Workplace violence is extensive in the health sector, and the problem of aggression toward healthcare professionals is global and increasing (Gates, 2004; Kuehn, 2010). Currently, violence against these professionals, especially nursing professionals, is a significant, worldwide concern for all healthcare areas (World Health Organization, 2012).
Workplace violence is defined as incidents in which personnel suffers abuse, sexual harassment, threats, or attacks in work-related circumstances, which explicitly or implicitly endanger their safety, well-being, or health (Norwegian Labour Inspection Authority, 2009).
Research outcomes vary considerably due to the different methodologies employed, the diversity of instruments, and assessment criteria, making it difficult to provide the incidence/prevalence rates of violent acts within the healthcare setting (Franz, Zeh, Schablon, Kuhnert, & Nienhaus, 2010; Kling, Yassi, Smailes, Lovato, & Koehoorn, 2009; Roche, Diers, Duffield, & Catling-Paull, 2010). For example, in the general healthcare setting, some studies find prevalence rates for physical violence ranging between 11% and 25% (Galián-Muñoz, Llor-Esteban, & Ruiz-Hernández, 2012; Gerberich et al., 2004; Roche et al., 2010), or even higher, around 35-71% (Hahn et al., 2010; Zampieron, Galeazzo, Turra, & Buja, 2010). With regard to non-physical aggression, the prevalence is even more difficult to assess, ranging between 38% and 90%, according to recent studies (Galián-Muñoz et al., 2012; Gascón et al., 2009; Roche et al., 2010).
The problem of aggression toward clinical staff has been the target of many studies, especially focusing on Mental Health Services and Emergency Units. Thus, a study of Magnavita and Heponiemi (2012) found that the Psychiatry and Emergency staff ran the highest risk of physical aggression, especially the workers in Mental Health Services, whose risk rate was 22 times higher than that of the other services. Different studies have studied the Emergency Units as a focus of aggressions, assuming that these professionals run greater relative risk than other specialties (James, Madeley, & Dove, 2006; Winstanley & Whittington, 2004). Other studies report that hospital violence occurs more frequently in psychiatric units, emergency units and geriatric units (Osuna, López-Martínez, Arce, & Vázquez, 2015; Spector, Zhou, & Che, 2014). There is a consensus that, within the healthcare sector, the nursing staff is one of the professional groups with the highest incidence of aggressions (Franz et al., 2010; Kling et al., 2009; Roche et al., 2010; Shields & Wilkins, 2009). According to Albashtawy (2013), the reason for this could be their physical proximity to the patients and relatives as care providers. Specifically, mental health nurses are considered the professional group with the highest probability of suffering aggressions (Murphy, 2004; Wei, Chiou, Chien, & Huang, 2016). In this sense, it has been noted that 80% of mental health nurses have suffered violence, whereas in the rest of the clinical staff, this percentage does not exceed 41% (Dack, Ross, Papadopoulos, Stewart, & Bowers, 2013).
This is also the case in Emergency Units, where the staff is often exposed to violent behaviors in emergency situations. According to the study of Ryan and Maguire (2006), 20% of the nurses had experienced sexual intimidation, harassment, or assault in the past month. Likewise, another study (Opie et al., 2010) reported that the most frequent kind of violence experienced in these units was verbal aggression (80%), followed by physical aggression (28.6%), and sexual harassment (22.5%).
However, it is agreed that aggressive incidents are not limited only to Mental Health Services and Emergency Units; some studies find similar rates in other services considered as of lower risk. For example, May and Grubbs (2002) found that between 35% and 80% of the nursing staff in the Emergency Units, the Intensive Care Units (ICUs), and in-patient wards had been physically attacked at least once while working. Magnavita (2014) and O’Connell, Young, Brooks, Hutchings, and Lofthouse (2000) reported that surgery nurses often suffer aggression by their patients. There are also data reflecting less conflictiveness in certain services. In this sense, Gacki-Smith et al. (2009) found that pediatric staff reported the least physical violence in comparison with other specialties.
