My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista de Osteoporosis y Metabolismo Mineral
On-line version ISSN 2173-2345Print version ISSN 1889-836X
Rev Osteoporos Metab Miner vol.13 n.2 Madrid Jun. 2021 Epub Aug 16, 2021
https://dx.doi.org/10.4321/s1889-836x2021000200002
ORIGINALS
Impact of dementia on the survival of patients with hip fracture after undergoing total and partial prosthesis
1Orthopedic Surgery and Traumatology Service, Alto Deba Hospital. Mondragon (Spain)
2Biodonostia Health Research Institute. San Sebastian (Spain)
3Research Unit, Alto Deba Hospital. Mondragon (Spain)
4Kronikgune Health Services Research Institute, Baracaldo (Spain)
5Research Network in Health Services in Chronic Diseases (REDISSEC). Bilbao (Spain)
6Department of Orthopedic Surgery and Traumatology, University Hospital Doce de Octubre. Madrid (Spain)
Objetive
To carry out a comparative survival analysis of patients diagnosed with hip fractures (HF) in the Basque Health Service from 2010 to 2016 depending on whether or not they were diagnosed with dementia and the type of arthroplasty.
Material and methods
Observational study (real world data) of survival. The data were obtained from the administrative and clinical databases of the Basque Health Service using the Oracle Business Intelligence (OBI) manager. All cases of femur neck fractures from 2010 to 2016 were analyzed in the Basque Health Service. A descriptive analysis was carried out to detect differences between groups according to previous diagnosis of dementia and type of prosthesis. The Kaplan-Meier method was used to obtain the survival curves and their comparison was made in pairs using the Achievement test. The adjusted risk of death for each group was analyzed with the Cox regression model.
Results
5,867 patients with CF were identified, being 1,131 patients without dementia and total prosthesis, 3,073 without dementia and partial prosthesis, 176 with dementia and total prosthesis and 1,487 with dementia and partial prosthesis. The median survival was 9.08 years, 3.79 years, 2.55 years, and 2.54 years respectively. The comparison of the survival curves was significant for all cases except between the last two groups. Using the first group as a reference, the odds ratio of death for the rest was 1.56, 2.27 and 2.37 respectively. When analyzing the risk of death only for patients with dementia, the type of prosthesis was not statistically significant.
Conclusions
Dementia influences the survival curve of patients who undergo arthroplasty after a femur neck fracture, with those who undergo a total arthroplasty have a similar mortality rate as those who undergo partial arthroplasty.
Key words dementia; hip fractura; arthroplasty; Cox regression
INTRODUCTION
Hip fractures represent a general public health problem due to their high incidence and their impact on mortality and loss of quality of life1. In the coming years, with the progressive aging of the population, its incidence is expected to increase, incurring a significant drain on resources2. Crude mortality figures after a hip fracture are considered in most studies. An estimated 5% of patients die in-hospital and approximately 20% do so during the first year, depending on the series3. However, hip fractures occur in elderly patients who have an associated comorbidity that also influences their survival4. The highest mortality rates are reported mainly in the elderly, sick or disabled populations5. A recent meta-analysis exploring the magnitude and duration of the excess risk of mortality after hip fracture found the highest risk in the first 3 months after the fracture, and mortality remained high even after 10 years6. Excess risk increases with age and, at any age, is higher for men than for women6.
Dementia affected 6.53% of the Spanish population over 60 years of age in 20207. The current prevalence worldwide is more than 40 million patients, which will double every 20 years8,9. Patients with dementia have an increased risk of suffering a hip fracture and also evolve significantly worse than patients without it due to higher mortality3. They tend to be patients with an increased risk of hip fracture due to their older age, significant comorbidities, polypharmacy, limited mobility, and a tendency to fall4,10. Treatment options for hip fracture in general include total prosthesis, partial prosthesis, osteosynthesis and conservative treatment without surgery, but in patients with dementia the results are usually worse, with a higher rate of postoperative complications and medium term5, so the choice of treatment should be based on these clinical considerations.
