INTRODUCTION
Cough, a respiratory reflex to clear the upper airways, is a common condition that affects people worldwide.1-3 Based on the duration, cough can be categorised as acute, sub-acute and chronic.4 Acute cough is defined as having a duration of less than three weeks and is commonly caused by upper respiratory tract infections and acute bronchitis.4,5 Sub-acute cough usually lasts between three to eight weeks and is most commonly due to post infectious cough or exacerbation of underlying disease, such as upper airways cough syndrome (UACS), asthma and other pulmonary diseases.4 Meanwhile, chronic cough is defined as cough lasting longer than eight weeks and can be attributed to bacterial infection such as Mycobacterium tuberculosis infections, environmental exposure such as tobacco smoke and air pollutants, adverse drug reactions to certain medications such as Angiotensin Converting Enzyme (ACE) inhibitors or Angiotensin Receptor Blockers (ARBs), and underlying medical conditions, including asthma and other pulmonary diseases, gastro-oesophageal reflux disease, upper airway cough syndrome, and cardiac origins.4,6
Many patients with cough often self-medicate to alleviate their symptoms, with community pharmacies as well-known sources for medicine supply that are accessible to most patients.7-10 Self-medication in this paper refers to the use of medicines by people on their own initiative, without prescription by a medical doctor.11,12 Surveys have shown that cough medicines are one of the highest selling over the counter (OTC) product categories in community pharmacies in many countries.13,14 This situation emphasises the importance of the role of community pharmacists.9 They are health care professionals who are well positioned in the community to provide professional advice for patients with cough.
In general, the provision of pharmaceutical consultation in community pharmacies include two important steps, which are: patient assessment and the provision of advice.15-17 During patient assessment, pharmacists should gather relevant information, such as information on patient identity, symptoms (such as nature and duration of the symptoms, accompanying symptoms, etc.), action that has been taken to alleviate the symptoms, medical conditions, current medications used, and allergies.18 Then, pharmacists need to use their knowledge to analyse the information gathered to decide what best advice that can be provided to patients. This could be medical referral, recommended products along with the product information, provided non-pharmacological advice, or other advice that are relevant to patient symptoms.17,19
Internationally, the provision of pharmaceutical consultations for patients with cough in community pharmacies is suboptimal, including Indonesia.20-22 There are deficiencies in many aspects of pharmaceutical counselling for cough, including lack of history taking and inappropriate advice provision.20-22 In developing countries, studies have identified several factors contributing to these deficiencies.23-25 In Indonesia, previous research has identified three main factors influencing pharmaceutical consultation performance: pharmacy staff-patient interaction, the organisational context of the pharmacy, and the external pharmacy environment (Figure 1).23 These factors are complex and inter-related; for example the lack of knowledge and competency of pharmacy staff to provide quality consultation are influenced by deficiencies in pharmacy education with respect to management and pharmaceutical consultation for self-medication.23 Indonesian pharmacists also perceive that there is a problem with relevancy between what is taught in their pharmacy education and the knowledge required for practice, and therefore they felt that their knowledge is insufficient to provide optimal self-medication services.23,26 Similar findings have been reported in the literature from other developing countries, such as Brazil and Vietnam.24,27

Figure 1. Factors related to the provision of self-medication consultation in community pharmacies in eastern Indonesia from Brata et al.23
In Indonesia, to become a pharmacist, students are required to complete a four-year Bachelor of Pharmacy (BPharm) degree, followed by a one-year pre-registration training programme (Apothecary programme). Pharmacy curricula are regulated by the Ministry of Education and are typically based on the curriculum developed by the Indonesian Association of Higher Education of Pharmacy (Assosiasi Perguruan Tinggi Farmasi Indonesia, or APTFI).28 While each pharmacy school has the freedom to design their own curriculum, APTFI suggests that the courses or units of study within the BPharm curriculum are designed to be predominantly theory based, with the addition of laboratory practice or simulation, whereas the apothecary program focuses on applied pharmacy practice.28
The quality of Indonesian pharmacy education varies widely across institutions.28 Therefore, from 2018 onwards, students in the apothecary programme are required to pass a national, computer-based test (CBT) examination before they can be registered as pharmacists.29 In addition, students also need to take an objective structured clinical examination (OSCE) as a formative assessment.29 The OSCE is intended to become a summative barrier examination; however, the transition is currently postponed as a result of the COVID pandemic.