As in other settings (Amado, Arce, & Herraiz, 2015), in the healthcare setting, aggression has an impact on professionals’ psychological adjustment, producing physical, psychological, and/or economic consequences for these workers (Pompeii et al., 2013). They may experience anger, fear, or irritation along with feelings of humiliation and guilt (Ayranci, Yenilmez, Balci, & Kaptanoglu, 2006; El-Gilany, El-Wehady, & Amr, 2010; Ruiz Hernández, García Jiménez, Llor Esteban, & Godoy Fernández, 2015), or they may consider that filing a complaint about such acts-even acts of physical violence-is a sign of weakness (Gacki-Smith et al., 2009). Other studies report job dissatisfaction, which translates into a decrease in the level of care, changing the workplace, or quitting the profession (Alameddine, Mourad & Dimassi, 2015; Fernandes et al., 2002; Kowlaenko, Walters, Khare, Compton, & Michigan College of Emergency Physicians Workplace Violence Task Force, 2005). Exposure to violence can also generate burnout, reactive psychopathological syndromes, substance abuse, or abuse of psychotropic medication (Dement, Lipscomb, Schoenfisch, & Pompeii, 2014; Estryn-Behar et al., 2008; Ünsal Atan et al., 2013). At the organizational level, there may be economic consequences for the company due to absenteeism or the loss of capable workers (Franz et al., 2010; Kneller & Harvey, 2016; Roche et al., 2010).
In this context, a research was designed with the aim of studying users’ hostile expressions against the nursing professionals of different public hospitals that report to the Murcian Health Service (MHS), in the Region of Murcia (Spain). Specifically, it was planned to determine the frequency of exposure in the past year to diverse violent user behaviors, as well as the sociodemographic and socio-occupational characteristics associated with greater exposure to this type of behaviors. The levels of violence between two high-risk services (Mental Health and Emergency Units) were compared with two other services (Medical Hospitalization and Maternal-and-Child) that present no evidence of suffering greater exposure to violence than the rest of the services. Lastly, the relation between exposure to hostile behaviors and the presence of possible consequences, such as variations in job satisfaction, burnout, and psychological well-being were analyzed.
Method
Participants
A sample of 518 participants was obtained from all the public hospitals in Murcia (southeastern Spain) that had Psychiatric Hospitalization Units (out of a total of 9 hospitals, we included in the project all 4 hospitals having these units). The study included two professional categories (nurses and auxiliary nursing staff) from 4 services: Mental Health, Emergency Units, Medical Hospitalization, and Maternal-and-Child Units, and the sample represents 30% of the total nursing staff of the selected hospitals. A total of 620 questionnaires were initially handed out, getting a global response rate of 83.55%.
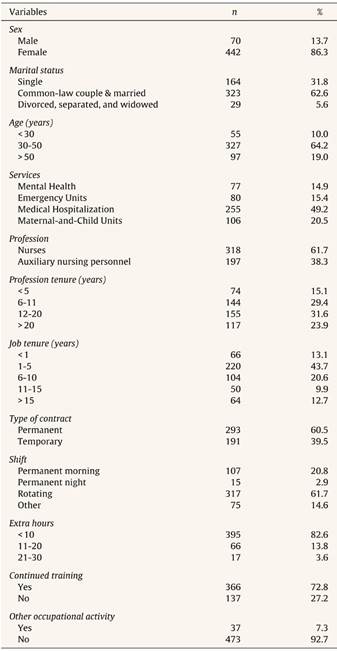
Of the sample, 61.4% were professional nurses and 38% were auxiliary nursing staff. Participants’ mean age was 41.3 years (SD = 9.57), ranging between 24 and 63 years. The majority were female (85.3% vs. 13.5%), with a predominance of married persons or persons living with a partner (62.4%). Regarding job characteristics, 14.9% of the professionals belonged to the Mental Health Service, 15.45% to the Emergency Units, 49.23% to Medical Hospitalization, and 20.46% to Maternal-and-Child Units (see Table 1 below).
