Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista de Osteoporosis y Metabolismo Mineral
versión On-line ISSN 2173-2345versión impresa ISSN 1889-836X
Rev Osteoporos Metab Miner vol.9 no.4 Madrid nov./dic. 2017
https://dx.doi.org/10.4321/s1889-836x2017000400002
Originals
Use of drugs for osteoporosis treatment in patients with type 2 diabetes mellitus: population-based cohort study
1 Atención Primaria Barcelona Ciutat - Instituto Catalán de la Salud - Barcelona (España)
2 Grupo de Investigación en Enfermedades Prevalentes del Aparato Locomotor en Atención Primaria (GREMPAL) - Instituto Universitario de Investigación en Atención Primaria (IDIAP) Jordi Gol - Universidad Autónoma de Barcelona - Barcelona (España)
3 Área de Fragilidad y Envejecimiento Saludable del Centro de Investigación Biomédica en Red (CIBERFES) - Instituto de Salud Carlos III (ISCIII) - Madrid (España)
4 Unidad de Endocrinología - Hospital Can Misses - Ibiza (España)
5Servicio de Endocrinología y Nutrición - Hospital Universitario Germans Trias i Pujol - Badalona (España)
6Área de Diabetes y Enfermedades Metabólicas Asociadas del Centro de Investigación Biomédica en Red (CIBERDEM) - Instituto de Salud Carlos III (ISCIII) - Madrid (España)
7 Departamento Medicina Interna - Instituto de Investigaciones Médicas del Hospital del Mar (IMIM) - Universidad Autónoma de Barcelona - Barcelona (España)
8 Departamento de Ortopedia, Reumatología y Ciencias Musculoesqueléticas de Nuffield (NDORMS) - Unidad de Investigación Biomédica Músculoesquelética del Instituto Nacional para la Investigación en Salud (NIHR) - Universidad de Oxford (Reino Unido)
Introduction
Osteoporosis is a disease of bone metabolism characterized by increased bone fragility and fracture propensity. In postmenopausal women, these fractures have been associated with a decrease in bone mineral density (BMD) 1. However, this correlation with low BMD does not occur in all situations; Patients with type 2 diabetes mellitus (DM2) present an increased risk of fractures, especially femoral fractures 2,3,4, despite presenting higher BMD values compared to the non-diabetic population that fracture 5,6.
Different mechanisms have been postulated through which the risk of fracture in the diabetic population could be increased. These include some complications associated with DM2 (hypoglycemia, neuropathy, nephropathy and diabetic retinopathy) 7,8,9,10 and also associated with an increased risk of falls and, consequently, fractures. Also, some antidiabetic drugs, such as sulfonylureas, glitazones and insulin, have been associated with an increased risk of fractures 11,12. An increased risk of fractures has also recently been reported in patients treated with a sodium 2-glucose co-transporter inhibitor type 2 (iSGLT-2), canagliflozin. This has not been observed so far with other iSGLT-2 13,14. Another possible explanation would be the effect of deposition of advanced glycosylation products on bone collagen that may decrease bone strength 15,16,17,18.
Different osteoporosis drugs (OD) are available for the prevention of osteoporotic fractures. These have been analyzed in a multitude of clinical trials, varying their effect depending on the drug, the population studied and the location of the fracture. However, there is little information on these drugs in normal clinical practice, especially in diabetic patients 19,20,21,22.
If patients with T2DM have a higher BMD than non-diabetics and an increased risk of bills, it seems logical to think that the assessment of the real risk of fractures in these patients is underestimated and, consequently, under-treated. Our objective was to determine if there were differences in the prevalence of osteoporosis drugs among patients with DM2 and non-diabetic patients.
Material and methods
Study design:
Population-based retrospective cohort study with data from the Information System for the Development of Primary Care Research (SIDIAP) (www.sidiap.org). The SIDIAP contains the socio-demographic information, clinical records of primary care physicians working at the Catalan Institute of Health (ICS), the main provider of health services in Catalonia, as well as analytical results and pharmacy billing data. It has information of more than 5 million patients (approximately 80% of the Catalan population). The representativeness of SIDIAP over the general population of Catalonia has been previously demonstrated 23. Previous studies carried out with SIDIAP in patients with DM2 observed a prevalence of the disease similar to studies done in other parts of Spain 24,25. Various studies are also available that analyze new predictors of fragility fracture 26,27,28,29,30.
