Meu SciELO
Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Revista de Osteoporosis y Metabolismo Mineral
versão On-line ISSN 2173-2345versão impressa ISSN 1889-836X
Rev Osteoporos Metab Miner vol.15 no.3 Madrid Jul./Set. 2023 Epub 08-Mar-2024
https://dx.doi.org/10.20960/revosteoporosmetabminer.00020
ORIGINALS
Should the FRAX tool include other variables to assess fragility-related osteoporotic fractures?
1Bone Metabolism Clinical Management Unit. Hospital Universitario Central de Asturias. Universidad de Oviedo. Institute of Health Research of the Principality of Asturias (ISPA). Oviedo, Spain
2Nephrology Clinical Management Area. Hospital Universitario Central de Asturias. Universidad de Oviedo. Institute of Health Research of the Principality of Asturias (ISPA). Oviedo, Spain
3REDinREN, Carlos III Health Institute (ISCIII). Madrid, Spain
4Internal Medicine Clinical Management Unit. Hospital Universitario Central de Asturias. Universidad de Oviedo. ISPA. Oviedo, Spain
Introduction and objective:
the objective of this study was to assess the significance of variables not included in the FRAX tool regarding the incidence of osteoporotic fractures.
Materials and methods:
a total of 316 women older than 50 years were followed for 8 years. The variables collected (age, BMI, previous fracture, parental history of hip fracture, smoking habit, use of glucocorticoids, femoral neck BMD) and those not collected by the FRAX tool (age at menarche, menopause, fertile years, nulliparity) were studied.
Results:
age and parental history of hip fracture were associated with hip fractures, but so were age at menopause and fertile years. Age [odds ratio (OR), 1.09; 95 % confidence interval (CI), 1.01-1.17] and age at menopause [OR, 0.90; 95 %CI, 0.82-0.99] were associated with hip fractures after the multivariate analysis adjusted for age and BMI. BMI, femoral neck BMD and nulliparity were associated with the occurrence of Colles fractures. According to the multivariate analysis, only nulliparity was associated with Colles fractures [OR, 4.59; 95 %CI, 1.59-13.26)]. Major osteoporotic fractures were significantly associated with parental history of hip fracture, nulliparity, and fertile years. According to the multivariate analysis, the parental history of hip fracture [OR, 3.26; 95 %CI, 1.23-8.61], nulliparity [OR, 3.07; 95 %CI, 1.48-6.37], and fertile years [OR, 0.92; 95 %CI, 0.87-0.98] were associated with the occurrence of major osteoporotic fractures.
Conclusions:
among the FRAX variables, age and parental history of hip fracture were associated with the incidence of major osteoporotic and hip fractures. However, the significance of other gynecological variables was similar, which is indicative that they should certainlay be taken into consideration during patient history assessment.
Keywords: FRAX; Major osteoporotic fracture; Hip fracture; Incidence; Gynecological variables
INTRODUCTION
Despite the availability of a wide therapeutic arsenal and bone densitometry, many patients at risk of fragility-related osteoporotic fractures remain undiagnosed and untreated. Back in 2019, it was estimated that 2,985,000 individuals in our country suffered from osteoporosis (79 % of them, women). Only 36 % of the 1,827,000 women diagnosed with osteoporosis receive treatment, underscoring a treatment gap of 64 % (1). It is estimated that up to 80 % of individuals who have experienced, at one time or another at least, 1 fragility fracture lack proper diagnosis, have not been identified correctly, and consequently, do not receive the necessary diagnosis or subsequent proper management.
The concern surrounding the clinical management of osteoporosis has stimulated the development of procedures to assess the risk of fracture using key risk factors. A group of experts developed a tool called FRAX to identify individuals at higher risk of sustaining fractures within the next 10 years, by combining key factors of risk of fracture and adding bone mineral density (BMD) when available (2). Among fracture-related factors, decreased BMD has been identified as the primary risk factor because of its close relationship with bone strength. Other factors contributing significantly to the risk of fracture have also been identified including family and personal history of fragility fractures, low body weight, smoking, and age, which is known to be one of the most important independent predictors of fracture other than BMD.