Design
A cross-sectional, descriptive-analytic design was used, applying a series of psychological and socio-occupational measurement instruments to a sample of professional nurses and auxiliary nursing staff from public hospital services of the MHS. For this purpose, the guidelines of the STROBE statement for observational and analytic studies (Von Elm et al., 2007) were followed. The study was approved by the Ethics Committee of the University of Murcia (Spain), and by the board of executives of all participating hospitals.
Measurement Instruments
An assessment protocol made up of a questionnaire of sociodemographic and work variables designed ad hoc for the study and four validated psychological assessment instruments were analyzed.
Ad hoc questionnaire of sociodemographic and work variables. Sociodemographic data such as age, sex, and marital status, and work data such as type of service, tenure at work, tenure in the profession, type of contract, shift, and extra hours were collected.
Healthcare-workers Aggressive Behavior Scale-Users (HABS-U; Waschgler, Ruiz-Hernández, Llor-Esteban, & García-Izquierdo, 2012). This scale measures users’ low-intensity hostile verbal and physical manifestations. The frequency of each situation is rated on a 6-point Likert-type scale, ranging from 1 (never in the past year) to 6 (daily). The questionnaire has 10 items divided into two factors: non-physical violence (7 items) and physical violence (3 items). In this study, Cronbach's alpha was .83 for the total scale and .84 and .78 for the non-physical and physical violence subscales, respectively.
Maslach Burnout Inventory - General Survey (MBI-GS). This inventory was designed by Schaufeli, Leiter, Maslach, and Jackson (1996), translated to Spanish, and validated by Gil-Monte (2002). This version has 16 items that assess 3 dimensions: emotional exhaustion (5 items), professional efficacy (6 items), and cynicism (5 items). Participants rate each item of the questionnaire on a Likert-type scale ranging from 0 (never) to 6 (always). In our sample, we obtained alphas of .87 (emotional exhaustion), .86 (professional efficacy), and .73 (cynicism).
General Health Questionnaire (GHQ-28). Designed originally by Goldberg and Hillier (1979), this questionnaire was adapted to Spanish by Lobo, Pérez-Echevarría, and Artal (1986) and is made up of 28 items distributed in 4 subscales: somatic symptoms of psychological origin (somatic GHQ), anxiety/insomnia (anxiety GHQ), social dysfunction (dysfunction GHQ), and depressive symptomatology (depression GHQ). Each item has four possible responses, scored from 0 to 3, ranging from lower to higher symptom intensity. In our study, we obtained alphas of .85 (somatic symptoms), .90 (anxiety), .69 (social dysfunction), and .87 (depression).
Overall Job Satisfaction Scale (OJS). Designed by Warr, Cook, and Wall (1979) and adapted to Spanish by Pérez and Hidalgo (1995), the scale includes 15 items divided into 2 subscales: intrinsic satisfaction (7 items) and extrinsic satisfaction (8 items). All items are rated on a 7-point scale, ranging from 1 (very dissatisfied) to 7 (very satisfied). In our study, we obtained alpha values of .88 for the total scale and of .73 and .86 for the subscales of intrinsic and extrinsic satisfaction, respectively.
Procedure
To obtain the sample, the research team met with the directors and nursing supervisors of the above-mentioned hospitals with a Mental Health Service. The supervisors were requested to hand out the questionnaires randomly, stratifying by categories, and to collect them in a closed, unidentified envelope. A maximum of two weeks was allowed to return the questionnaires, and questionnaires that were not collected by then were considered missing. The professionals’ participation was voluntary, and they were ensured the confidentiality and anonymity of the data collected. They were provided with information about the results after the study was completed.
