The core symptoms of Autism Spectrum Disorders (ASD) are persistent deficits in communication and social interaction and repetitive and restricted patterns of behaviours, activities and interests that cause significant impairments in social, occupational or other areas of personal functioning (APA, 2013, 2022). Studies on the aetiology of ASD suggest that the disorder may arise from an early alteration in brain development caused by an interaction between certain genetic abilities and environmental variables (Muhle et al., 2018). These alterations in brain development seem to focus, from the symptoms of the disorder, on areas related to socio-communicative functions among others (Alcantud-Marín & Alonso-Esteban, 2022). That is, as the structure and functioning of the brain is determined by interaction with the environment (Koizumi, 2004), a disturbance in the development of communication and social interaction will produce a cascading disorder (Mundy & Crowson, 1997). Early intervention to enhance social-communicative interactions, by taking advantage of brain plasticity in the early years, can mitigate symptoms of ASD (Artigas-Pallarés, 2007; Dawson et al., 2012; Holland et al., 2014; Pierce et al., 2016). The increasing prevalence rate evidenced in recent studies (CDC, 2020; Autism Europe, 2019), justifies interest in developing evidence on the efficacy of early intervention.
Many early intervention techniques and methods focus on the development of communication and social interaction functions (Prizant et al., 2003, 2006), including involving parents (Ingersoll & Dvortcsak, 2010; Ingersoll & Wainer, 2011, 2013). Review studies (Rojas-Torres et al., 2020) have demonstrated the positive influence of parental involvement in early intervention programmes. If infants show warning signs of autism and intervention is provided, there is an improvement in symptomatology (milder signs of autism and increased social interaction). This improvement manifests itself even years later (Green et al., 2017). Kim et al. (2017) identify that in addition to cognitive skills, parental involvement in early intervention at age 3 is a predictor of later academic performance. However, many parents report a high level of stress related to their child's disorder and intervention (Bluth et al., 2013).
Parenting requires resources that can sometimes exceed the means of one or both parents (Diener & Swedin, 2020). The feeling of exceeding one's means is a source of distress, anxiety and psychological discomfort and can be at the root of multiple disturbances in family coexistence and parenting (Mikolajczak et al., 2019). The scientific literature highlights that parent coping with parenting a child with developmental disorders experience a greater number and intensity of sources of distress and anxiety (Newacheck et al., 2004; Sen & Yurtsever, 2007). Distress and anxiety are present from the earliest warning signs (Hartley et al., 2010) and depending on the supports received, this stress tends to become chronic. Parents often seek help, either for impaired psychological well-being (Cachia et al., 2016; Falk et al., 2014; Firth & Dryer, 2013; Merkaj et al., 2013) or for high levels of stress (Almansour et al., 2013; Hayes & Watson, 2013). Parental stress also feeds back into personal stress, with consequences not only for parents, their personal stability and family relationships (Benn et al., 2012), but also for their children's psychological well-being and possible reduction in the effectiveness of intervention programs (Cachia et al., 2016). One of the most documented causes of high levels of stress is alterations in parent-child interaction patterns (Pons-Salvador et al., 2005; Osborne et al., 2008).
Parents and caregivers who are under high levels of stress tend to collapse, therefore, there is a need for targeted intervention for parents to improve coping with stress in order to improve family functioning (Bögels & Restifo, 2014). Research provides evidence for the positive changes produced by mindfulness practice (Boekhorst et al., 2020; Cachia et al., 2016; Gammer et al., 2020; Rojas-Torres et al., 2022). In particular, these mindfulness-based programmes offer positive effects on stress and anxiety management in parents of children with autism (Benn et al., 2012; Bluth et al., 2013; Cachia et al., 2016; Ferraioli & Harris, 2013). Preserving good parental health and well-being is a precondition for optimal care of children with autism (Keen et al., 2010).
The present clinical trial aims to train parents in Mindful Parenting (Bögels & Restifo, 2014) and play activities with their children as a start to communicative interaction. The concept of Mindful Parenting is directed towards the development of mindfulness in parents, children and family relationships and was already proposed in the early work of Kabat-Zinn (1997). For Ahemaitijiang et al. (2021), mindful parenting consists of five elements (awareness, attention, non-judgmental acceptance, compassion and self-regulation) through three orientations (parents, children and interaction between the two), defining it as "a parenting process in which parents make every effort to provide awareness, attention, non-judgmental acceptance and self-control" (Ahemaitijiang et al., 2021, p.3). In this sense, the hypothesis of interventions based on Mindfulness Parenting is to help reduce interparental conflict by reducing emotional reactivity in the partners, avoiding a spiral of negative feelings and guilt during parenting (Bögels et al., 2010).