However, we should admit that FRAX is not a perfect tool and has been criticized since its inception for not including certain risk factors widely discussed in the medical literature available, such as spine BMD, bone markers, use of benzodiazepines, or history of risk of fall (3-7). Therefore, the objective of this study was to assess if the variables not included in this algorithm, particularly certain gynecological variables, should be included based on the role they play on fragility fractures.
MATERIAL AND METHODS
A total of 316 women older than 50 years were randomized from the Oviedo municipal registry in Oviedo, Asturias, Spain. These women had previously participated in the EVOS study, which was initially designed to determine the prevalence of vertebral fractures across Europe. Also, they were asked to fill out a specifically designed survey for the EVOS study, which exhibited good reproducibility (8,9). This survey included questions on clinical variables such as weight and height to calculate the body mass index (BMI), osteoporosis-related risk factors such as previous fractures, parental history of hip fractures, smoking habits, and use of glucocorticoids for over 3 months. Additionally, other variables were analyzed, such as age at menarche, age at menopause, fertile years, and nulliparity. The femoral neck BMD of this cohort was also established.
This cohort was prospectively followed for 8 years through 4 postal surveys to establish the incidence of non-vertebral osteoporotic fractures during this period. All osteoporotic fractures (hip, Colles, humerus, rib, pelvis, and tibia) excluding skull and limb fractures were confirmed through x-rays, or medical reports. The total number of participants in the final follow-up was 223, with a participation rate of 81.3 % at the 8-year follow-up (excluding deaths). The participation rates for the 3 previous postal follow-ups were 87.1 %, 87.5 %, and 82.4 %, respectively.
DENSITOMETRIC ANALYSIS
The femoral neck BMD was measured using a Hologic® QDR-1000 DXA densitometer (Hologic Inc., Waltham, MA, United States). The coefficient of variation (CV) was 1.9 % (10). Precision and quality control were kept through daily scans using a lumbar spine phantom, resulting in a CV of 0.0 ± 0.1 %.
All studies conducted followed the principles established in the Declaration of Helsinki and received formal approval from the Regional Clinical Research Ethics Committee of the Principality of Asturias, Spain.
STATISTICAL ANALYSIS
Data analysis was conducted using SPSS version 25.0 for Windows. Quantitative variables were analyzed using the Student t test, and the qualitative ones using the chi-square test.
To conduct a multivariate analysis on the impact of multiples risk factors, included or not in FRAX calculations, on the incidence of non-vertebral osteoporotic fractures, logistic regression adjusted for age and BMI was used.
RESULTS
Table I illustrates the baseline clinical characteristics of the variables used by the FRAX tool, as well as other variables not included in this algorithm, such as age at menarche and menopause, fertile years, and nulliparity. The mean age was 65 years and the BMI, 28.6 kg/m². The femoral neck BMD (0.683 g/cm²) fell within the range observed for the Spanish population aged 60-69 years (0.694 g/cm²). The parental history of hip fracture was reported by 7.7 % of participants, and the prevalence of previous non-traumatic fractures was 20 %. Less than 10 % (8.5 %) had used corticosteroids, and 4.7 % of women were smokers. Regarding the gynecological and obstetric variables, notable figures include a mean menarche, menopause, and fertile age of 14, 48.8, and 34.8 years, respectively. Approximately 17.5 % of women had never been pregnant (nulliparity).
The univariate analysis showed that, among the variables used to build the FRAX algorithm, only age and parental history of hip fracture were actually associated significantly with the incidence of hip fracture. However, age at menopause and fertile years were also associated (Table II). We should mention that, among fractured women, no use of corticosteroids or smoking habits were reported. The multivariate analysis adjusted for age and BMI only showed significant associations between age [OR, 1.09; 95 % confidence interval (CI), 1.01-1.17] and age at menopause [OR, 0.90; 95 %CI, 0.82–0.99] with incidental hip fractures.
Table II. Association between clinical variables and the presence or absence of incidental hip fractures.