Our study aimed to analyze the comparative survival of patients diagnosed with hip fractures (HF) who underwent arthroplasty in the Basque Health Service from 2010 to 2016 depending on whether or not they were diagnosed with dementia and the type of joint replacement, total and partial.
MATERIAL AND METHODS
Design
A retrospective and observational study (real world data) was carried out on the survival of hip fracture cases registered in the Basque Health Service (SVS). The necessary data were obtained anonymized from the SVS administrative and clinical databases using the Oracle Business Intelligence (OBI) manager. The electronic medical record is fully implemented in the public health system of the Basque Country and associated with administrative data of the patient. This allows each of the contacts and all the use of resources of the patients with the health system to be registered. The clinical research ethics committee of the Basque Country approved the study protocol on February 14, 2019 with registration number PI2019010. Informed consent is not required as the database is anonymized.
Patient sample and variables
All cases of femoral neck fractures operated on by partial or total prosthesis from 2010 to 2016 were analyzed in the Basque Health Service. The diagnosis of femoral neck fracture included ICD-9 codes 820.0 and ICD-10 codes S72.0. The surgical procedures included the ICD-9-CM codes 81.51 for the total prosthesis and 81.52 for the partial one. Within this population, patients with a previous diagnosis of dementia were identified both at the primary care level, as well as at the level of hospital care, emergencies, home care or hospitalization and / or outpatient specialist consultations with a validated procedure11. Diagnosis of dementia included ICD9-MC codes 290, 294.1, and 331, as well as ICD10 codes F01.5, F02.8, F03.9, F05, G30, and G31. The identification of dementia also included the prescription of specific drugs for Alzheimer's disease identified with the ATC code N06D. The final date of follow-up was set at October 31, 2020. The following variables were obtained for each patient: age, sex, risk index from the American Society of Anesthesiologists (ASA), diagnosis and date of dementia, diagnosis and date of hip fracture, type of prosthesis, vital status at the end of follow-up and date of death in such cases. The ASA risk index was used as an adjustment co-variate for the presence of comorbidities and appears in the database as assigned by the anesthetist responsible for the intervention.
Statistic analysis
Statistic analysis was carried out using the R statistics program (version 3.3.2) with a confidence level of 95%. First, a univariate descriptive analysis was performed to detect differences between groups according to a previous diagnosis of dementia. Fisher's exact test was applied for categorical variables of two categories and expected value less than or equal to 5. In the case of continuous variables with normal distribution, the comparison of means was carried out using the Student's t test.
Subsequently, a survival analysis was carried out that included the non-parametric methods of Kaplan-Meier and Cox to compare survival adjusted for previous diagnosis of dementia and type of prosthesis. Four groups were differentiated: 1) patients without dementia and total prosthesis, 2) patients without dementia and partial prosthesis, 3) patients with dementia and total prosthesis, and 4) patients with dementia and partial prosthesis. For each group, the survival functions and curves were calculated using the Kaplan-Meier method, which calculates the cumulative survival ratio at the individual level of each patient. For the comparison of the survival curves, the Mantel-Cox test, also known as the achievement test, was used. The survival curves were compared in pairs. Using Cox regression, the risk of death was analyzed as a function of time, adjusting for age, sex, ASA risk and group (defined based on the previous diagnosis of dementia and type of prosthesis). This calculation was repeated exclusively for the subgroup of patients with dementia, adjusting this time for age, sex, ASA risk index and type of prosthesis.
RESULTS
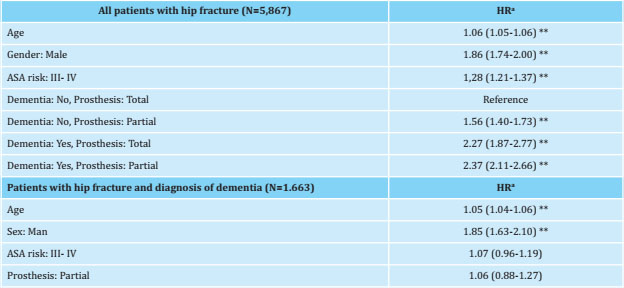
Between 2010 and 2016, 5,867 patients diagnosed with a femoral neck fracture were identified, of which 1,663 had a previous diagnosis of dementia. As can be seen in table 1, the mean follow-up was 2.98 years for patients with dementia and 4.29 years for patients without dementia, while the mean age was 84.71 years and 81.91 years respectively. In the univariate analysis, significant differences were observed by age, sex, ASA risk and type of prosthesis. In the group of patients with dementia, there was a higher percentage of partial dentures, as well as a higher ASA risk. There were also significant differences in the mortality rate, since it was higher in the group of patients with a previous diagnosis of dementia (82.4%) than in the rest (63.5%).