Method
Participants
The management of ASPAU (Asociación Proyecto Autismo de Valencia -Spain-) was contacted, asking for their collaboration. From the ASPAU management, an e-mail was sent to all ASPAU members who fulfilled the condition of having an autistic son or daughter under four years old. An informative meeting was held with the researchers and parents interested in participating. At this meeting, only seven families attended, of which only four expressed their wish to participate. The response time to the call was extended and the families attended at the AVAPACE (Valencian Association for Cerebral Palsy Support) early care centre "Xicotets" were also contacted. The trial was conducted between October 2021 and March 2022. It was designed with a control group (waiting list) that would receive treatment afterwards. The inclusion/exclusion conditions were (a) Parents of children under 4 years old; (b) with a diagnosis of ASD confirmed by medical report; (c) that the participating parents lived with the children; and (d) that a signed informed consent form was submitted.
A total of fourteen participants were selected (six couples and two mothers) with ages between 30 and 51 years. The children were between 3 and 4 years old (7 boys and 1 girl), (see Table 1). With the exception of one family whose children were twins, all were so far only children (first child). All fathers, and more than 60% of mothers, were in paid employment, with average incomes (20.000-30.000€ annually). All of them parents provided a diagnostic report from the USMIAS (Child and Adolescent Mental Health Units). The reports took the data from the administration of the ADOS-2 (Autism Diagnostic Observation Schedule. Lord et al., 2012), confirming a level 3 (non-verbal or minimally verbal, avoided looking, some showed ecological language, little interest in interaction with adults or peers). All the children have been attending for at least one-year general comprehensive intervention programmes in early childhood centres. The two groups consisted of three couples and one mother, with the intervention took place on Fridays at 6 p.m. for a duration of two hours. The first group started treatment in October 2021 and finished in December. The second group remained without treatment (waiting list), and began the intervention in January 2022 and ended in March of the same year, maintaining the same timetable and operating rules.
Instruments
In order to test the effects of the Mindfulness Parenting program, a battery of tests was designed:
Generalized Anxiety Disorder (GAD-7; Spitzer et al., 2006), is self-report scales for screening, diagnosis and severity assessment of anxiety disorders. The GAD-7 score is the result of the sum of the responses to the items (5-point Likert type) and therefore informs us of the degree to which the symptoms have been present in recent weeks. The numerical value indicates the magnitude of the perceived anxiety. The Spanish version (Garcia-Campayo et al., 2010) has obtained excellent reliability (Cronbach's Alpha = 0.94) and high stability of the measure (Test-retest correlation of 0.84). In our trial, we will limit it to the last week in order to use the results as feedback to trial participants to assess the immediate results, adherence to treatment and whether any extraneous variable has influenced the variation in anxiety perceived by them.
Parental Stress Index Fourth Edition (PSI-4; Abidin, 2012), is a 120-item questionnaire used to explore parental stress levels. There is a short form (PSI-SF; Abidin, 2012) consisting of 36 items taken directly from the full form. The short form provides a Total Stress score (TS) that is a combination of three components: Parent Distress (PD), Difficult Child (DC) and Parent-Child Dysfunctional Interaction (P-CDI). The Spanish version of the PSI-SF (Díaz-Herrero et al., 2010, Rivas et al., 2021) was used in this study, showing internal consistency (McDonald's Omega = .84 -.94 and Cronbach's Alpha = .79 - .93), high convergent and diagnostic validity. All items are rated on a five-point Likert scale. The numerical magnitude expresses the perceived stress.
Autism Impact Measure (AIM; Kanne et al., 2014). It is a measure of frequency and impact of behaviors and symptoms characteristic of autism. It uses a double Likert scale (five points) to assess the frequency of certain symptoms and the impact (also five points). The result is the sum of the frequency and impact scores. It is composed of 41 items distributed in 5 subdomains: Repetitive Behavior (RB); Communication (C); Atypical Behavior (AB); Social Reciprocity (SR); Peer Interaction (PI). The numerical magnitude expresses the severity of symptoms as perceived by parents and caregivers. The numerical magnitude expresses the severity of symptoms as perceived by parents and caregivers. The original version offers acceptable internal consistency (Cronbach's Alpha = .66 - .79) and stability of the measure (test-retest = .53-.85).