Studies looking at the situation of Indonesian pharmacy education are limited. A study conducted at the University of Gadjah Mada, has evaluated their 422 apothecary students' performance using an OSCE.30 The authors reported that approximately 85% of the 422 students were able to pass the minor ailment station.30 However, the study aim was to measure students' experience and perception of the OSCE and not to measure the competence of students in responding to patients with minor illness.
This study is conducted to measure the competency of Indonesian pharmacy students in providing self-medication consultations for patients with a cough. In this study, the competency of pharmacy students in providing self-medication consultation is defined as a combination of students asking/gathering essential information such as information related to patient identity, symptoms (nature, duration, action taken to alleviate symptoms, associated symptoms, etc.), medical conditions, medications used, and allergies during patient assessment and students subsequently providing appropriate advice to the patient. Therefore, the specific objectives are to: (1) describe the type and amount of information gathered; (2) describe the type and amount of advice provided, (3) measure the overall proportion of students providing appropriate advice, and (4) identify factors associated with the provision of appropriate advice.
METHODS
Ethics approval
Ethics approval was sought from the Ethical Committee University of Surabaya, Indonesia (No 057/KE/XII/2018). To protect the identity of the research setting and student participants, any identifying information was not allowed to be published.
Research context
In this particular university, topics related to self-medication services are provided to third year BPharm students. The course (COMM PHARM 1) comprises a 4 hour session per week, consisting of a 1-hour lecture and 3-hours of laboratory practice for 14 weeks. In the laboratory practice component, students are expected to be able to respond to a simulated patient (i.e., tutors or students acting as a patient) requesting self-medication for several minor ailments such as painful conditions, respiratory problems, gastrointestinal tract problems, skin problems, and eye and ear problems. The COMM PHARM 1 course is intended to provide competency in the provision of advice when responding to minor ailment requests to the level that supervised provision of advice to the public is subsequently able to be conducted in the apothecary programme.
Participant recruitment
All third year pharmacy students in the research site who had completed COMM PHARM 1 were eligible for recruitment. In the first week of semester 6, the researchers announced and explained the study to all enrolled students in COMM PHARM 2. Announcement was made in the COMM PHARM 2 class because this is the subsequent class that needs to be enrolled after third year students completing COMM PHARM 1. Several students who had completed COMM PHARM 1 but did not enrol in COMM PHARM 2, identified via the school data register, were also contacted separately. Students were asked to participate in a simulated patient assessment at a time that suited them. Free cakes/pastry/snacks were provided after participation and an extra-curricular student point which can be printed on their non-academic transcript upon graduation was also offered. Participation was voluntary with students who agreed to participate providing informed consent.
Study instrument
This study is a cross-sectional study. A simulated patient method was used to present the scenario of cough due to worsening of asthma. The scenario was adapted from Schneider et.al and was presented as both a product and symptom-based request (Online appendix).21 The data collection form was adapted from previous literature and consisted of a checklist of participants' characteristics, the type of information gathered and the advice provided.15,17 The types of information gathered included important information that needs to be gathered in patients with cough as stated by Blenkinsopp et al.16 The information elements comprised: patient identity, symptoms (including nature of cough, duration of cough, and accompanying symptoms including danger symptoms), action taken, medical conditions, medications used, and allergies. The types of advice provided were categorised as medical referral, recommending products, recommending non-pharmacological advice or other advice (including advice on follow up).17 As per previous literature, the appropriateness of the advice for this scenario was defined as direct medical referral.21 In order to adjust to the local context, four Indonesian academics and practitioners in pharmacy practice assessed the scenario for content validity and reviewed the data collection form. No significant changes were made in the scenario and the data collection form after being revalidated.