Participants:
There were selected all the subjects of 50 or more years of age by diagnosis of DM2 prevalent or incident between 2006 and 2013, using codes CIE10 (E11.0, E11.1, E11.2, E11.3, E11.4, E11.5, E11.6, E11.7, E11.8 and E11.9). For every person with DM2, two nondiabetic subjects were selected of the same sex, age (± 2 years) and from the same health center. Those subjects with no diagnosed DM2 or type 1 were considered non diabetic and not to receive any anti-diabetic medication before being included.
Study variables:
Data on age, sex and some clinical variables were collected: body mass index (BMI), smoking (smoker, non-smoker and former smoker) and alcohol consumption (measured by units consumed per week and classified as: low-risk consumption, when consumption in men is less than 17 units or in women to 11, moderate consumption, when in men is between 17 and 28 units or in women between 11 and 17, and consumption of risk when in men is Higher than 28 units or in women at 17, as defined in the Program of Preventive Activities and Health Promotion) 31. The presence of ischemic heart disease (stable angina, unstable angina or myocardial infarction) and cerebrovascular disease (cerebral infarction or transient ischemic attack) were evaluated at the time of inclusion, using CIE10 codes. Prevalent fractures were also collected (from any location except face or skull, and fingers or toes). The use of drugs for osteoporosis was grouped into three categories: 1) bisphosphonates (BF), 2) supplements calcium and vitamin D (CaD), and 3) any osteoporosis drug (OD). The Anatomical Therapeutic Chemical Classification (ATC) codes were used for this purpose.
Statistical analysis:
The characteristics of the studied population are described by uni-variate descriptive analysis, calculating the mean and standard deviation for the continuous variables, and the absolute frequency and percentage for the categorical variables. Chi square test was used to compare the prevalence of cardiovascular disease and fractures in both groups. The association between the presence of DM2 and the use of OD was calculated through logistic regression; Was adjusted for the following confounding factors, defined a priori according to available literature and biological plausibility: age, sex, BMI, smoking, alcohol consumption, ischemic heart disease (ICH) or previous cerebrovascular disease (CVD) and previous fractures. All statistical tests were performed with a 95% confidence interval (CI) and assuming a bilateral contrast. The statistical package Stata SE version 12.0 for Mac was used for all analyzes.
Ethical considerations:
SIDIAP provided wholly observational data for this study. The SIDIAP data are totally anonymous and identified by an internal code created at the moment of data inclusion, so it is impossible to identify the subjects included. Approval was obtained from the local Clinical Research Ethics Committee (CEIC IDIAP Jordi Gol), code P15/150.
Results
We identified 166,106 patients diagnosed with DM2 prevalent or incident between 2006 and 2013, and were matched with 332,212 non-diabetic patients. The baseline characteristics of both cohorts are shown in Table 1. Subjects with DM2 had a higher prevalence of IHD and CVD than non-diabetics. They also had a higher prevalence of previous fractures, in general and by specific locations (Table 2).
Table 1 Baseline characteristics in paired T2D and non-diabetic patients

♀: women; SD: standard deviation; BMI: body mass index; CVD: cerebrovascular disease; IHD: ischemic heart disease.
Table 2 Prevalence of fractures in patients with T2DM and non-diabetic pairs

* Fracture of hip, wrist, forearm, humerus or vertebral.
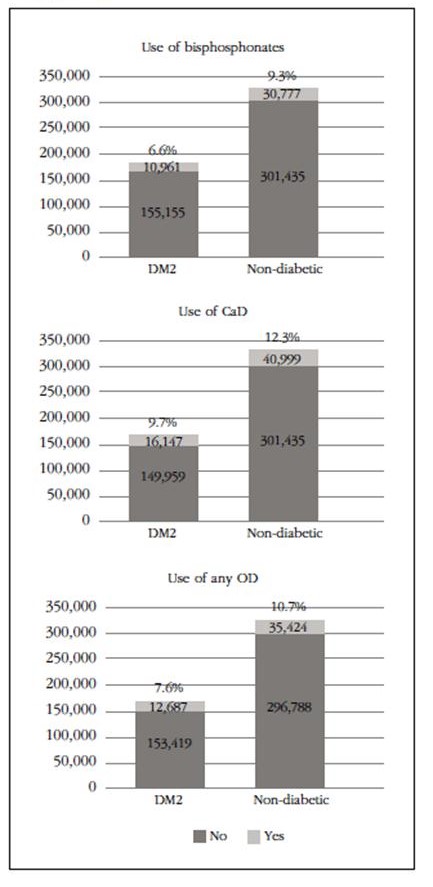
Patients with DM2 presented a lower proportion of drug use for osteoporosis, both BF and any OD and also for CaD, statistically significant (p<0.001 in all three situations) compared to non-diabetic patients (Figure 1).