Screen for Adult Anxiety Related Disorders (SCAARED; Angulo et al., 2017), is a version of the SCARED (Birmaher et al., 1997) for adults composed of 41 items Likert type assessing four major factors: Generalized Anxiety Disorder (GA), Social Anxiety (SA), Panic Disorder (PD) and Separation Anxiety Disorder (SAD). SAD was included among anxiety disorders in the DSM 5 (Silove et al., 2015; APA, 2013). The numerical magnitude expresses the severity of the perceived anxiety symptoms. The Spanish version of the SCAARED used in this study (Sánchez-Cueva et al., 2021) has very good internal consistency (Cronbach's alpha = .91) and test-retest stability (<.81).
Five Facet Mindfulness Questionnaire (FMMQ; Baer et al., 2006, 2008), is a self-report made up of 39 items that aims to measure mindfulness based on five domains: Observation (Ob), Description (Des), Acting with Awareness (AA), Absence of Judgement (AJ) and Absence of Reactivity (AR). The scores range from 39 points to 195, with higher scores indicating a greater state of mindfulness (Schmidt & Vinet, 2015). In this study we used the Spanish version of the FMMQ (Cebolla et al., 2012) which has high internal stability (Cronbach's Alpha = .80 -.91).
Procedure
The allocation of participants to the groups was not random and was determined according to the couple's possibilities of reconciling work and work schedules. While the parents received the Mindfulness Parenting training, the children were cared for by a group of volunteer students from the 3rd year of the Primary Education Teaching Degree (Therapeutic Pedagogy) guided by a member of the research team. The playroom of the "Xicotets" centre was available with various materials (balls, dolls, cars, construction games, etc.) and spaces specifically designed for play on the floor (ball pool, slides, swings, etc.). During this period of time the children engaged in non-directive play activities on the floor with the intention of improving communication and social interaction. Play-focused therapy techniques with children with autism have been used for some time, and have even been shown to be effective in meta-analysis studies (Bratton et al., 2005; Hillman, 2018; Leblanc & Ritchie, 2001), with results demonstrating changes in social-emotional and communicative development.
The clinical trial took place during the sixth wave of the COVID-19 pandemic. During the sessions, the recommended sanitary measures were maintained (use of masks, distance, temperature control, hand washing, etc.). In anticipation of possible quarantines, a course was designed on the Moodle platform (https://acceso.uv.es/Moodle) and a WhatsApp instant messaging group was creative. On the Moodle platform, participants could access all the material used in the face-to-face sessions. The sessions were carried out normally with no significant absences (never more than one family) which were compensated by the use of the telematic tools.
There was only one session in each group held for all attendees virtually due to the high incidence of COVID-19 infections among children and parents that week. This project was approved by the Human Research Ethics Committee of the University of Valencia, which ensures compliance with the principles of the Helsinki agreement (Code: H1541505018986).
Intervention Programme
For the development of the program, the manual of Bögels & Restifo (2014) was followed and consisted of 8 sessions (1 per week). The scheduled duration of each session was 90 minutes (See Table 2 for sessions description). Following the recommendations, a set of daily activity sheets was included ad hoc for home and work, specially adjusted to each session (between 15 and 30 minutes per day). During the first 15 minutes of each session, the participants expressed their thoughts about the material sent analyzed the records they made, and then the moderator therapist explained the activities for the following week. Each session was divided into two parts, the first part consisted of the development and training in Mindfulness exercises, being led by one of the authors of this article. The second part consisted of developing psychoeducation sessions on ASD with an active listening dynamic (Robertson, 2005; Rogers & Farson, 1957), led by the senior researcher, an expert in ASD.
Table 2. Brief Description of the Mindfulness Parenting Programme Sessions (Modified fromBogels & Restifo, 2014).