Figures 1 and 2 show the survival curves obtained using the Kaplan-Meier method, the first being differentiated only by a previous diagnosis of dementia and the second by a previous diagnosis of dementia and type of prosthesis. Of the 5,867 patients in the total sample, 1,131 were patients without dementia and with total prosthesis, 3,073 patients without dementia and with partial prosthesis, 176 patients with dementia and total prosthesis, and 1,487 patients with dementia and partial prosthesis. The follow-up that indicated the probability of survival at 50% for each subgroup was 9.08 years, 3.79 years, 2.55 years and 2.54 years respectively (Table 2 and Figure 2). Table 3 shows the log-rank test that compared the survival curves of the four groups. Significant differences were observed between the curves of all groups, except between the curve of the group of patients with dementia and total prosthesis and the curve of the group of patients with dementia and partial prosthesis.
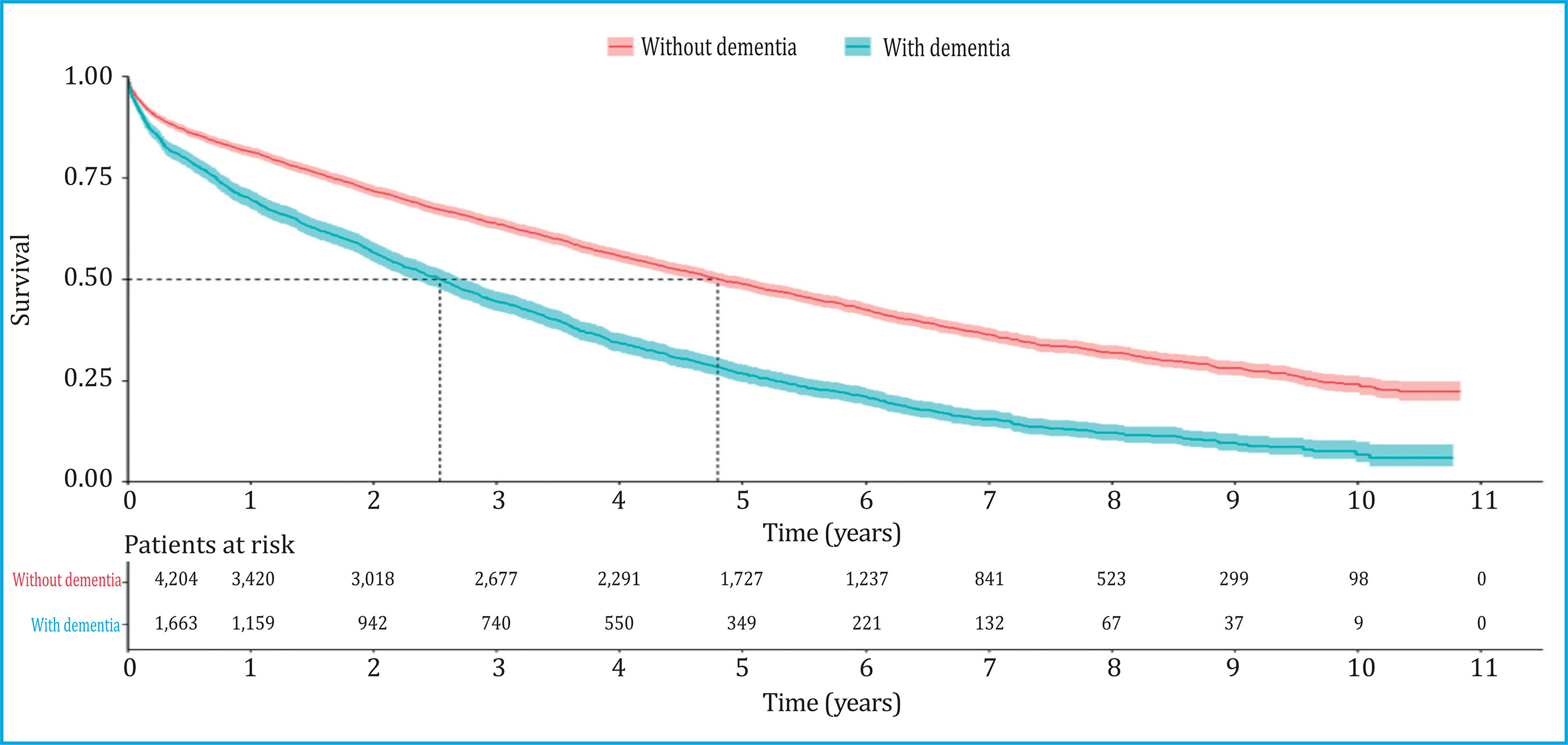
Figure 1. Survival curves of patients with hip fracture differentiated by previous diagnosis of dementia
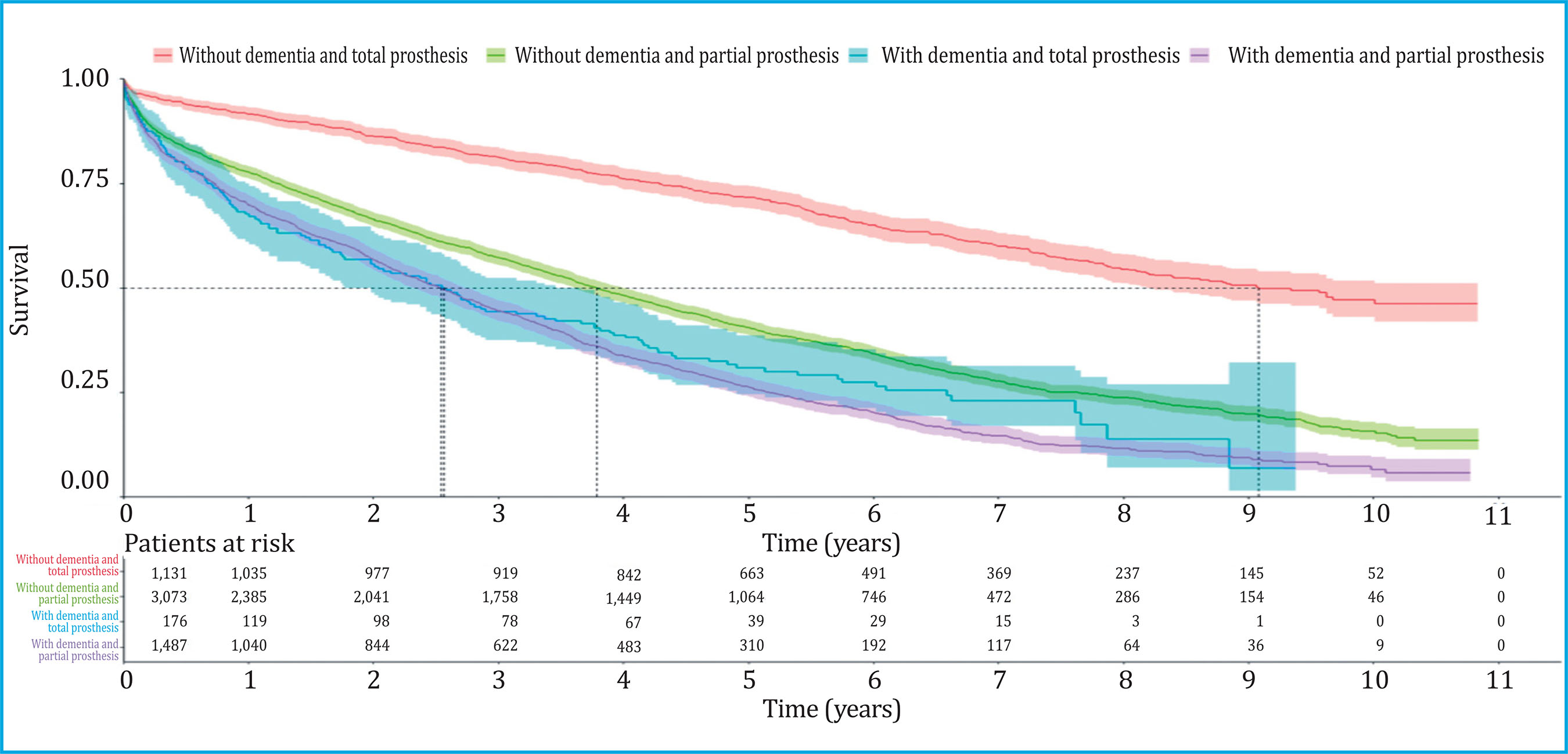