Seven simulated patients, consisting of two pharmacists who were PhD students, three recent pharmacist graduates, and two drug information pharmacists were recruited and trained beforehand. The training consisted of explanation of the scenarios, how to fill the data collection form, and role plays. Role plays were repeated until the simulated patients were deemed able to accurately enact the scenarios and fill in the data collection form as evaluated by the principal researcher (CB). Details of the characteristics of the simulated patients as well as the training is presented in Online appendix and is informed by an article by Resende et al.31
Data collection
One simulated patient was assigned to each student. During data collection, each participating student was presented with a product and a symptom-based request. For the product-based request, the simulated patients said "I want to buy woods® merah" (woods® merah is an Indonesian brand of cough medicines that contain dextromethorphan HBr and diphenhydramine HCl). For the symptom-based requests, the simulated patient started the conversation by saying "I want to buy medicines for cough, what do you recommend?". No further information was provided unless it was requested by the students. The whole process was audio-recorded. The simulated patients also recorded in writing all the information asked and the advice provided by participating students. After completing each meeting, the simulated patients validated the written data in the data collection form with the audio recorder.
Data analysis
Descriptive statistics (i.e. frequencies) were used to summarise data related to the types of information gathered and types of advice provided. Univariate followed by multivariate logistic regression was used to identify factors associated with the participants' provision of appropriate advice. Independent variables were derived from participant characteristics (i.e., gender, age, previous education, having working/training experience in community pharmacies, grade point average (GPA), and mark for COMM-PHARM 1 class), the number of questions asked, and the type of question asked (i.e., who is the patient, nature of cough, duration of cough, accompanying symptoms, action taken, medical conditions, medications used, allergies). The significant variables from the univariate analysis (p<0.05) were then entered into the multivariate model. A backward elimination method with a significance threshold of 0.05 was implemented to obtain the final, multivariate model. Odds ratios (OR) and 95% confidence intervals were calculated. IBM SPSS Statistics for Windows version 23 (Armonk, NY: IBM Corp) was used for the analysis.
RESULTS
Based on the faculty registration data, the population of third year students who had completed COMM-PHARM 1 in 2018 was 304. Of these, 183 agreed to participate in this study, resulting in a response rate of 60.2%. Details related to participants' characteristics are presented in Table 1.
Table 1. The comparison of demographic characteristics between participants and the total population
| Demographic characteristics | Sample n=183 (%) | Population n=304 (%) |
|---|---|---|
| Age in years; mean (SD) | 20 (0.95) | 20 (0.85) ∞ |
| Gender: female | 159 (87%) | 248 (82%) |
| Previous education | ||
| High school | 125 (68%) | 198 (70%)∞ |
| Pharmacy assistant school (equivalent to high school)^ | 58 (32%) | 84 (30%)∞ |
| Have any experience of working or training in community pharmacy | ||
| Yes | 54 (30%) | 80 (28%)∞ |
| No | 129 (70%) | 202 (72%)∞ |
| Average GPA*; mean (SD) | 2.8 (0.52) | 2.7 (0.56) |
| Mark for COMM PHARM 1 course:# | ||
| A | 0 | 1 (0,3%) |
| AB | 9 (5%) | 10 (3%) |
| B | 65 (36%) | 93 (31%) |
| BC | 65 (36%) | 100 (33%) |
| C | 33 (18%) | 67 (22%) |
| D | 11 (6%) | 33 (11%) |
| E | 0 | 0 |
∞Data is from 282 students
*The maximum Grade Point Average (GPA) is 4.
#The interpretation of the marking score were as follows: A = more than or equal to 81, AB = 73 to 81, B=66 to 72, BC= 60 to 65, C=55 to 59, D=40 to 54, E= less than 40. The maximum marking score is 100.