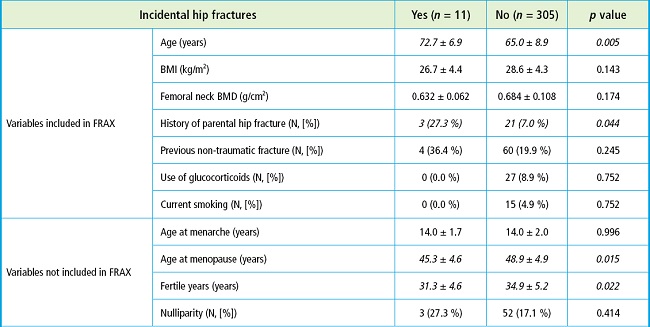
Italicized values indicate significant differences between the two groups.
In the univariate analysis, BMI, femoral neck BMD, and nulliparity were associated with the occurrence of incidental Colles fractures (Table III). According to the multivariate analysis, only nulliparity was associated significantly with the occurrence of Colles fractures [OR, 4.59; 95 %CI, 1.59-13.26)].
Table III. Association between clinical variables and the presence or absence of incidental Colles fractures.
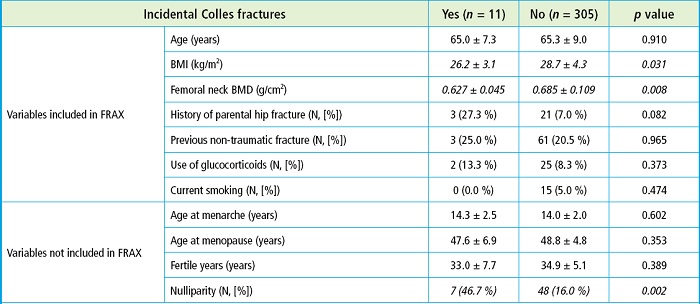
Italicized values indicate significant differences between the two groups.
Regarding the incidence of major osteoporotic fractures, the univariate analysis showed significant associations with the parental history of hip fracture, nulliparity, and fertile years (Table IV). According to the multivariate analysis, the parental history of hip fracture [OR, 3.26, 95 %CI, 1.23-8.61)], nulliparity [OR, 3.07, 95 %CI, 1.48-6.37)], and fertile years [OR, 0.92, 95 %CI, 0.87-0.98)] were associated with the occurrence of incidental major osteoporotic fractures.
DISCUSSION
The results from this study illustrate the significance of some gynecological variables not included in the FRAX algorithm that could carry specific weight. We should mention the significant protective effect of delaying menopause age on the incidence of hip fractures, or the protective effect of fertile years or pregnancy on major osteoporotic fractures.
Undoubtedly, FRAX is a valuable tool to aid clinicians in the identification of individuals needing osteoporosis treatment and those who do not. Also, it is the only algorithm validated across various population cohorts, with or without BMD data, and available in multiple languages. It can equally serve as an inclusion criterion in clinical trial design where fracture is an endpoint. However, it does have well-recognized limitations (11).
Within these limitations, particularly pertinent to this study, is that FRAX has not been validated in Spain (12). Also, FRAX does not include variables that could be challenging for general practitioners to obtain, such as physical activity measurements, vitamin D deficiency, bone turnover markers, or bone loss. Another variable not included is falls despite being a recognized risk factor for non-vertebral fractures, especially hip fractures. Falls are excluded mainly due to the lack of standardized assessment methods. Perhaps this is why gynecological variables were never added to the FRAX algorithm, despite having a specific weight on the occurrence of fragility-related osteoporotic fractures (13). Also, it is possible that the confinement of these variables to women alone may require 2 separate calculators for each gender, which could be operationally cumbersome.
A study of our geographical context showed that not all risk factors included in the FRAX algorithm were significant when fractured and non-fractured women were compared (14). Specifically, age, previous fracture, and baseline osteoporosis were significant. However, excessive alcohol consumption, use of glucocorticoids, rheumatoid arthritis, low BMI, and parental hip fracture history did not show any significance, despite the latter 2 being considered strong or very strong risk factors in FRAX (14). In our case, BMI was associated only with the occurrence of osteoporotic Colles fractures, an association that wasn't found in the multivariate analysis. Similarly, the history of parental hip fracture was associated with the occurrence of hip and major osteoporotic fractures in the univariate models, but only remained significant with major osteoporotic fractures at the multivariate level.
