fees vary between USD 15 and USD 40.70 Additionally, pharmacies can charge customers or private employers with whom they contract directly. The average direct costs paid per adult vaccination were shown to be lower in pharmacies compared with other medical settings, likely because in medical settings additional billing codes can be applied (e.g., billing codes covering patient counseling).71
Medication therapy management
MTM is a service included in Medicare Part D plans that aims at improving medication use and reducing the risk of adverse events in eligible Medicare beneficiaries.72 MTM includes five core elements: 1) comprehensive medication review (CMR); 2) provision of a personal medication record; 3) construction of a medication-related action plan consisting of a list of actions for patients to track progress for self-management; 4) intervention to address medication-related problems or referral to a physician or other healthcare professional; and 5) documentation of MTM services and follow-up visit.73,74 Part D plans are required to provide and automatically enroll in their MTM programs beneficiaries who meet pre-specified CMS criteria, namely: having multiple chronic diseases, taking multiple Part D medications, and being likely to incur annual Part D medication costs that meet or exceed a certain threshold every year (e.g., USD 4,044 in 2019).75 However, 27% of MTM programs in 2019 used expanded eligibility requirements beyond the minimum required by CMS.76 MTM services may be provided by pharmacists or other healthcare professionals. For example, of the 649 Part D contracts with an approved MTM program in 2019, 100% used pharmacists to provide MTM services, 74% used a registered nurse, 24.5% a physician, and 15.1% a physician assistant (multiple selections were allowed, thus categories were not mutually exclusive). Beneficiary enrollment into MTM programs should be at least quarterly (47.1% of plans in 2019), but could also be every other month, monthly, weekly or daily. Eligible beneficiaries are mainly identified via medication claims data.76
The CMR is a core element of MTM and it consists of an “an interactive person-to-person or telehealth medication review and consultation conducted in real-time between the patient or other authorized individual, such as prescriber or caregiver, and the pharmacist or other qualified provider and is designed to improve patients’ knowledge of their prescriptions, over-the-counter (OTC) medications, herbal therapies and dietary supplements, identify and address problems or concerns that patients may have, and empower patients to self-manage their medications and their health conditions”. Part D sponsors are required to provide a CMR at least annually or targeted medication reviews (TMR) quarterly. TMRs are shorter duration medication reviews to assess medication use, monitor unresolved issues, identify new drug therapy problems, and assess whether beneficiaries experienced a transition of care. CMR delivery method can be face-to-face, over the phone or through telehealth.76 The benefits from obtaining a CMR include the identification of effectiveness and safety issues with prescribed medications, as well as identification of less expensive alternative medications for patients.77 Despite the benefits of CMRs, the uptake of the service is low - less than 20% of eligible Medicare beneficiaries in 2013 and 2014 received the service -, either because patients are unaware of it or because they perceive it as unnecessary.77 78-79 Data from the 2019 National Pharmacist Workforce Study indicated that 66.7% of respondents provided MTM services.66 Additionally, analyses of Medicare claims data from 2014 revealed that community pharmacies provided only 22% of the CMRs, with the remainder provided by either other types of pharmacists or other professionals.80 In 2018, the CDC launched a statewide initiative focused on implementing and evaluating evidence-based strategies to manage diabetes and prevent or delay onset of type 2 diabetes in high-burden populations and communities, and one of the strategies proposed is to expand MTM services provided by pharmacists to patients with diabetes.81
The effectiveness of MTM services remains a contested topic because of heterogeneity of previous studies’ populations, settings, and outcomes.82 In addition, contemporary MTM definitions found in the professional literature differed from the early definition in the regulatory reference, making meaningful evaluations over time difficult.83
Reimbursement to pharmacists (and other professionals) rendering MTM services is provided by CMS. Billing is in 15-minute increments using current procedural technology codes (specific codes used for medical billing). The initial 15-min face-to-face assessment is reimbursed at a rate of USD 50 and is covered once a year per provider per beneficiary. Follow-up assessments of 15-minute increments are reimbursed at a rate of USD 25 and providers can bill up to seven times in a year. Additional 15-minute increments to the two previous codes can be billed up to four times per provider per beneficiary per date of service at a rate of USD 10.84 Lack of standardization for documentation and billing is an important limiting factor of MTM programs.85 Another potentially contested aspect is the effectiveness of a CMR without access to the electronic health record (EHR).