When analyzing the likelihood of receiving a drug for osteoporosis in subjects with T2DM, compared to non-diabetic subjects, the unadjusted odds ratios were 0.67 (95% CI: 0.65-0.68) for BF, from 0.74 (95% CI: 0.72-0.75) for CaD, and 0.66 (95% CI: 0.65-0.68) for any OD.
After adjusting for age, sex, BMI, smoking, alcohol consumption, previous IC or CVD and previous fractures, subjects with DM2 were less likely to be treated with BF (OR=0.67; 95% CI: 0.64-0.68), with CaD (OR=0.71, 95% CI: 0.70-0.73) or with any OD (OR=0.66, 95% CI: 0.64-0, 67) than non-diabetics.
Discussion
Patients with DM2, despite having a higher prevalence of previous fractures, had more than a 30% probability of not receiving a drug for osteoporosis, compared to non-diabetic subjects. As in previous studies, we observed a higher proportion of fractures in patients with T2DM compared to non-diabetic patients, especially at the femur level, where the prevalence was multiplied by four. These data coincide with two recent meta-analyzes where 30% more risk of femur fracture is described in patients with DM2 3,32.
Paradoxically, even with a higher prevalence of previous fractures, patients with DM2 are less likely to be treated with a bisphosphonate, calcium and vitamin D supplements, or with any osteoporosis drug. One possible explanation for these events could be an underestimation of the risk of fracture in these subjects. Although we do not have data in our BMD cohort, previous studies comparing patients with T2DM with non-diabetic patients observed that the former had a higher BMD 5. Therefore, if the fracture risk assessment is performed exclusively by BMD values, patients with DM2 would be undervalued. Another possibility would be the assessment of fracture risk through the use of tools that allow the calculation of the absolute risk of fracture.
In our area, the most commonly used tool is FRAX®, which does not consider DM2 a risk factor. Different studies 33,34 support the idea of not using FRAX® in patients with DM2, since at the same absolute risk value calculated by FRAX® patients with DM2 present a greater real risk of fractures than non-diabetic patients 35. In an analysis of the Manitoba cohort, it was observed that patients with DM2 had a higher proportion of observed fractures than expected, both main and femoral fractures, a fact that did not occur in non-diabetic subjects 36. A third plausible explanation would be that patients with DM2 receive more drugs than non-diabetics, and this could condition the clinician when prescribing a drug for osteoporosis. Although we do not have the number of drugs that our patients received on average, other studies carried out on patients with DM2 from the SIDIAP database 37 describe medication costing almost double compared to non-diabetic patients and, consequently, a greater number of drugs.
As expected, the DM2 patients in our cohort had a higher prevalence of IHD and CVD than nondiabetic patients, almost double. Some authors suggest that there is a relationship between cardiovascular disease and bone metabolism. A case-control study in subjects with metabolic syndrome observed that patients with a coronary event in the last six months had a higher prevalence of vertebral fracture and of any location compared to subjects who had not had a coronary event 38.
One of the limitations of our study is that the data come from the computerized medical history and, unlike the classic cohort studies, there is no case-by-case validation of each fracture. Previous studies have validated SIDIAP data compared to classic cohort studies and hospital discharge databases, with a moderate sensitivity (close to 70%) and high specificity (>95%) 39. In addition, the ICD-10 coding does not distinguish between trauma fractures and fragility fractures. A recent validation of a sample of more than 300 fractures recorded in patients >50 years of age on the basis of SIDIAP found that more than 90% of femur fractures, more than 87% of vertebral fractures and more than 80% of fractures The main ones were due to fragility (not related to trauma) 40, which gives greater validity to our data. Another possible limitation is that the data in relation to the prescription are collected from the billing data to Pharmacy, in such a way that there may be a stated prescription not withdrawn at the pharmacy and, therefore, not considered. But this fact would occur in both cases in both DM2 and non-diabetic patients.