Some authors suggest that the FRAX tool should add gynecological variables, such as menopause, including its onset and duration (15). The findings from our study are not intended to challenge the utility of FRAX. We view FRAX as a highly useful tool to assess individuals at high risk of sustaining fragility fractures. However, clinicians should consider these gynecological variables during the clinical examination of women older than 50 years, in addition to using the FRAX tool, because these variables have shown an association with the incidence of osteoporotic fractures (13,16-20). In our study, regarding hip fractures, delaying menopause by 1 year reduced its incidence by 10 %, which is similar to the 9 % increased risk associated with 1 additional year of aging. Similarly, for major osteoporotic fractures, the parental history of hip fracture was associated with a 3-fold higher risk, which is somewhat similar to the risk associated with nulliparity. Each fertile year cut the risk of major osteoporotic fracture by 8 %.
Our study has several limitations. The survey used to collect osteoporosis risk factor data was interviewer-administered rather than self-administered, which potentially introduces response biases. Some FRAX variables, such as rheumatoid arthritis, secondary osteoporosis, or alcohol consumption, could not be assessed due to the survey design. Another possible, yet inevitable, limitation is the time elapsed between gynecological changes and the study data collection. The study's limited number of incidental osteoporotic fractures and the relatively small cohort size (n = 316) could also be considered limitations.
Despite these limitations, we believe the study has significant strengths. On the one hand, the cohort analyzed participated in the EVOS-EPOS study, being our center one of the 5 centers that completed all the study guidelines. Additionally, the response rate across the 4 postal follow-ups over 8 years exceeded 80 %, strongly supporting the sample's representativeness (21).
In conclusion, some gynecological variables like age at menopause, fertile years, and nulliparity should be considered risk factors for the occurrence of fragility fractures in the patients' medical records. Future studies should clarify whether adding these gynecological variables alongside the FRAX algorithm could enhance the predictive capabilities of this tool widely used in the routine clinical practice.
ACKNOWLEDGEMENTS
This study has received partial funding from the European vertebral osteoporosis study (EVOS), E.U. (1991-1993); the European prospective osteoporosis study (EPOS), E.U. (BIOMED 93-95), the BMHI-CT 092-0182 (1993-1997); the Health Research Fund (FIS 94/1901-E); the Network of Renal Research (REDinREN) of ISCIII (RD06/0016/1013, RD12/0021/0023, RD16/0009/0017, RICORS2040 - Kidney Disease); the National R & D & I Plan 2008-2011, State R & D & I Plan 2013-2016, the European Regional Development Fund (ERDF), the Science, Technology, and Innovation Plan 2013-2017 and 2018-2022 of the Principality of Asturias (GRUPIN14-028, IDI-2018-000152, IDI-2021-000080), and Fundación Renal Iñigo Álvarez de Toledo (FRIAT).