| Number session | Denomination | Brief Description |
|---|---|---|
| 1 | Automatic Parenting | The focus of the first session is to make parents aware of parenting on autopilot. It explores the reactions of parents in typical situations that can generate discomfort. We will teach them to stop before acting, particularly in those situations where they may present high levels of stress, and to take the time to act with intentionality. |
| 2 | Parental Awareness for Beginners | Parents share the experience of observing their children with awareness and often discover the positive qualities they had not been paying attention to when they were only looking at the children's difficulties. We talk about the predisposition to see children in a negative way, especially when they have received a diagnosis and how they tend to always see it in that context. On the other hand, we invited parents to use "kindness" as part of their parental experience, especially when they are experiencing stress levels. |
| 3 | Reconnecting with our bodies as parents | The main theme of this session is for parents to become aware of bodily sensations. We explore how often we forget about body signals and limits. The main idea is that parents reconnect with their body and take care of it. |
| 4 | Responding rather than reacting | This session will explore how many automatic responses occur when we respond to stress and how our thoughts can generate more of these situations. A relaxed state and knowing how to breathe can help us get out of automatic stress reactions, to learn to stop and respond more intentionally. |
| 5 | Parenting Patterns and Schemes | Parents learn to recognize the anger and reactions they may have to situations that create difficulties with their children. The main practice in this session is self-compassion and acceptance mainly in situations of emotional difficulty involving their children. |
| 6 | Conflict and parenting | In this program parents have had the opportunity to practice "self-compassion" and "acceptance" on themselves, now we ask them to do this practice on the emotional states of their children. We ask parents to be able to recognize and manage their own emotions and simultaneously those of their children. |
| 7 | Love and boundaries | This session has two main themes. The aim is to extend the practice of self-compassion and to formally introduce "lovingkindness" by developing our capacity to love and be kind by exploring boundaries within parenting. |
| 8 | Conscious Path through Parenting | We will reflect on the program and ask if parents have felt any changes personally, outside and inside the home. Some parents may have had difficulties during this process and others may have had moments of introspection and change. |
Data Analysis
The design of two groups was made. The first group (A) received the Mindfulness Parenting training while the second group (B) remains on the waiting list. At a second stage, the first group (A) remains on the waiting list without receiving treatment in the follow-up phase while the second group (B) received the same Mindfulness Parenting training program (see Figure 1).
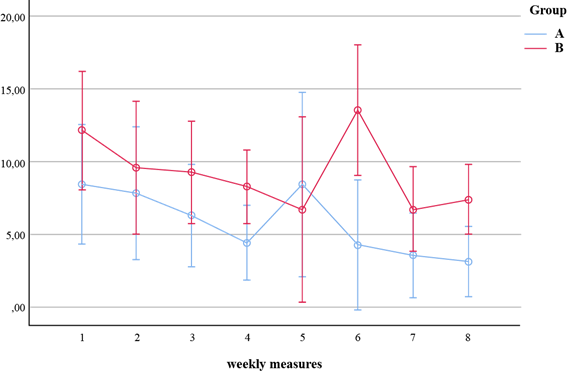
Two types of measures were taken. On the one hand, weekly measures of the level of generalised anxiety using the GAD-7 to analyse treatment effects and give feedback to participants, and on the other hand, pre- and post-test measures.
The repeated measures at the three points in time in the two groups required a two-group repeated measures ANOVA (Mitchell & Jolley, 2010). All the calculations were made with SPSS, version 26, licensed by the University of Valencia.
Results
As a direct result of the intervention, a decrease in generalized anxiety as measured by the GAD-7 was observed. In other words, the ANOVA results (see Table 3 and Figure 2) showed that the decrease in anxiety levels in the two groups and over the course of the treatment was significant (p< .01).
Table 3. Results of Repeated Measures (ANOVA) for Generalised Anxiety Across the 8 Weeks of Intervention.
| ANOVA GLM | ANOVA Reaped Measures | |||||||||||
| Measures | Measures group | Effect Sizes and Powers | ||||||||||
| Partial eta-squared | Observed power (alpha= 0.05) | |||||||||||
| F | p | Eta2 | Power | F | p | F | p | Measures | Measures group | Measures | Measures group | |
| GAD | 73.67 | .00 | .86 | 1.00 | 3.05 | .00 | 2.14 | .12 | .20 | .15 | .92 | .78 |
Note.GLM: General Linear Model. GAD: Generalized Anxiety Disorder index evaluated with GAD-7 (Spitzer, et al., 2006)
In Table 4, the descriptive data for the four scales used are presented and in the Table 5, we present the details of the variance model for each variable measured. In addition, post-hoc tests were performed to compare the different measures that emerged as significant.