In contrast, this study has important strengths such as the high number of individuals included, which allows for the detection of statistically significant differences that in other cohort studies with a smaller sample size would not have been detected.
We consider necessary the search for tools that provide a better estimate of the risk of fractures in patients with DM2. One possibility could be to incorporate DM2 as a risk factor in FRAX® or to have a specific tool for patients with DM2 that takes into account both classic and DM2 risk factors. Another option would be the incorporation of new techniques, such as micro-indentation, which allow the assessment of fracture risk independently of BMD 41,42.
Conclusions
Patients with DM2 are about 30% more likely to not receive bisphosphonate, calcium and vitamin D supplements or any osteoporosis drug than non-diabetic patients. We believe that this lower probability of being treated is due to an underestimation of the real risk of fracture in patients with T2DM, which justifies the need for a specific tool for the estimation of fracture risk in these patients.
received an Italfarmaco award for the best Oral Communication of the Congress of SEIOMM 2016 held in Gran Canaria, Spain.
REFERENCES
1. Siris ES, Miller PD, Barrett-Connor E, Faulkner KG, Wehren LE, Abbott TA, et al. Identification and fracture outcomes of undiagnosed low bone mineral density in postmenopausal women: results from the National Osteoporosis Risk Assessment. JAMA. 2001;286:2815-22. [ Links ]
2. Janghorbani M, Van Dam RM, Willett WC, Hu FB. Systematic review of type 1 and type 2 diabetes mellitus and risk of fracture. Am J Epidemiol. 2007;166:495-505. [ Links ]
3. Dytfeld J, Michalak M. Type 2 diabetes and risk of low-energy fractures in postmenopausal women: meta-analysis of observational studies. Aging Clin Exp Res. 2017;29(2):301-9. [ Links ]
4. Fan Y, Wei F, Lang Y, Liu Y. Diabetes mellitus and risk of hip fractures: a meta-analysis. Osteoporos Int. 2016;27:219-28. [ Links ]
5. Vestergaard P. Discrepancies in bone mineral density and fracture risk in patients with type 1 and type 2 diabetes--a meta-analysis. Osteoporos Int. 2007;18:427-44. [ Links ]
6. Ma L, Oei L, Jiang L, Estrada K, Chen H, Wang Z, et al. Association between bone mineral density and type 2 diabetes mellitus: A meta-Analysis of observational studies. Eur J Epidemiol. 2012;27:319-32. [ Links ]
7. Johnston SS, Conner C, Aagren M, Ruiz K, Bouchard J. Association between hypoglycaemic events and fall-related fractures in Medicare-covered patients with type 2 diabetes. Diabetes Obes Metab. 2012;14:634-43. [ Links ]
8. Barzilay JI, Buzkova P, Chen Z, de Boer IH, Carbone L, Rassouli NN, et al. Albuminuria is associated with hip fracture risk in older adults: the cardiovascular health study. Osteoporos Int. 2013;24:2993-3000. [ Links ]
9. Ivers RQ, Cumming RG, Mitchell P, Peduto AJ. Diabetes and risk of fracture: The Blue Mountains Eye Study. Diabetes Care. 2001;24:1198-203. [ Links ]
10. Rasul S, Ilhan A, Wagner L, Luger A, Kautzky-Willer A. Diabetic polyneuropathy relates to bone metabolism and markers of bone turnover in elderly patients with type 2 diabetes: greater effects in male patients. Gend Med. 2012;9:187-96. [ Links ]
11. Zhu Z-N, Jiang Y-F, Ding T. Risk of fracture with thiazolidinediones: An updated meta-analysis of randomized clinical trials. Bone. 2014;68:115-23. [ Links ]
12. Majumdar SR, Josse RG, Lin M, Eurich DT. Does sitagliptin affect the rate of osteoporotic fractures in type 2 diabetes? population-based cohort study. J Clin Endocrinol Metab. 2016;101:1963-9. [ Links ]