Figure 2. Survival curves of patients with hip fracture differentiated by previous diagnosis of dementia and type of prosthesis
Table 1. Univariate statistical analysis of the baseline characteristics of patients with hip fracture differentiated by a previous diagnosis of dementia
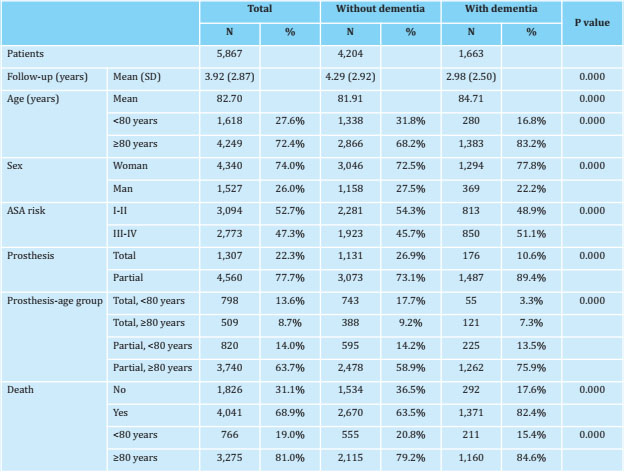
a Fisher's exact test was used for categorical variables and Student's t test for continuous variables; SD: standard deviation.
Table 2. Follow-up indicating the 50% probability of survival for each group and differentiated by previous diagnosis of dementia and type of prosthesis according to the Kaplan-Meyer analysis
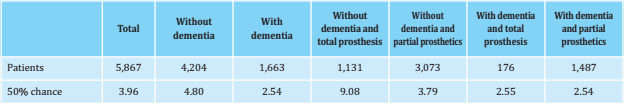
Table 3. Pairwise comparison of the survival curves of patients with hip fracture differentiated by previous diagnosis of dementia and type of prosthesis
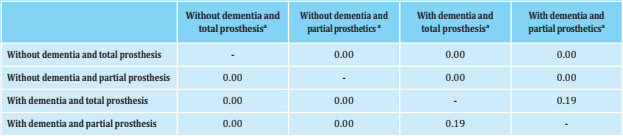
a Log rank test compared the survival curves of the four groups.
Table 4 shows the results of the two Cox regressions performed in the form of hazard ratios and significance. In the first Cox model, developed for all patients with hip fracture, age, sex, ASA risk, and group, according to dementia diagnosis and type of prosthesis, were found to be statistically significant. The risk was higher the older, in men and in patients with worse ASA. Regarding the group, the group of patients without dementia and full prosthesis was used as a reference and it was observed that the risk was 1.56 times higher for the group without dementia and partial prosthesis, 2.27 times higher for the group with dementia and total prosthesis and 2.37 times greater for the group with dementia and partial prosthesis. However, when performing the second Cox model only for patients with dementia, the ASA risk and the type of prosthesis were not statistically significant.
DISCUSSION
Two findings stand out as the main results of our study. First, the previous diagnosis of dementia in patients who have suffered a hip fracture determines a great reduction in their life expectancy. Second, in patients with dementia, the type of prosthesis does not modify survival. These data are consistent with the clinical recommendations for the indication of a total hip arthroplasty as it is reserved for those patients with greater functional capacity, less comorbidity and high life expectancy12.