Table 4. Means and Standard Deviations of the Measures Used for Both Groups.
| Measure 1 | Measure 2 | Measure 3 | |||
|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | |||
| Group | |||||
| PSI-4 | TS | A | 88.00 (17.30) | 80.71 (22.20) | 84.29 (26.05) |
| B | 105.71(15.45) | 100.86 (19.76) | 84.00 (20.88) | ||
| PD | A | 30.71 (7.54) | 27.28 (8.82) | 28.28 (10.64) | |
| B | 34.00 (8.98) | 34.29 (9.15) | 29.71 (11.83) | ||
| DC | A | 19.00 (4.36) | 17.00 (6.55) | 17.14 (6.30) | |
| B | 21.43 (4.57) | 21.28 (5.12) | 18.00 (7.16) | ||
| P-CDI | A | 27.57 (7.23) | 25.85 (7.22) | 26.85 (7.45) | |
| B | 35.42 (7.04) | 31.57 (9.38) | 25.42 (7.21) | ||
| AIM | RB | A | 31.14 (16.75) | 32.29 (9.98) | 30.43 (12.97) |
| B | 34.57 (6.16) | 33.87 (5.87) | 34.29 (5.99) | ||
| C | A | 34.00 (4.65) | 31.85 (7.77) | 34.71 (10.22) | |
| B | 31.43 (2.37) | 32.71 (3.77) | 31.00 (2.94) | ||
| AB | A | 28.14 (9.60) | 24.42 (5.02) | 24.29 (6.72) | |
| B | 23.29 (4.68) | 25.86 (8.34) | 23.57 (6.32) | ||
| SR | A | 28.86 (8.15) | 29.00 (6.61) | 31.14 (6.30) | |
| B | 32.43 (5.86) | 30.57 (7.18) | 27.86 (5.67) | ||
| PI | A | 21.43 (2.82) | 22.29 (2.98) | 25.14 (3.72) | |
| B | 23.86 (4.63) | 23.14 (4.06) | 23.00 (6.48) | ||
| TAI | A | 143.57 (27.55) | 139.86 (14.54) | 145.71 (23.31) | |
| B | 145.57 (12.99) | 146.14 (13.93) | 138.71 (14.53) | ||
| SCAARED | PD | A | 6.29 (5.44) | 3.14 (3.89) | 4.00 (3.31) |
| B | 8.00 (4.24) | 8.43 (4.35) | 4.71 (4.23) | ||
| GA | A | 14.00 (7.37) | 8.71 (3.99) | 9.71 (4.54) | |
| B | 15.29 (5.02) | 16.00 (5.48) | 14.00 (5.63) | ||
| SA | A | 2.71 (1.89) | 1.28 (1.25) | 2.14 (1.68) | |
| B | 5.29 (1.49) | 5.43 (1.51) | 4.29 (1.60) | ||
| SAD | A | 3.57 (4.03) | 3.71 (5.12) | 3.57 (4.31) | |
| B | 7.14 (3.08) | 8.00 (3.06) | 5.42 (2.70) | ||
| TA | A | 27.14 (16.56) | 17.14 (12.82) | 19.71 (12.24) | |
| B | 36.00 (11.46) | 38.14 (11.27) | 28.57 (11.45) | ||
| FFMQ | Ob | A | 25.57 (7.98) | 31.00 (2.76) | 26.28 (4.61) |
| B | 23.57 (6.19) | 22.71 (4.30) | 23.43 (5.74) | ||
| Des | A | 28.71 (4.61) | 31.29 (3.45) | 30.43 (5.94) | |
| B | 23.86 (4.84) | 24.14 (5.67) | 25.14 (7.24) | ||
| AA | A | 26.43 (6.92) | 27.43 (5.29) | 27.43 (5.26) | |
| B | 23.28 (6.73) | 24.00 (4.97) | 24.57 (5.62) | ||
| AJ | A | 23.57 (7.72) | 25.29 (4.11) | 26.86 (3.94) | |
| B | 23.86 (6.51) | 23.14 (5.87) | 27.14 (5.40) | ||
| AR | A | 22.57 (5.09) | 25.00 (3.06) | 21.00 (4.00) | |
| B | 21.28 (3.20) | 22.00 (3.83) | 22.00 (4.94) |
Note.Total Parental Stress (TPS); Parent Distress (PD); Difficult Child (DC ); Dysfunctional Parent-Child Interaction (P-CDI); Repetitive Behavior (RB); Communication (C); Atypical Behavior (AB); Social Reciprocity (SR); Peer Interaction (PI); Total Autism Impact (TAI); Panic Disorder (PD); Generalized Anxiety Disorder (GA); Social Anxiety (SA); Separation Anxiety Disorder (SAD); Total Anxiety (TA); Observation (Ob), Description (Des), Acting with Awareness (AA), Absence of Judgement (AJ) and Absence of Reactivity (AR) .