Medication adherence
Similar to other countries, community pharmacists in the US offer services aimed at improving medication adherence.86,87
Medication packaging is one such service. Packaging interventions significantly improved medication adherence in a meta-analysis of 52 studies.88 This study demonstrated that interventions using blister packs compared with pill boxes, and delivered in pharmacies compared to interventions delivered elsewhere were significantly more effective at improving adherence.88 It is unclear what percentage of community pharmacies in the US offer medication packaging services. The service is not reimbursed by CMS or prescription insurance plans. While some pharmacies may offer the service as part of their medication synchronization service, others may charge an out-of-pocket fee to customers.
Medication synchronization is a process by which a patient’s medications refill dates are aligned so that patients only come to the pharmacy once a month. Prior to preparing the medication, pharmacy staff call patients to identify whether any changes to medications occurred and to confirm what medications should be dispensed. This contributes to a higher efficiency of the pharmacy workflow, in addition to presenting an opportunity for pharmacists to perform a medication review and identify any therapeutic or compliance issues.89 As of 2015, this service was being offered by more than 20,000 chain and 2,000 independent community pharmacies across the country and 66.5% of participants in the National Pharmacist Workforce Study reported that they offered the service.66,90 However, service provision varies across pharmacies - while some focus exclusively on the alignment of refill dates, others conduct an appointment-based medication synchronization where patients meet with the pharmacist to discuss their medications, any adherence issues, or receive MTM services.91,92 Unfortunately, the extent to which each modality occurs is unknown and even if it were self-reported, it is legitimate to expect response bias. The service itself is not reimbursable but it may contribute to increased monthly prescription volume.93 Additionally, if MTM services are provided with medication synchronization, the pharmacy receives reimbursement via the MTM billing mechanisms. Retrospective analyses of the service showed that appointment-based medication synchronization increased the odds of being adherent by 2 to 6 times compared to patients not enrolled in the service.94 95-96 Patients in a synchronization program also presented rates of hospitalization and emergency department visits and rates of outpatient visits that were 9 and 3 percent lower, compared to a control group obtained via propensity score matching.94 However, it is unclear which components of the service contribute to these improvements due to the lack of a consensus definition of medication synchronization.92
Hormonal contraception
As of December 2019, nine states and the District of Columbia had statewide authority for autonomous pharmacist contraception prescribing.97 Each statewide authority has different prescribing protocols, patient age limitations, contraceptive formulations allowed (e.g., oral, patch), and pharmacist training requirements.97 Many included a patient self-screening assessment, blood pressure measurement, documentation requirements, and patient education materials in the prescribing procedure.97 Reimbursement exists on a state-by-state basis. For example, in the state of Oregon, certified pharmacists prescribe hormonal contraception and are reimbursed by Medicaid and private payers at the same rate as physicians and nurse practitioners for both the product and the assessment.98 Since April 2019, California’s State Medicaid program (Medi-Cal) reimburses pharmacist services furnishing hormonal contraception at a rate of 85% of the fee schedule for physician services.99 A time and motion study conducted in community pharmacies in the state of Oregon found that pharmacists spent approximately 18 minutes to screen a patient for eligibility, document the encounter, and provide a written prescription for contraceptives in an uncomplicated patient.100 A descriptive study of 391 supermarket-based pharmacies in California and Oregon revealed that 1970 service visits resulted in birth control prescriptions by 381 pharmacists, 95.7% of which were for the pill, 2.1% for the vaginal ring, 1.6% for a transdermal patch and 0.1% for an injectable.101 In other studies, pharmacists described time constraints, lack of access to EHRs, lack of reimbursement, additional training needs, and liability concerns as potential barriers to prescribing contraception.102 103-104 State practice laws, workflow design, and perceived barriers by pharmacists will need to be addressed to fully expand patient access to pharmacist-prescribed hormonal contraception.
Point-of-care testing
Point-of-care (POC) testing, such as blood glucose, hemoglobin A1c, cholesterol and international normalized ratio testing are some of the available community pharmacist-provided services and may be included under a CPA. In order to perform POC tests, pharmacies must obtain a certificate of waiver from CMS to perform a Clinical Laboratory Improvement Amendment (CLIA)-waived test.105 A CLIA-waived test is designed for screening, monitoring, or diagnosis outside of a laboratory setting and are used within a community pharmacy setting.106
In recent years, POC testing has expanded beyond glucose and cholesterol (Table 2). Community pharmacists providing POC testing for group A streptococcus and influenza under a CPA increased access by administering POC tests outside of normal clinic hours, conducting tests in patients without a primary care provider, and providing appropriate medication based on test results.107 108-109 Similarly, POC testing for human immunodeficiency virus and hepatitis C was provided by trained community pharmacists.110 111-112 The availability of these tests is not widespread and patient awareness, willingness to receive, and payment mechanisms for community-based POC infectious disease testing remain a concern.113 While POC testing may be an important means to screen patients and provide care, the business model for it must be developed.