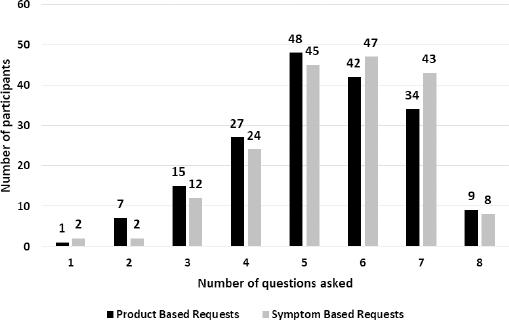
All students (100%) asked questions before providing advice. The average number of questions asked for product and symptom-based requests for cough due to worsening asthma scenarios were 5 and 6 with the standard deviation of 1.5 and 1.4 respectively. Information related to patient identity, and the nature and duration of cough were the most common types of information gathered in both scenarios (≥ 80% of the participating students). In contrast, accompanying symptoms, medications, and allergies were the least frequently gathered types of information; they were gathered in less than 60% of the participating students. Details related to the types and amount of information gathered can be seen in Figure 2 and Table 2.
Table 2. The types of information gathered
| The types of information gathered | Product-based request n=183 (%) | Symptom-based request n=183 (%) |
|---|---|---|
| Patient identity | 147 (80%) | 81 (81%) |
| Symptoms | ||
| Nature of cough | 158 (86%) | 165 (90%) |
| Duration of cough | 161 (88%) | 167 (91%) |
| Accompanying symptoms | 79 (43%) | 68 (37%) |
| Action taken | 125 (68%) | 131 (72%) |
| Medications | 91 (50%) | 106 (58%) |
| Medical conditions | 119 (65%) | 137 (75%) |
| Allergies | 93 (51%) | 88 (48%) |
The types and amount of advice provided by participants are outlined in Table 3. In the product-based request scenario, medical referral was advised by 99 students (54% of the 183 participants). Of these 99 students, 21 and 26 students also recommended cough medicines and non-pharmacological/follow-up advice, respectively. In the symptom-based request scenario, 102 students (56% of the 183 participants) recommended direct medical referral. Fifteen and 23 of these 102 students also recommended cough medicines and non-pharmacological/follow up advice, respectively.
Table 3. The types and amount of advice provided
| The types of advice provided | Symptom based requests n =183 (%) | Product based requests n=183 (%) |
|---|---|---|
| (1) Direct medical referral | 68 (37%) | 61 (33%) |
| (1) Direct medical referral and (2) suggesting medicines* | 11 (6%) | 12 (7%) |
| (1) Direct medical referral, (2) suggesting medicines, and (3) suggesting non-pharmacological advice or other advice.** | 5 (3%) | 9 (5%) |
| (1) Direct medical referral and (3) suggesting non-pharmacological advice, or other advice | 18 (10%) | 17 (9%) |
| (2) Suggesting medicines. | 29 (16%) | 29 (16%) |
| (2) Suggesting medicines and (3) suggesting non-pharmacological advice, or other advice. | 41 (22%) | 47 (26%) |
| (3) Suggesting non-pharmacological advice or other advice. | 1 (0%) | 4 (2%) |
| (4) No advice suggested.*** | 10 (6%) | 4 (2%) |
*Medicines suggested was a variety of cough medicine brand names.
**Examples of non-pharmacological advice or other advice including: enough rest, eat healthy food, drink a lot of water, avoid strenuous exercise, avoid dusty or unhygienic places, drink herbal medicines such as ginger and honey, and advising on follow up (such as go to a doctor if there is no improvement after tyring the suggested medicines, go back to the pharmacist if there is no improvement after trying the suggested medicines).
***No advice suggested meant that the students said that they did not know the answer or said that they did not know how to respond to the scenario in the simulated patient test.
Appropriate advice, which was defined as advice that contained direct medical referral, was provided in 99 (54%), and 102 (56%) of 183 participating students in the product-based requests and symptom-based requests, respectively.
From the univariate analysis, significant variables for providing appropriate advice comprised of asking about action taken and duration of cough in the product-based request scenario (Table 4). Meanwhile, significant variables for providing appropriate advice in the symptom-based request scenario consisted of: GPA, number of questions asked, asking about duration of cough, action taken, and other medical conditions (Table 5).