Table 5. Results of Repeated Measures Analysis (ANOVA) for PSI-4, AIM, SCAARED and FFMQ.
| ANOVA | GLM | ANOVA Reaped Measures | |||||||||||
| Measures | Measures group | Effect Sizes and Powers | |||||||||||
| Partial eta-squared | Observed power (alpha=0.05) | ||||||||||||
| F | p | Eta2 | Power | F | p | F | p | Measures | Measures group | Measures | Measures group | ||
| PSI-4 | TPS | 321.83 | .00 | .96 | 1.00 | 5.73 | .00 | 4.41 | .02 | .32 | .27 | .82 | .70 |
| PD | 162.47 | .00 | .93 | 1.00 | 2.44 | .11 | 1.74 | .19 | .17 | .13 | .44 | .33 | |
| DC | 178.85 | .00 | .94 | 1.00 | 3.17 | .06 | 1.32 | .29 | .21 | .10 | .55 | .26 | |
| P-CDI | 256.05 | .00 | .95 | 1.00 | 5.18 | .01 | 4.21 | .03 | .30 | .26 | .77 | .69 | |
| AIM | RB | 161.06 | .00 | .93 | 1.00 | .08 | .92 | .21 | .81 | .01 | .02 | .06 | .08 |
| C | 625.84 | .00 | .98 | 1.00 | .07 | .93 | 1.09 | .35 | .01 | .06 | .08 | .22 | |
| AB | 274.75 | .00 | .96 | 1.00 | .74 | .49 | 1.30 | .29 | .06 | .16 | .10 | .25 | |
| SR | 394.63 | .00 | .97 | 1.00 | .26 | .78 | 2.27 | .13 | .52 | .16 | .09 | .42 | |
| PI | 602.16 | .00 | .98 | 1.00 | 1.01 | .38 | 2.10 | .14 | .08 | .15 | .21 | .39 | |
| Total | 1131.88 | .00 | .99 | 1.00 | .14 | .87 | 1.14 | .34 | .012 | .09 | .07 | .23 | |
| SCAARED | PD | 33.86 | .00 | .74 | 1.00 | 3.85 | .04 | 2.88 | .08 | .24 | .19 | .64 | .51 |
| GA | 88.59 | .00 | .88 | 1.00 | 6.62 | .005 | 6.76 | .005 | .36 | .36 | .87 | .88 | |
| SA | 88.20 | .00 | .88 | 1.00 | 3.04 | .07 | 4.82 | .02 | .20 | .28 | .53 | .74 | |
| SAD | 30.23 | .00 | .71 | .99 | 2.40 | .11 | 1.98 | .16 | .17 | .14 | .44 | .37 | |
| TA | 76.47 | .00 | .86 | 1.00 | 5.94 | .008 | 5.29 | .01 | .33 | .31 | .83 | .78 | |
| FFMQ | Ob | 398.03 | .00 | .97 | 1.00 | 1.89 | .17 | 3.54 | .04 | .14 | .23 | .35 | .60 |
| Des | 455.22 | .00 | .97 | 1.00 | 1.02 | .38 | 5.17 | .59 | .08 | .04 | .21 | .13 | |
| AA | 318.13 | .00 | .96 | 1.00 | .60 | .56 | .04 | .96 | .05 | .003 | .14 | .06 | |
| AJ | 311.05 | .00 | .96 | 1.00 | 5.92 | .008 | .93 | .41 | .33 | .07 | .83 | .19 | |
| AR | 485.78 | .00 | .97 | 1.00 | 4.29 | .02 | 3.89 | .03 | .26 | .25 | |||
Note.(TPS), Total Parental Stress; (PD), Parent Distress; (CC), Child Characteristics; (P-CDI), Dysfunctional Parent-Child Interaction; (PD) Panic Disorders; (GA) Generalized Anxiety Disorder; (SA), Social Anxiety; (SAD) Separation Anxiety Disorder; (AT) Total Anxiety; (RB), Repetitive Behavior; (C), Communication; (AB), Atypical Behavior; (SR), Social Reciprocity; (PI), Peer Interaction; (TAI) Total Autism Impact; (Ob), Observation, (Des) Description, (AA) Acting with Awareness, (AJ) Absence of Judgement and (AR) Absence of Reactivity
Firstly, with respect to the PSI-SF scale, we found that there are significant differences between the groups in all dimensions (PD, CD and P-CDI) and in total parental stress. These differences are greater at the beginning of the treatment and tend to disappear at the end of the treatments. A significant improvement between the assessment measures comprising the training phase (pre-post) in both groups is noteworthy. The results show that there is a significant decrease in total parental stress TPS (F (2,24) = 5.73 p=.00) due to a decrease in anxiety derived from the characteristics of the children DC (F (2,24) = 3.17 p=.06) and from the dysfunctional parent-child interaction P-CDI (F (2,24) = 5.18, p= .01). However, post hoc tests show that only P-CDI and TPS show significant differences between the different measures (see Table 6 and Figure 3).