Table 2. Point-of-care tests available in community pharmacy in the United States*
| Blood glucose Cholesterol Group A Streptococcus Helicobacter pylori Hemoglobin A1c Hepatitis C Virus Human Immunodeficiency Virus Influenza International normalized Ratio Pharmacogenetics |
*Note that this is not a complete list of all possible tests.
Adapted from information provided by NCPA105 and previous literature.114, 115
Opioid reversal agents
In response to the opioid epidemic in the US, efforts to increase access to naloxone in community pharmacies have been widespread. Each state and the District of Columbia has varying levels of how pharmacists may prescribe or dispense naloxone, ranging from a statewide protocol, including pharmacist prescribing authority, to the ability to dispense without a prescription.116,117 In the 2019 National Pharmacist Workforce Study, 72.2% participants reported dispensing naloxone.66 Despite 57% pharmacists working in community settings feeling confident recommending naloxone, only 28.3% felt confident administering it.66 A greater proportion of mass merchandiser (76.6%) and large chain (63.3%) pharmacies dispense naloxone via a standing order compared to independent and small chain pharmacies. The latter dispense naloxone more frequently based on a prescription order (44.4% each).66
An analysis of community pharmacy records revealed that naloxone dispensing increased from 1,282 prescriptions (0.4 per 100,000) in 2012 to 556,847 (170.2 per 100,000) in 2018. Individuals with commercial insurance represented the largest percentage of dispensed naloxone prescriptions in 2018 (51.1%), followed by Medicare (35.9%), Medicaid (10.7%), and self-pay (2.4%). A majority (42.3%) of prescriptions did not require out-of-pocket costs, while 24.5% required out-of-pocket costs of less than USD 10.00, 21.9% between USD 10.01-50.00, and 5.8% over USD 50.00. Counties with high naloxone-dispensing also had more high-dose opioid dispensing rates, higher drug overdose deaths rates, higher potential buprenorphine treatment capacity, and higher rates of Medicaid enrollment. Micropolitan and rural counties were less likely to be a high naloxone-dispensing county compared to metropolitan ones. However, in this study, pharmacists were grouped under “other” specialty prescribers, thus limiting the ability to determine the amount of pharmacist-provided naloxone.118 Differences in state practice laws, required pharmacist training, pharmacist time, pharmacist confidence in naloxone prescribing, inadequate pharmacist reimbursement, and patient out-of-pocket costs present current challenges to widespread adoption of naloxone dispensing.119,120
Smoking cessation
Prescription of tobacco cessation therapy can be achieved through the establishment of population-based CPAs, standing orders, statewide protocols, or independent prescribing. In the latter two cases, pharmacists not only prescribe but are also able to bill the patient’s insurance for any covered smoking cessation services in addition to the prescription medication dispensed (reimbursement variable).121 For example, in California, the Medicaid program (Medi-Cal) covers smoking cessation services at 85% of the physician’s fee.99 The products covered under statewide protocols vary across states, with some including varenicline and bupropion, in addition to non-prescription and prescription nicotine replacement therapy products. Pharmacists must meet minimum education requirements to engage in autonomous prescribing of tobacco cessation products.122 Provision of this service is sporadic, despite legislation being passed in many states.
FUTURE DIRECTIONS IN COMMUNITY PHARMACY IN THE US
Community pharmacy practice in the US contains multiple stakeholders whose interests often compete. To discuss the future of community pharmacy in the US we will use Donabedian’s structure, process, outcomes framework.123
Structure
One of the most significant barriers is the current payment structure and pharmacists not being recognized as providers by CMS, as discussed above. While achieving provider status is an important step for the profession to bill under fee-for-service, it is also important to acknowledge a growing shift from this model to pay-for-performance healthcare reimbursement. Similar to other jurisdictions around the world, the US is facing precipitous increases in healthcare costs. One method for beginning to address these increases is shifting incentive structures away from the quantity of services provided to one focused on the quality of services provided. Quality measures have been proposed and adopted at multiple levels of the healthcare system including hospitals, physicians, nursing homes and health plans, to drive improvement, inform consumers, and determine payment. Of particular relevance to community pharmacy is the Medicare Star Ratings program which evaluates the quality of Medicare prescription drug plans on a 5-star system where higher is better.124 There are currently five active medication-related measures, which have been developed in collaboration with the Pharmacy Quality Alliance, whose mission is to optimize health by advancing quality medication use.125 The five measures are: 1) medication adherence (via calculation of the proportion of days covered) for 1a) diabetes, 1b) hypertension, and 1c) cholesterol medications; 2) CMR completion rate as part of the MTM program; and 3) statin use in persons with diabetes.126,127 Though not specific to community pharmacy, community pharmacists have the potential to impact all these measures through many of the services outlined previously. Importantly, health plans in select states have started paying bonuses to high performing pharmacies (i.e., those who positively impact medication-related quality measures) and including them in preferred pharmacy networks, meaning that patients who utilize these pharmacies will have reduced or no co-pays for their prescriptions.128 Although value-based reimbursement continues to evolve, it does present community pharmacy with a unique opportunity to build a new community pharmacy practice model.