Data Analysis
The data were statistically analyzed using the SPSS software (version 22.0 for Windows). Firstly, the distribution of the sample was analyzed, and the response percentages were ordered according to the sociodemographic and socio-occupational variables. Subsequently, Student's t-test was used for dichotomic variables, and ANOVA for multi-response variables to analyze the mean score obtained in the HABS-U scale. Tukey's post hoc test was employed with the ANOVAs to establish differences between the different groups. Pearson's correlation was calculated to analyze the correlation between exposure to violence and the scores obtained in the remaining scales. Lastly, to determine possible differences in the frequency of exposure to violence between the different groups of professionals, frequency was categorized as high (daily, weekly, or monthly frequency) or low (trimestral, annual frequency, or never), using Fisher's F as a statistical significance test, with a level of significance of<.05 for all the contrasts.
Results
Table 1 presents the descriptive statistics obtained for the quantitative target variables. It can be seen that the professionals had a mean job tenure in their current post of 87 days, and the mean tenure in the profession as a nurse or an auxiliary nurse was 176 days. Of the sample, 60.5% had a permanent contract versus 39.5% of temporary contracts. Moreover, 61.7% were on a rotating shift, 20.8% worked the morning shift, 2.9% worked the night shift, and 14.6% had another type of shift. The majority of them did not work extra hours per month, or they did so fewer than 10 hours (82.6%), and only 7.3% had another job.
There were significant differences in the scales of physical and non-physical violence as a function of the sociodemographic variables (sex, age, and marital status). The males reported greater exposure to physical violence than the females, t = 3.16, df = 507, p < .05, d = 0.632, and age was significantly negative correlated, r = -.146, p < .01, with non-physical violence in the sense that younger professionals received greater levels of non-physical violence. Regarding marital status, the ANOVA revealed significant differences between the groups of single, married, and divorced or widowed people. The post hoc analysis showed that single professionals were exposed to greater levels of non-physical violence compared with the other two groups (Tukey = 15.26, p < .05, η2 = .606).
With regard to the socio-occupational variables, it was found a negative correlation between the dimension of non-physical violence and tenure in the profession (r = -.09, p < .05), such that greater experience was related to lower risk of suffering verbal violence. Differences were also found between non-physical violence and professional level, t = 2.86, df = 503, p < .01, d = 0.333, with higher levels of violence received by professional nurses than auxiliary nurses. No differences were found in exposure to violence (physical and non-physical) as a function of the type of contract or having carried out continued training activities.
Table 2 shows the Pearson correlations obtained in the above-mentioned hospital wards between the physical and non-physical user violence dimensions of the HABS-U and the scores in the MBI-GS, the OJS, and the frequency of psychological symptomatology of the GHQ-28.
Table 2 Correlations between the Scores of the Variables Measured by the HABS-U, OJS, MBI-GS, and GHQ-28 Scales in Mental Health Service, Emergency Units, Medical Hospitalization, and Maternal-and Child Units.

*p < .05, **p < .01.
The non-physical violence dimension of the HABS-U correlated positively with emotional exhaustion of the MBI-GS (r = .27, p < .01) and with the GHQ-28. Specifically, the subscale of somatic symptoms of the GHQ-28 presented greater significance with non-physical violence (r = .29, p < .001), followed by the depression subscale (r = .25, p < .01), and lastly by anxiety (r = .17, p < .05) and social dysfunction (r = .17, p < .05) subscales. Regarding burnout, non-physical violence also had a negative correlation with the dimension of professional efficacy of the MBI-GS (r = -.18, p < .05), and the physical violence dimension had a negative correlation with intrinsic satisfaction of the OJS (r = -.21, p < .05).
Tables 3 and 4 presents the ANOVA comparing the levels of perceived user violence among the four types of healthcare units studied (Mental Health, Emergency Units, Medical Hospitalization, and Maternal-and-Child Units). The post hoc tests revealed statistically significant differences in the variables non-physical violence (Table 3) and physical violence (Table 4). Specifically, higher levels of physical violence were found in Mental Health and Emergency Units compared to the supposedly low-risk services, and the highest rates of non-physical violence were found in the Emergency Units, followed by Mental Health Units.