13. Watts NB, Bilezikian JP, Usiskin K, Edwards R, Desai M, Law G, et al. Effects of canagliflozin on fracture risk in patients with type 2 diabetes mellitus. J Clin Endocrinol Metab. 2016;101:157-66. [ Links ]
14. Ljunggren Ö, Bolinder J, Johansson L, Wilding J, Langkilde AM, Sjöström CD, et al. Dapagliflozin has no effect on markers of bone formation and resorption or bone mineral density in patients with inadequately controlled type 2 diabetes mellitus on metformin. Diabetes Obes Metab. 2012;14:990-9. [ Links ]
15. Miyata T, Notoya K, Yoshida K, Horie K, Maeda K, Kurokawa K, et al. Advanced glycation end products enhance osteoclast-induced bone resorption in cultured mouse unfractionated bone cells and in rats implanted subcutaneously with devitalized bone particles. J Am Soc Nephrol. 1997;8:260-70. [ Links ]
16. Jehle PM, Jehle DR, Mohan S, Böhm BO. Serum levels of insulin-like growth factor system components and relationship to bone metabolism in Type 1 and Type 2 diabetes mellitus patients. J Endocrinol. 1998;159:297-306. [ Links ]
17. Takagi M, Kasayama S, Yamamoto T, Motomura T, Hashimoto K, Yamamoto H, et al. Advanced glycation endproducts stimulate interleukin-6 production by human bone-derived cells. J Bone Miner Res. 1997;12:439-46. [ Links ]
18. Yamamoto M, Yamaguchi T, Yamauchi M, Yano S, Sugimoto T. Serum pentosidine levels are positively associated with the presence of vertebral fractures in postmenopausal women with type 2 diabetes. J Clin Endocrinol Metab. 2008;93:1013-9. [ Links ]
19. Vestergaard P, Rejnmark L, Mosekilde L. Are antiresorptive drugs effective against fractures in patients with diabetes? Calcif Tissue Int. 2011;88:209-14. [ Links ]
20. Johnell O, Kanis JA, Black DM, Balogh A, Poor G, Sarkar S, et al. Associations between baseline risk factors and vertebral fracture risk in the Multiple Outcomes of Raloxifene Evaluation (MORE) Study. J Bone Miner Res. 2004;19:764-72. [ Links ]
21. Ensrud KE, Stock JL, Barrett-Connor E, Grady D, Mosca L, Khaw K-T, et al. Effects of raloxifene on fracture risk in postmenopausal women: the Raloxifene Use for the Heart Trial. J Bone Miner Res. 2008;23:112-20. [ Links ]
22. Schwartz AV, Pavo I, Alam J, Disch DP, Schuster D, Harris JM, et al. Teriparatide in patients with osteoporosis and type 2 diabetes. Bone. 2016;91:152-8. [ Links ]
23. García-Gil MM, Hermosilla E, Prieto-Alhambra D, Fina F, Rosell M, Ramos R, et al. Construction and validation of a scoring system for the selection of high-quality data in a Spanish population primary care database (SIDIAP). Inform Prim Care. 2011;19:135-45. [ Links ]
24. Vinagre I, Mata-Cases M, Hermosilla E, Morros R, Fina F, Rosell M, et al. Control of glycemia and cardiovascular risk factors in patients with type 2 diabetes in primary care in Catalonia (Spain). Diabetes Care. 2012;35:774-9. [ Links ]
25. Mata-Cases M, Franch-Nadal J, Real J, Mauricio D. Glycaemic control and antidiabetic treatment trends in primary care centres in patients with type 2 diabetes mellitus during 2007-2013 in Catalonia: a population-based study. BMJ Open. 2016;6(10):e012463. [ Links ]
26. Prieto-Alhambra D, Premaor MO, Fina Avilés F, Hermosilla E, Martinez-Laguna D, Carbonell-Abella C, et al. The association between fracture and obesity is site-dependent: a population-based study in postmenopausal women. J Bone Miner Res. 2012;27:294-300. [ Links ]
27. Prieto-Alhambra D, Premaor MO, Avilés FF, Castro AS, Javaid MK, Nogués X, et al. Relationship between mortality and BMI after fracture: a population-based study of men and women aged =40 years. J Bone Miner Res. 2014;29:1737-44. [ Links ]