Table 6. Post Hoc Test (p): Significance of the Differences Between Measures Based on the Estimated Marginal Means of PSI-4.
| Measures Group A | ||||
|---|---|---|---|---|
| Measures Group B | 1 | 2 | 3 | |
| P-CDI | 1 | - | .07 | .62 |
| 2 | .08 | - | .54 | |
| 3 | .02* | .14 | - | |
| TPS | 1 | - | .08 | .41 |
| 2 | .08 | - | .19 | |
| 3 | .03* | .08 | - | |
Note. (*)p < 0.05
Total Parental Stress (TPS);; Dysfunctional Parent-Child Interaction (P-CDI);

Figure 3. Graphical Representation of Total Parental Stress Levels and Dysfunctional Parent-Child Interaction as Assessed by the PSI-4 SF at the three Intervention Times.
The AIM results show that although there are differences in the perception of severity between groups A and B in all subdomains, these remain unchanged across the three measures. No change in parents' assessment of symptom severity was expected. However, it was necessary to measure it in order to show that the decrease in the level of stress does not imply a decrease in the assessment of their children's autistic symptoms (see Table 5).
Four types of anxiety were assessed using the SCAARED (Angulo et al., 2017). In SAD, no treatment-dependent changes were generated. However, there was a decrease in GA (F (2,24) =6.62 p= .005), SA (F (2,24)= 3.04 p= .07) and PD (F (2,24)=3.85 p=.04) and total anxiety TA (F (2,24)= 5.94 p=.008) , during the treatment phases (see Table 7 and Figure 4).
Table 7. Post Hoc Test (p): Significance of the Differences Between Measures Based on the Estimated Marginal Means of SCAARED.
| Measures Group A | ||||
|---|---|---|---|---|
| Measures Group B | 1 | 2 | 3 | |
| GA | 1 | - | .01* | .02* |
| 2 | .37 | - | .04* | |
| 3 | .29 | .22 | - | |
| SA | 1 | - | .04* | .00** |
| 2 | .60 | - | .00** | |
| 3 | .00** | .00** | - | |
| PD | 1 | - | .05* | .24 |
| 2 | .40 | - | .38 | |
| 3 | .10 | .08 | - | |
| TA | 1 | - | .00** | .04* |
| 2 | .26 | - | .12 | |
| 3 | .11 | .08 | - | |
Note. (*)p < 0.05;
(**)p < 0.01
Generalized Anxiety Disorder (GA); Social Anxiety (SA); Panic Disorder (PD); Total Anxiety (TA).

Figure 4. Graphical Representation of the Changes Produced by the Programme in Three Types of Anxiety Assessed by SCAARED.
The post hoc tests were, with the general anxiety measures, more significant than in the case of parental stress. In the Table 6 shows the results of the post hoc contrasts for group A (upper half) and group B (lower half). These differences focus on TA, GA, SA and PD. It is noteworthy that the greatest overlaps occur precisely in Social Anxiety, probably due to the stigma that parents suffer as a result of the diagnosis.
The evaluation of the effects of mindfulness training has been assessed by means of the FFMQ (Baer et al., 2006, 2008). Although the two groups start from similar initial positions, only two of the five dimensions AJ (F (2,24) = 5.92 p= .008) and AR (F (2,24) = 4.29 p= .02) change during treatment (see Tables 8 and Figure 4).
Table 8. Post hoc test (p): Significance of the Differences Between Measures Based on the Estimated Marginal Means of FFMQ.
| Measures Group A | ||||
|---|---|---|---|---|
| Measures Group B | 1 | 2 | 3 | |
| AJ | 1 | - | .28 | .08 |
| 2 | .18 | - | .05* | |
| 3 | .14 | .07 | - | |
| AR | 1 | - | .10 | .16 |
| 2 | .18 | - | .00** | |
| 3 | .52 | 1.00 | - | |
(*)p < 0.05;
(**)p < 0.01
Absence of Judgement (AJ) and Absence of Reactivity (AR) .