Table 4. Factors associated with the provision of appropriate advice - product-based request scenario
| Factors | Univariate analysis | |
|---|---|---|
| OR (95%CI) | p-value | |
| Age | 0.95 (0.696, 1.286) | 0.723 |
| Gender | 0.994 | |
| Male | 1.00 (0.424, 2.374) | |
| Female | Reference^ | |
| Previous education | 0.449 | |
| High school | 1.27 (0.682, 2.376) | |
| Pharmacy assistant school | Reference | |
| Have any experience in working or training in community pharmacies | 0.693 | |
| Yes | 0.88 (0.465, 1.663) | |
| No | Reference | |
| GPA | 1.42 (0.810,2.480) | 0.222 |
| Mark for COMM PHARM 1 course | ||
| AB | 0.71 (0.118, 4.319) | 0.654 |
| B | 0.86 (0.228, 3.224) | 0.820 |
| BC | 0.49 (0.131, 1.873) | 0.290 |
| C | 0.69 (0.168, 2.799) | 0.599 |
| D | Reference | |
| Number of questions asked | 1.16 (0.955, 1.417) | 0.132 |
| Asking who is the patient | 0.845 | |
| Yes | 0.93 (0.447, 1.934) | |
| No | Reference | |
| Asking nature of cough | 0.821 | |
| Yes | 1.10 (0.474, 2.566) | |
| No | Reference | |
| Asking duration of cough | 0.003* | |
| Yes | 4.77 (1.677, 13.566) | |
| No | Reference | |
| Asking accompanying symptoms | 0.413 | |
| Yes | 0.78 (0.435, 1.408) | |
| No | Reference | |
| Asking action taken | 0.020* | |
| Yes | 0.47 (0.250, 0.887) | |
| No | Reference | |
| Asking medications | 0.264 | |
| Yes | 1.40 (0.778, 2.500) | |
| No | Reference | |
| Asking medical conditions | 0.415 | |
| Yes | 1.29 (0.701, 2.370) | |
| No | Reference | |
| Asking allergies | 0.326 | |
| Yes | 0.75 (0.417, 1.338) | |
| No | Reference | |
*significant p value; ^the term "reference" category is a category of comparison for the other categories
Table 5. Factors associated with the provision of appropriate advice-symptom-based request scenario
| Factors | Univariate analysis | |
|---|---|---|
| OR (95%CI) | p-value | |
| Age | 1.01 (0.742, 1.376) | 0.949 |
| Gender | ||
| Male | 1.13 (0.473-2.695) | 0.784 |
| Female | Reference^ | |
| Previous education | ||
| High school | 1.56 (0.831, 2.909) | 0.167 |
| Pharmacy assistant school | Reference | |
| Have any experience in working or training in community pharmacies | ||
| Yes | 0.58 (0.307, 1.104) | 0.098 |
| No | Reference | |
| GPA | 1.82 (1.029,3.217) | 0.039* |
| Mark for COMM PHARM 1 course | ||
| AB | 1.40 (0.232, 8.464) | 0.714 |
| B | 2.31 (0.616, 8.682) | 0.214 |
| BC | 2.63 (0.698, 9.875) | 0.153 |
| C | 2.10 (0.514, 8.573) | 0.301 |
| D | Reference | |
| Number of questions asked | 1.26 (1.014, 1.553) | 0.037* |
| Asking who is the patient | 0.569 | |
| Yes | 1.24 (0.592, 2.594) | |
| No | Reference | |
| Asking nature of cough | 0.057 | |
| Yes | 1.33 (0.103, 1.034) | |
| No | Reference | |
| Asking duration of cough | 0.047* | |
| Yes | 3.05 (1.014, 9.167) | |
| No | Reference | |
| Asking accompanying symptoms | 0.735 | |
| Yes | 1.110 (0.606, 2.032) | |
| No | Reference | |
| Asking action taken | 0.022* | |
| Yes | 2.14 (1.114, 4.108) | |
| No | Reference | |
| Asking medications | 0.563 | |
| Yes | 1.19 (0.659, 2.148) | |
| No | Reference | |
| Asking medical conditions | 0.024* | |
| Yes | 2.18 (1.107, 4.310) | |
| No | Reference | |
| Asking allergies | 0.701 | |
| Yes | 1.12 (0.627, 2.003) | |
| No | Reference | |
*signifant p value, ^the term "reference" category is a category of comparison for the other categories
After inputting these significant variables into the multivariate analysis, we determined that the nature of the information gathering by students is associated with the provision of appropriate advice. In the product-based request scenario, students who asked about the duration of cough were more likely to provide appropriate advice than students who did not ask this question (OR 4.8, 95%CI 1.68-13.57). Meanwhile, in the symptom-based request scenario, students who asked about other medical conditions were more likely to provide appropriate advice than students who did not (OR 2.1, 95%CI 1.05-4.19). Demographic characteristics of participating students (i.e. age, gender, previous education, have working/training experience in community pharmacies, GPA, mark for COMM PHARM 1 course) were not associated with the provision of appropriate advice.