Three treatment options for hip fractures are conservative without surgery, osteosynthesis of the fracture or different types of prostheses. In our series, only patients with displaced femoral neck fracture were included, those who are treated by arthroplasty, either partial or total, and in whose indication for a surgical procedure life expectancy plays a key role. Hip fractures without surgery were not included because the clinical interest of the survival analysis is due to the fact that it is a criterion for deciding the type of surgical procedure or the patients with fractures in the trochanteric area in whom the surgical management is different. Partial arthroplasty, preferably cemented, is the most indicated option for those patients with a limited life expectancy, with poorer function and mobility, or with cognitive alterations13. In recent years there has been an increase in the use of total arthroplasty for the surgical treatment of femoral neck fractures13, but an analysis of results from the clinical and also the economic point of view is necessary to know in what type of patients its use is more efficient. Total arthroplasty is more expensive, requires a longer surgery time, is more aggressive for the patient and with a higher probability of postoperative anemia and the need for transfusions. In addition, we should bear in mind that patients with dementia have a higher risk of prosthetic dislocation and periprosthetic fracture14. In our sample, only 176 patients with dementia underwent total arthroplasty. Although it has been a small number, our results indicate that it is not the most appropriate option given that these patients' mortality is similar to that of patients who received a partial prosthesis. If the surgeon considers a total arthroplasty, the so-called double mobility prosthesis, should be indicated, the risk of dislocation is significantly reduced15.
Hip fracture, in turn, can also be a risk factor for developing dementia. The main cause lies in the delirium that some of these patients experience during the postoperative period, which is estimated to increase the risk of developing dementia by up to 15 times in the 3 years after the fracture16. In addition, other factors have been related, such as the inflammatory response during the fracture consolidation process, the alteration of motor function and a decrease in physical activity after it, and the medication they receive during the process - before, during and after surgery- which could influence cognitive impairment17.
Our results, referring to patients operated on with prostheses, are consistent with those described in the literature. A clear decrease in survival in patients with hip fracture in general were reportedly diagnosed with dementia. This is considered an independent risk factor for mortality after a hip fracture, since it behaves like the worst of the concomitant diseases18, worsening functional recovery and vital prognosis. The reasons may be that these patients have more limitations in following postoperative instructions, more difficulties in exercising rehabilitation and a higher risk of malnutrition19. Mortality is also influenced by age, male sex, medical comorbidities (which may delay surgery), anesthetic risk, and functional status before the fracture. Dementia also increases the risk of suffering respiratory and urinary infections and more tendency to sepsis20. Some studies report an increase in mortality at one month21,22, at 6 months22,23, at one year19,22 and with longer follow-ups22 after the fracture. Ortho-geriatric functional recovery programs are beneficial in the acute phase, reducing mortality and institutionalization, although it is not clear which is the most appropriate approach24.
Regarding these patients' treatment, the fact that on many occasions they present a high number of comorbidities and that the greater the clinical complexity, the worse the results25, makes it possible to consider the surgery that is as less invasive as possible, for example with a simple osteosynthesis of the fracture or even, with surgical abstention. However, this extreme does not seem advisable since without surgery, mortality doubles at 6 months26, along with increasing complications such as pressure ulcers and pain, which are very limiting and hinder simple care tasks such as hygiene or postural changes.
Our work has some limitations. As previously noted, we only include those patients operated on with a prosthesis, excluding patients with a fracture in the trochanteric region and also those patients who underwent osteosynthesis. However, the profile of the patient who undergoes a total prosthesis for a femur neck fracture is a more active patient with a theoretically longer life perspective, in which dementia plays a relevant role in its evolution. In the same way, we have been able to analyze the number of total arthroplasties in these types of patients, whose indication is debatable and indicates that clinical results such as survival should be measured in order to assess their use. Another limitation is that we do not assess the degree of dementia or the number of falls that patients have, as well as the bone status or the diagnosis of osteoporosis or the antiosteoporotic medication that the patient may receive, although we recognize that they may influence their clinical development.