Figure 5. Graphical Representation of Two of the Five Dimensions of the FFMQ in Which Changes Have Occurred During Treatment.
The post hoc tests were, with the measures of the effects of mindfulness training less significant than in the previous cases, concentrating in both variables on the comparison between measure 2 and 3 in group A (treatment follow-up). Table 7 shows the results of the post hoc contrasts for group A (upper half) and group B (lower half). These differences focus on Absence of Judgement (AJ) and Absence of Reactivity (AR) being significant only in group A and during the follow-up phase (see Figure 5). These results make us think that it is possible that the results of mindfulness training are more evident over longer periods of time, opening up a new working hypothesis.
Qualitative Data Analysis
Following the recommendations of the Mindfulness programme, a set of recording sheets for daily activities was designed. Formal Practices (FP) and Informal Practices (IP) were differentiated. The FP refers to the practical sessions in which parents had to repeat the methods and techniques learned during the previous session. The IP refers to the incorporation of mindfulness into some routine daily activity.
From the analysis of the qualitative records, it was found that parents had a high adherence to the programme. They also reported that this kind of programmes are a great tool for parents of children with autism, especially for those who have been recently diagnosed with autism. The families in this trial, week after week, reported the usefulness of the activities in the session and the tasks they had to do at home. This helped them to be more aware of their relationships with their children and their partners. In this sense, the participation of both members of the couple (when there was one) was positively valued as it allowed for better organisation at home and an appreciation of the effort made. They also highlighted the importance of having a support group with people who were going through similar situations, as it allowed them to share personal experiences or feelings, coping strategies or to receive direct information about the diagnosis and treatments. According to parents, this space not only allowed them to work on their mental health and relationships with their children, but it was also a space where they could solve practical doubts, and contributions were mostly received by the other participants.
Discussion
There is evidence in the literature that parents of children with autism report more mental health problems than parents of children with neurotypical development (Falk et al., 2014). In particular, parents and caregivers of children with autism often report high levels of stress (Dabrowska & Pisula 2010), anxiety and depression (Rezendes & Scarpa, 2011). In some early intervention programmes, parents are directly targeted as agents of the early intervention process (Minguela & Alcantud-Marín, 2022). This demand, sometimes increases the stress on the couple or on one of the partners who feels overwhelmed. In community-based early childhood centres in Spain, different comprehensive programmes are followed. Attention to families is usually reduced to orientation, coordination and psychoeducation. The aim of this trial is to demonstrate that a brief intervention (8 weeks) can improve parents' stress and anxiety levels and, as a consequence, create more and better interactions with children. However, it has only been in the last few years that stress coping techniques for parents have been incorporated into early intervention programs (Rojas-Torres et al. , 2021). Quality information based on scientific evidence is undoubtedly the greatest support we can give to parents, but it is not enough. To the extent that our activity is recognized, is a reference, we will achieve greater adherence to the treatment guidelines that we propose. Parents need strong additional support and even guidelines to cognitively restructure the situation, come to terms with their new reality and develop new coping strategies.
All these problems impact on both personal and family well-being (Hartley et al., 2017), as well as on child development. Keen et al. (2010) establishes as a precondition for the optimal care of an autistic child the preservation of good mental health and well-being of the parents. It is essential that the determinants of stress, anxiety and depression are clearly identified in the intervention programs. In this line, it is necessary to remember that the results of this trial are based on the participation of parents of children with a high demand for support (level 3) and its implications. That experiences of mutual social support are generated among the participants in the program and that they experience how to deal with maladaptive behaviors of children, regulating their reactivity. In this context, mindfulness parenting program aimed at improving parent-child interaction and reducing parental reactivity have been shown to be effective in reducing parental stress by improving the level of communicative interaction between parents and children. However, these types of interventions have been scarcely studied in a time window close to the diagnosis of ASD. Implementing brief interventions based on mindfulness parenting within the framework of the care received by parents in early intervention centres can enhance the positive effects of intervention programmes on children.
The results of the intervention programme presented here demonstrate a post-treatment decrease in parents' self-reported anxiety values that could lead to positive changes in the psychological well-being and quality of life of the families. The demonstration of this fact opens up new lines of research since psychological well-being and quality of life do not only depend on a low level of anxiety.
Perhaps the most important limitation of the present study relates to the small number of participants. However, it is important to note that for the group dynamics to be adequate, the number of participants must be small. In terms of strength, we believe that the results demonstrate how mindfulness training can reduce the levels of stress and anxiety related to raising a child with autism.