DISCUSSION
This is the first study in Indonesia that examined the ability of pharmacy students in gathering information and providing appropriate advice for a simulated patient with chronic cough. All students participated in this study were novice learners, which describes that they just learnt about self-medication consultation during their undergraduate pharmacy curriculum.
This study indicates that the information-gathering process among students in this school, needs to be improved. The lecture notes and laboratory practice module of COMM-PHARM1 class indicated that topics related to information-gathering have been provided. However, this study showed that students did not gather appropriate information when encountering our simulated patients. Important information such as medical conditions, medications used, and accompanying symptoms that are needed to enable students to identify the root of the problems were asked in 40% to 75% of the encounters. This contrasts with the results from an Australian study, in which most of their novice students perform well during the information-gathering process.32 While it is argued that complete information is not always necessary to be gathered in order to provide appropriate advice, it is safer for novice students to gather complete information for assessing patients correctly and hence appropriate advice.33
In this case, advice was considered appropriate when students recommended direct medical referral. However, in both scenarios, only about 55% of them were able to do so. This figure is about similar to findings from an Australian study, which stated that appropriate advice was provided in 52% of their novice students in the case of childhood fever.32 Other than incomplete information gathered as explained above, these participating students may also have limited knowledge of disease and therapy and inability to analyse the information gathered; and hence inappropriate advice.17,32 The syllabus in this pharmacy school shows that during semester 1 to 4, students only learn about basic sciences (human anatomy & physiology, pathophysiology, and pharmacology). Topics related to diseases and drug therapy, drug related problems, and patient counselling are provided in semester 5 and above. It could be that these students may not know that the case is cough due to worsening of asthma since they haven't learnt much about asthma, and therefore they did not know that direct medical referral was needed.
A potential factor to sub-optimal student performance is the teacher-student ratio. A review of the COMM PHARM1 classroom student list and tutor schedule identified that the teacher-student ratio was 1:20 during laboratory practices and 1:80 during lectures. Such ratios may be insufficient for students to receive adequate supervised practice and feedback during simulated role-plays. As the effectiveness of simulation learning relies on practice and feedback for each learner, measures should be undertaken to optimised the teacher-student ratio.34 Furthermore, with the current curriculum design, students are expected to be ready for supervised provision of minor ailment care to the public in the apothecary programme after completing the COMM PHARM1 course. This indicates that this one semester course carries a lot of weight in the curriculum. Redesigning the BPharm curriculum, such as by adopting the spiral curriculum in which key concepts are revisited and reinforced throughout the curriculum with increasing levels of complexity, could be more appropriate than a stand-alone course.35,36 Further qualitative research looking at the design of the current curriculum, students and teachers' perceptions, the teaching-learning process including the mode of delivery is required for designing interventions for the optimisation of student performance.
Simulated patient technique has been used widely in pharmacy education, including for training in consultation for self-medication requests.34 Using simulated patient technique as an educational tool may improve training since it can reinforce knowledge, integrate between knowledge and practice, and improve professional skills and attitudes (e.g., communication skills, decision making, emphaty, teamwork, social and cultural competency, and confidence).34,37 In addition as an educational tool, simulated patient technique can also be an assessment tool for evaluating the effectiveness of the training provided. Indeed, simulated patients in the form of OSCE is planned to be a compulsory element of the Indonesian national pharmacist registration examination.30 Evidence suggests that examinations using simulated patient technique challenges students to think critically and indicates student performance in real clinical encounters.37 Indonesian pharmacy schools, therefore, should use this technique in the teaching and evaluation of pharmacy students.