Table 3 Descriptive Statistics and ANOVA of Non-Physical User Violence as a Function of Hospital Service.

Tukey = Post hoc analysis among the diverse units.
***p < .001.
η2 = eta squared.
Table 4 Descriptive Statistics and ANOVA of Physical User Violence as a Function of Hospital Service.

Tukey = Post hoc analysis among the diverse units.
***P < .001.
η2 = squared eta.
With regard to the frequency of exposure to violence, both physical and non-physical, these hostile behaviors were found more frequently in Emergency Units, followed by Mental Health Services. Thus, it is observed that anger because of assistance delay is more frequent in Emergency Units than in the other services studied, F = 32.69, df = 515, p < .001, η2 = .690, and also angry grimaces or disdainful looks, F = 19.34, df = 514), p < .001, η2 = .692.
With regard to non-physical violence, the behavior of raising one's voice is more frequent in Emergency Units and Mental Health compared to the low-risk group, F = 30.19, df = 512, p < .001, η2 = .715, as is insulting, F = 24.72, df = 511, p < .001, η2 = .729, displaying a defiant attitude or gesticulating violently, F = 19.29, df = 513, p < .001, η2 = .691, and threatening to attack the staff, F = 20.59, df = 509, p < .001, η2 = .702.
With regard to physical violence, hostile behaviors are displayed more frequently in Mental Health Services. Displaying anger by banging objects or slamming doors, F = 36.18, df = 515, p < .001, η2 = .751, or shoving, jostling, or spitting, F = 28.81, df = 514, p < .001, η2 = .783, occur more often in this service. More intense anger, breaking doors, windows, walls, F = 18.93, df = 514, p < .001, η2 = .799, is also more frequent in the high-risk group.
Discussion
As expected when proposing the working hypotheses, significant differences in the frequency and type of violence among the hospital services studied were found: Mental Health Services, Emergency Units, Medical Hospitalization, and Maternal-and-Child Unit. Our results coincide with those of other studies showing a higher prevalence in Emergency and Psychiatry Units (James et al., 2006; Magnavita & Heponiemi, 2012). The data obtained on the scale of violence among nursing professionals of these units of the public hospitals of the Region of Murcia are higher than those of the other services studied, and non-physical expressions are even more frequent than physical ones. Higher rates of physical violence were found in Mental Health Services, and of non-physical violence in Emergency Units, compared to the other units. Physically violent behaviors such as banging objects or slamming doors, pushing, jostling, or spitting occur to a greater extent in Psychiatry Units. This is amply reported in diverse studies, such as Dack et al.’s (2013), whose meta-analysis concluded that the factors most frequently associated with violent behavior in Psychiatry wards are being male, young, involuntary admittance, diagnosis of schizophrenia, and substance abuse, among others. Furthermore, Magnavita (2014), in a study comparing diverse hospital services, reports that mental health professionals’ risk of suffering physical aggressions is 45 times higher than that of other professionals.
Regarding Emergency Units, our results indicate that the most frequently reported hostile behavior is anger because of assistance delay, followed by angry grimaces and anger due to the lack of information. This coincides with observations of other authors, who report that prolonged waiting times, massification of waiting rooms, lack of security measures, substance consumption, and the presence of mental disease trigger user aggressiveness (Crilly, Chaboyer, & Creedy, 2004; Gacki-Smith et al., 2009). These violent behaviors could be related to the pain and distress of the user, who urgently needs to be attended to at that moment. To this is added the generalization in recent years of the classification of the patients who come to Emergency Units by means of a triage system (Galián-Muñoz, Llor-Esteban, & Ruiz-Hernández, 2014). This method may not be well understood by the users, whose concept of emergency may differ from that of the professional who attends to them (Sánchez-Bermejo et al., 2013). Providing information to the patients with adequate communication techniques about the classification system and the approximate waiting times could decrease the incidence of violent situations (Estryn-Behar et al., 2008). Diverse studies have found that the implementation of training plans for clinical staff, both in Emergency Units and Mental Health Services, considerably reduces the number of user aggressions, minimizes worker stress, and buffers the effect of traumatic incidents (Bjorkdahl, Hansebo, & Palmstierna, 2013; Swain & Gale, 2014).