In conclusion, our study shows how dementia influences the survival curve of patients who underwent arthroplasty after a femoral neck fracture, and that patients with total arthroplasty present a similar mortality rate than patients who underwent partial prosthesis. Thus, we consider the indication of a more aggressive surgery in this type of patient should be avoided.
Funding. The study was funded by the Department of Health of the Basque Government (grant number 2020111021). The funding source did not participate in the study design, in obtaining the data, in the analysis and interpretation of the data, in the writing of the report, nor in the decision to present the article.
Ethics Committee/Animal Experimentation Commission: The Basque Region clinical research ethics committee approved the study protocol on February 14, 2019 with registration number PI2019010. Informed consent is not required as the database is anonymized.
REFERENCES
1 Etxebarria-Foronda I, Arrospide A, Soto-Gordoa M, Caeiro JR, Abecia LC, Mar J. Regional variability in changes in the incidence of hip fracture in the Spanish population (2000-2012). Osteoporos Int. 2015;26(5):1491-1497. [ Links ]
2 Bartra A, Caeiro J-R, Mesa-Ramos M, Etxebarría-Foronda I, Montejo J, Carpintero P, et al. Cost of osteoporotic hip fracture in Spain per Autonomous Region. Rev Esp Cir Ortop Traumatol. 2019;63(1):56-68. [ Links ]
3 Johansson C, Skoog I. A populationbased study on the association between dementia and hip fractures in 85-year olds. Aging (Milano). 1996; 8(3):189-196. [ Links ]
4 Knauf T, Bücking B, Bargello M, Ploch S, Bliemel C, Knobe M, et al. Predictors of long-term survival after hip fractures?-5-year results of a prospective study in Germany. Arch Osteoporos. 2019;14(1):40. [ Links ]
5 Tsuda Y, Yasunaga H, Horiguchi H, Ogawa S, Kawano H, Tanaka S. Association between dementia and postoperative complications after hip fracture surgery in the elderly: analysis of 87,654 patients using a national administrative database. Arch Orthop Trauma Surg. 2015;135(11):1511-1517. [ Links ]
6 Haentjens P, Magaziner J, Colón-Emeric CS, Vanderschueren D, Milisen K, Velkeniers B, et al. Meta-analysis: excess mortality after hip fracture among older women and men. Ann Intern Med. 2010;152(6):380-390. [ Links ]
7 Soto-Gordoa M, Arrospide A, Moreno-Izco F, Martínez-Lage P, Castilla I, Mar J. Projecting Burden of Dementia in Spain, 2010-2050: Impact of Modifying Risk Factors. J Alzheimers Dis. 2015;48(3):721-730. [ Links ]
8 Ferri CP, Prince M, Brayne C, Brodaty H, Fratiglioni L, Ganguli M, et al. Global prevalence of dementia: a Delphi consensus study. Lancet. 2005;366(9503):2112-2117. [ Links ]
9 Mar J, Soto-Gordoa M, Arrospide A, Moreno-Izco F, Martínez-Lage P. Fitting the epidemiology and neuropathology of the early stages of Alzheimer's disease to prevent dementia. Alzheimers Res Ther. 2015;7(1):2. [ Links ]
10 Allan LM, Ballard CG, Rowan EN, Kenny RA. Incidence and prediction of falls in dementia: a prospective study in older people. PLoS One. 2009;4(5): e5521. [ Links ]
11 Mar J, Arrospide A, Soto-Gordoa M, Machón M, Iruin Á, Martinez-Lage P, et al. Validity of a computerized population registry of dementia based on clinical databases. Neurologia. 2018; S0213-4853(18)30090-2. [ Links ]
12 Guyen O. Hemiarthroplasty or total hip arthroplasty in recent femoral neck fractures? Orthop Traumatol Surg Res. 2019;105(1S):S95-101. [ Links ]