The multivariate analysis identified that asking a particular type of question (i.e., duration of cough and medical conditions) are factors positively associated with the provision of appropriate advice (Tables 4 and 5). This finding is in keeping with a previous Australian study in pharmacy staff responding to a very similar scenario.21 It could be that by asking such questions, students were able to discern that the patient had a contraindication for self-medication and recommend medical referral. It is important to train students to be able to ask key questions according to the clinical situation to improve the appropriateness of advice for minor ailments. Further, as there is a current lack of formal guidance on information-gathering when responding to patients with self-medication requests in Indonesia, policy makers such as the Indonesian Pharmacists Association (IAI), the Ministry of Health, and the APTFI may need to develop and promote a national protocol to improve appropriate information-gathering and to optimise the provision of care.
Research evaluating the competence of pharmacy students providing self-medication consultation in Indonesia is limited. Kristina et.al reported that 85% of 422 apothecary students from the University of Gadjah Mada, passed the the minor ailment station in their OSCE assessment.30 However, detailed aspects assessed in this minor illness station were not provided in the article and the population used were different with this study's population (apothecary students vs third year students in this study); thus making direct comparison difficult. It could be hypothesized that final year/apothecary programme students may have superior outcomes compared to students at an earlier stage in their education, as found in an Australian study.32
Despite the students in this study only being halfway through their pharmacist training, their performance was superior to Indonesian pharmacy staff, as reported in previous research.20,38 When responding to a simulated patient asking for a particular product for chronic cough, all of these students conducted information gathering and 54% of them were able to provide appropriate advice. In contrast, only 1% of pharmacy staff performed information gathering and none provided appropriate advice in the previous articles.20,38 Although the cases of chronic cough used between this study and the previous studies were not exactly the same, the essence and complexity of the cases are similar; and therefore we think they can be compared.
Better performance of these students compared to pharmacy staff as reported in the previous article may be due to several reasons. As stated in the theory of the Efficiency-Thoroughness Trade-Off (the ETTO principle), there is a balance or tradeoff between being efficient and being thorough.39 If demands to productivity are high, thoroughness is usually reduced. On the other hand, if demands to safety are high, efficiency is reduced. Following this theory, it could be that pharmacy staff were being efficient due to demands of high productivity, whereas students were being thorough because they knew that they were being assessed and therefore they will try harder to show their best performance. Another possible reason of why Indonesian pharmacy staff performed more poorly than students might be that the person that typically handles patients with self-medication requests in pharmacies is a non-pharmacist, as has been reported in Indonesian and other developing countries' literature.40-42 This being the case, measures should be taken to ensure that pharmacists are able to provide self-medication services when they are on duty. Further research on why students perform better than pharmacy staff is required.
Limitations
This study was only conducted in one pharmacy school in Indonesia. Because the quality of Indonesian pharmacy schools has been reported to vary, these findings may not be generalisable for all pharmacy students in Indonesia.28 Therefore, further research using samples of different pharmacy schools are required to obtain a general picture of Indonesian pharmacy students' ability in self-medication consultation. Furthermore, the study was conducted in novice students and therefore may not reflect the ability of pharmacy graduates. Future research on evaluating the ability of final year pharmacy students in handling self-medication consultation is also required. In addition, a Hawthorne effect may have been generated, because this is an overt method, in which participating students knew that they were being assessed. However, although these students have showed their best performance, only half of them were able to provide appropriate advice; and therefore there is still a need for improvement. Lastly, there was a possibility of selection bias in this study. However, the characteristics of the participating students were similar to the student cohort (Table 1) and therefore it might not significantly affect the findings.
CONCLUSIONS
The performance of novice students in responding appropriately to a simulated patient with a self-medication request for cough is sub-optimal. Appropriate information-gathering is a predictor of appropriate provision of advice. Measures to improve student performance, such as curriculum restructuring, optimising teacher-student ratio, and developing a protocol for appropriate information-gathering may be required. Further qualitative research to identify factors affecting student performance is required to develop strategies to improve student response to self-medication requests.