In our work, gender differences were found with regard to physical violence, which is more frequent in males than in females. This coincides with other studies indicating that males are at greater risk of violence (Landau & Bendalak, 2008; Shields & Wilkins, 2009), possibly because men are less intimidated and feel less fear and, therefore, they expose themselves more frequently to violent behaviors (Jansen, Middel, Dassen, & Menno, 2006). Another possible explanation is related to the role of gender stereotypes in our society. The male has traditionally been considered the protector of the female, and this could make men feel a moral obligation to confront dangerous situations (Young & Sweeting, 2004).
It was also found that younger professionals suffer more non-physical violence, as do professionals with less tenure in the profession. Our findings coincide with those of some authors, who point out as risk factors being younger or having less professional experience (Roche et al., 2010). The users’ perception of a professional's excessive youth may lead them to treat these young professionals less respectfully than older ones. Regarding experience, Jonker, Goossens, Steenhuis, and Oud (2008) note that more experienced nurses are capable of recognizing the first signs of aggressive behavior and of intervening more appropriately, using fewer coercive measures. Regarding marital status, single professionals were exposed to greater levels of non-physical violence compared with the other two groups. This may be related to age, since singles are generally younger than the other groups.
Significant differences were detected in the subscale of non-physical violence between nurses and auxiliary nursing staff. This variable could be related to the position of authority, indicated by some authors as a risk factor (Landau & Bendalak, 2010). In this sense, Gascón et al. (2009) analyzed professional category as a risk factor, concluding that there is a direct association between the level of responsibility and exposure to non-physical violence, such that doctors and directors were the most exposed personnel.
After reviewing different studies (Franz et al., 2010; Galián-Muñoz et al., 2014), it was confirmed that exposure to violent situations can provoke diverse psychological consequences in health professionals. These can range from decreased job satisfaction and the onset of burnout symptoms to the presence of psychological distress. Our work has detected a higher relation of these indicators with non-physical violence, which is directly related to the dimension of emotional exhaustion of the burnout scale and to the decrease of psychological well-being as measured by the GHQ scale. In this sense, Wittington (2002) found that emotionally exhausted staff had more difficulty understanding the patients’ viewpoint and tolerating aggressive behavior. This can lead to inadequate handling of violent situations and the onset of new aggressions, which in turn cause more emotional exhaustion (Zampieron et al., 2010).
The present work also has some limitations that should be taken into account. On the one hand, the type of design, because it is a retrospective cross-sectional study, which limits the possibility of establishing causal relations among the variables of interest. Moreover, it is based on the participants’ recall of the events, which might not be exact. On the other hand, another limitation is the type of sample used, which focuses on health professionals, specifically nursing staff. It would be interesting to include in future research other professionals from this setting, including non-health workers.
This study allows us to conclude that user violence toward clinical staff is non-physical rather than physical in most cases, and that, as reported in current studies, the areas of Mental Health and Emergency Units are the most affected. Our findings suggest that non-physical violence is more typical of Emergency Units, and physical violence is more frequent in Mental Health Services. Another fact to be taken into account is the person's experience in the position or the profession, because it has been shown to be related to lower rates of violence. Therefore, we think that the implementation of training plans similar to the above-mentioned ones would provide the professionals with the necessary communication skills to manage conflictive situations, which would, in turn, lead to a considerable reduction of the number of aggressions.