13 Stronach BM, Bergin PF, Perez JL, Watson S, Jones LC, McGwin G, et al. The rising use of total hip arthroplasty for femoral neck fractures in the United States. Hip Int. 2020;30(1):107-113. [ Links ]
14 Kristoffersen MH, Dybvik E, Steihaug OM, Kristensen TB, Engesaeter LB, Ranhoff AH, et al. Cognitive impairment influences the risk of reoperation after hip fracture surgery: results of 87,573 operations reported to the Norwegian Hip Fracture Register. Acta Orthop. 2020;91(2):146-151. [ Links ]
15 Iorio R, Iannotti F, Mazza D, Speranza A, Massafra C, Guzzini M, et al. Is dual cup mobility better than hemiarthroplasty in patients with dementia and femoral neck fracture? A randomized controlled trial. SICOT J. 2019;5:38. [ Links ]
16 Olofsson B, Persson M, Bellelli G, Morandi A, Gustafson Y, Stenvall M. Development of dementia in patients with femoral neck fracture who experience postoperative delirium-A three-year follow-up study. Int J Geriatr Psychiatry. 2018;33(4):623-632. [ Links ]
17 Kim SY, Lee JK, Lim J-S, Park B, Choi HG. Increased risk of dementia after distal radius, hip, and spine fractures. Medicine (Baltimore). 2020;99(10):e19048. [ Links ]
18 Brossa Torruella A, Tobías Ferrer J, Garde Garde A, Soler Conde M, Comet Jaumet D, Saavedra Vilchez D. Demencia y fractura de fémur. Rev Esp Geriatr Gerontol. 2007;42(3):135-141. [ Links ]
19 Chiu H-C, Chen C-M, Su T-Y, Chen C-H, Hsieh H-M, Hsieh C-P, et al. Dementia predicted one-year mortality for patients with first hip fracture: a population-based study. Bone Joint J. 2018; 100-B(9):1220-1226. [ Links ]
20 Delgado A, Cordero G-G E, Marcos S, Cordero-Ampuero J. Influence of cognitive impairment on mortality, complications and functional outcome after hip fracture: Dementia as a risk factor for sepsis and urinary infection. Injury. 2020;51 Suppl 1:S19-24. [ Links ]
21 Petersen JD, Siersma VD, Wehberg S, Nielsen CT, Viberg B, Waldorff FB. Clinical management of hip fractures in elderly patients with dementia and postoperative 30-day mortality: A population-based cohort study. Brain Behav. 2020;10(11):e01823. [ Links ]
22 Bai J, Liang Y, Zhang P, Liang X, He J, Wang J, et al. Association between postoperative delirium and mortality in elderly patients undergoing hip fractures surgery: a meta-analysis. Osteoporos Int. 2020;31(2):317-326. [ Links ]
23 Collin C, Bimou C, Mabit C, Tchalla A, Charissoux J-L, Marcheix P-S. Orthogeriatric assessment of patients over 75 years of age with a proximal femur fracture: Predictors of 6-month mortality. Orthop Traumatol Surg Res. 2020;106(7):1441-1447. [ Links ]
24 de Miguel Artal M, Roca Chacón O, Martínez-Alonso M, Serrano Godoy M, Mas Atance J, García Gutiérrez R. [Hip fracture in the elderly patient: Prognostic factors for mortality and functional recovery at one year]. Rev Esp Geriatr Gerontol. 2018;53(5):247-254. [ Links ]
25 Schuetze K, Eickhoff A, Rutetzki K-S, Richter PH, Gebhard F, Ehrnthaller C. Geriatric patients with dementia show increased mortality and lack of functional recovery after hip fracture treated with hemiprosthesis. Eur J Trauma Emerg Surg. 2020 Aug 31. doi: 10.1007/s00068-020-01472-4. Online ahead of print; [ Links ]
26 Berry SD, Rothbaum RR, Kiel DP, Lee Y, Mitchell SL. Association of Clinical Outcomes With Surgical Repair of Hip Fracture vs Nonsurgical Management in Nursing Home Residents With Advanced Dementia. JAMA Intern Med. 2018;178(6):774-780. [ Links ]
Received: January 22, 2021; Accepted: April 13, 2021











 text in
text in