28. Reyes C, Pottegård A, Schwarz P, Javaid MK, Van Staa TP, Cooper C, et al. Real-Life and RCT Participants: Alendronate Users Versus FITs' Trial Eligibility Criterion. Calcif Tissue Int. 2016;99:243-9. [ Links ]
29. Reyes C, García-Gil M, Elorza JM, Fina-Avilés F, Mendez-Boo L, Hermosilla E, et al. Socioeconomic status and its association with the risk of developing hip fractures: A region-wide ecological study. Bone. 2015;73:127-31. [ Links ]
30. Güerri-Fernandez R, Vestergaard P, Carbonell C, Knobel H, Avilés FF, Castro AS, et al. HIV infection is strongly associated with hip fracture risk, independently of age, gender, and comorbidities: a population-based cohort study. J Bone Miner Res. 2013;28:1259-63. [ Links ]
31. Córdoba García R, Camarelles Guillem F, Muñoz Seco E, Gómez Puente JM, Ramírez Manent JI, José Arango JS, et al. Recomendaciones sobre el estilo de vida. Aten Primaria. 2016;48(Suppl 1):27-38. [ Links ]
32. Fan Y, Wei F, Lang Y, Liu Y. Diabetes mellitus and risk of hip fractures: a meta-analysis. Osteoporos Int. 2016;27:219-28. [ Links ]
33. Bridges MJ, Ruddick S a. Do FRAX/NOGG guidelines predict fractures in post-menopausal women with Type 2 diabetes? Diabet Med. 2012;29:555-6. [ Links ]
34. Carnevale V, Morano S, Fontana A, Annese MA, Fallarino M, Filardi T, et al. Assessment of fracture risk by the FRAX algorithm in men and women with and without type 2 diabetes mellitus: a cross-sectional study. Diabetes Metab Res Rev. 2014;30:313-22. [ Links ]
35. Schwartz A V, Vittinghoff E, Bauer DC, Hillier TA, Strotmeyer ES, Ensrud KE, et al. Association of BMD and FRAX score with risk of fracture in older adults with type 2 diabetes. JAMA. 2011;305:2184-92. [ Links ]
36. Giangregorio LM, Leslie WD, Lix LM, Johansson H, Oden A, McCloskey E, et al. FRAX underestimates fracture risk in patients with diabetes. J Bone Miner Res. 2012;27:301-8. [ Links ]
37. Mata-Cases M, Casajuana M, Franch-Nadal J, Casellas A, Castell C, Vinagre I, et al. Direct medical costs attributable to type 2 diabetes mellitus: a population-based study in Catalonia, Spain. Eur J Health Econ. 2016;17:1001-10. [ Links ]
38. Silva HC, Pinheiro MM, Genaro PS, Castro CHM, Monteiro CMC, Fonseca FAH, et al. Higher prevalence of morphometric vertebral fractures in patients with recent coronary events independently of BMD measurements. Bone. 2013;52:562-7. [ Links ]
39. Pagès-Castellà A, Carbonell-Abella C, Avilés FF, Alzamora M, Baena-Díez JM, Laguna DM, et al. Burden of osteoporotic fractures in primary health care in Catalonia (Spain): a population-based study. BMC Musculoskelet Disord. 2012;13:79. [ Links ]
40. Martinez-Laguna D, Soria-Castro A, Carbonell-Abella C, Orozco P, Estrada-Laza P, Nogues X, et al. P172 Validation of fragility fractures in primary care electronic medical records: a population-based study. Osteoporos Int. 2016;27:79-548. [ Links ]
41. Farr JN, Drake MT, Amin S, Melton LJ, McCready LK, Khosla S. In vivo assessment of bone quality in postmenopausal women with type 2 diabetes. J Bone Miner Res. 2014;29:787-95. [ Links ]
42. Nilsson AG, Sundh D, Johansson L, Nilsson M, Mellström D, Rudäng R, et al. Type 2 diabetes mellitus is associated with better bone microarchitecture but lower bone material strength and poorer physical function in elderly women: a population-based study. J Bone Miner Res 2017;32:1062-71. [ Links ]
Received: March 20, 2017; Accepted: May 21, 2017











 texto en
texto en