Another significant barrier, but also a potential opportunity, comes from needed improvements in access to technologies such as EHRs, use of mobile health applications, and telemonitoring.129,130 Success in accessing patients’ EHRs from a community pharmacy setting to help coordinate care and communicate with other providers is achievable, though would require collaborations across multiple health systems and EHRs.131 Access to EHRs helps community pharmacists gain access to the current medication list, doses, and laboratory results to monitor medication effectiveness and disease control or progression.132 The use of mobile health apps for sharing of health information between the community pharmacy, the patient, and other healthcare providers is growing. For instance, the MEDIvate iOS smartphone application using cloud architecture allows patients to scan a vaccine prescription QR code to import their vaccine data and vaccine information into the app.133
Failing to adequately address these barriers will leave community pharmacy open to a substantial threat from disruptors such as Amazon. In addition to its recent acquisition of the online pharmacy PillPack, Amazon’s operations are specifically designed for efficiency, have extensive transportation networks, and can leverage the presence of Whole Foods (a groceries store) to provide great customer experience.134,135 Amazon can offer substantial discounts to cash-paying customers because of its size and will present a viable alternative to the employers searching for pharmacy benefit plans for their employees.134 Finally, it is also nearly prepared to meet the needs of the Drug Supply Chain Security Act, which will come into effect in 2023, that requires that all prescription medications be traceable from manufacturer to patient.134
Process
The success of structural adaptations will only be achieved if corresponding adjustments are made to processes taking place within the community pharmacy. To begin, all technical duties should be transitioned to pharmacy technicians. There is growing evidence supporting technicians’ participation in MTM sessions, serving as pharmacist extenders, and completing tech-check-tech dispensing.136,137 Some states have passed legislation allowing technicians to provide some immunizations.138 Before these tasks can be given entirely to technicians, the laws governing technician practice across the country must be standardized to ensure adequate levels of training and competency.137
The COVID-19 pandemic has also further accelerated the process of giving and receiving care via telehealth.139 This represents an opportunity for community pharmacy to transition some services to this delivery format to save patients time and pharmacy resources. For example, it could be a means to standardize the provision and increase uptake of MTM among Medicare Part D plan beneficiaries.
As technicians release pharmacists’ time for clinical duties and new opportunities for the provision of care via telehealth are adopted, the profession should acknowledge and lessen the impact of “community pharmacy practice inertia”, characterized by a reliance on outdated protocols and practices in the face of new evidence.140 Despite various legislative advances, uptake of community pharmacist services is generally low across states, speaking further to the need to address both structure and process aspects.
Outcome
Once structure and process adjustments have been made, community pharmacists can focus on service expansion and clinical, humanistic and economic outcomes. A common criticism to the pharmacy practice literature relates to the poor and inconsistent intervention reporting.141 142 143-144 As mentioned above, a challenge with MTM and medication synchronization is the lack of standardized definitions and process of how these services are provided across multiple studies.82,83,92 In order for services to be integrated in routine community pharmacy practice and sustained over time, it will be helpful to draw from the implementation science discipline. Implementation science focuses on methods to “promote the systematic uptake of research findings and other evidence-based practices into routine practice”.145 Implementation science emphasizes systematic thinking about healthcare delivery and has developed numerous frameworks for, not only rethinking practice change implementation, but also for guiding ongoing data collection and monitoring.146 These data will be as equally important as patient outcomes as current and future practice scope expansion legislation is passed.
CONCLUSION
Community pharmacy is the US offers some clinical services to support primary care, but the business model retains a focus on dispensing. Chain pharmacies (and potentially pharmacies within CPESN) offer important opportunities to scale clinical services nationwide. Yet, the delivery of medications to homes via incredibly efficient modes - whether Amazon or automated transportation - offers significant opportunity beyond dispensing for helping healthcare providers and patients obtain the best outcomes from medications. When we overcome structural barriers to care such as limited reimbursement and lack of coordination with the EHR, then community pharmacists will be able to adapt their processes of care to achieve improved patient outcomes.