REFERENCES
1. Kanis JA, Norton N, Harvey NC, Jacobson T, Johansson H, Lorentzon M, et al. SCOPE 2021: a new scorecard for osteoporosis in Europe. Arch Osteoporos 2021;16(1):82. DOI:10.1007/s11657-020-00871-9 [ Links ]
2. Kanis JA; on behalf of the World Health Organization Scientific Group. Assessment of Osteoporosis at the Primary Health-Care Level. Technical Report. WHO Collaborating Centre for Metabolic Bone Diseases. University of Sheffield, Sheffield, UK. World Health Organization. Summary Report of a WHO Scientific Group. WHO, Geneva. Available from: www.who.int/chp/topics/rheumatic/en/index.html [ Links ]
3. Díez Pérez A. El debate sobre el FRAX. Rev Osteoporos Metab Miner 2010;2:5-6. [ Links ]
4. Claus-Hermberg H, Bagur A, Messina OD, Negri A L, Schurmann L, Sanchez A. FRAX, un nuevo instrumento para calcular el riesgo absoluto de fracturas a 10 años. Medicina (Buenos Aires) 2009;69:571-5. [ Links ]
5. del Río L, Tebe, C, Johansson H, Gregorio S, Estrada S, Espallargues M. Aplicación del método de evaluación del riesgo absoluto de fractura (FRAX) en población española. Rev Mult Gerontol 2009;19(Supl. 1):17. [ Links ]
6. González Macías J, Marín M, Vila J, Díez Pérez A, Abizanda M, Alvarez R, et al. Prevalencia de factores de riesgo de osteoporosis y fracturas osteoporóticas en una serie de 5.195 mujeres mayores de 65 años. Med Clin (Barc) 2004;123(3):85-9. [ Links ]
7. McGrother CW, Donaldson MMK, Clayton D, Abrams KR, Clarke M. Evaluation of a hip fracture risk store for assessing elderly women: the Melton Osteoporotic Fracture (MOF) study. Osteoporos Int 2002;13:89-96. [ Links ]
8. O'Neill TW, Cooper C, Algra D, Pols HAP, Agnusdei D, Dequeker J;on behalf of the European Vertebral Osteoporosis Study Group. Design and development of a questionnaire for use in a multicentre study of vertebral osteoporosis in Europe: The European vertebral osteoporosis study (EVOS). Rheumatology in Europe 1995;24:75-81. DOI:10.1007/s198-002-8343-6 [ Links ]
9. O'Neill TW, Cooper C, Cannata JB, Diaz Lopez JB, Hoszowski K, Johnell O, et al. Reproducibility of a questionnaire on risk factors for osteoporosis in a multicentre prevalence survey:the European Vertebral Osteoporosis Study. Int J Epidemiol 1994;23:559-65. DOI:10.1093/ije/23.3.559 [ Links ]
10. Naves M, Rodriguez-Garcia M, Diaz-Lopez JB, Gomez-Alonso C, Cannata-Andia JB. Progression of vascular calcifications is associated with greater bone loss and increased bone fractures. Osteoporos Int 2008;19(8):1161-6. DOI:10.1007/s00198-007-0539-1 [ Links ]
11. Silverman SL, Calderon AD. The utility and limitations of FRAX:A US perspective. Curr Osteoporos Rep 2010;8:192-7. DOI:10.1007/s11914-010-0032-1 [ Links ]
12. Azagra Ledesma R, Prieto Alhambra D, Encabo DuróG, Casado Burgos E, AguyéBatista E, Díaz Pérez A;en representación del grupo de estudio FRIDEX. Utilidad de la herramienta FRAX en el tratamiento de la osteoporosis en población femenina española. Med Clin (Barc) 2011;136(14):613-9. DOI:10.1016/j.medcli.2010.09.043 [ Links ]
13. Naves M, Díaz López JB, Gómez C, Rodríguez Rebollar A, Cannata Andía JB. Determinants of incidence of osteoporotic fractures in the female Spanish population older than 50. Osteoporos Int 2005;16(12):2013-7. DOI:10.1007/s00198-005-1983-4 [ Links ]
14. Azagra R, Roca G, Martín Sánchez JC, Casado E, Encabo G, Zwart M, et al. Umbrales de FRAX para identificar personas con alto o bajo riesgo de fractura osteoporótica en población femenina española. Med Clin (Barc) 2015;144(1):1-8. DOI:10.1016/j.medcli.2013.11.014 [ Links ]
15. Minaković I, Zvekić-Svorcan J, Janković T, Vuksanović M, Mikić D, Bošković K. Early menopause and risk of fractures – A preventable gap. Iran J Public Health 2023;52(3):534-41. DOI:10.18502/ijph.v52i3.12136 [ Links ]
16. Pérez Cano R, Galán Galán F, Dilsen G. Risk factors for hip fracture in Spanish and Turkish women. Bone 1993;14(Suppl 1):S69-72. DOI:10.1016/8756-3282(93)90353-C [ Links ]
17. Wang Q, Huang Q, Zeng Y, Liang JJ, Liu SY, Gu X, et al. Parity and osteoporotic fracture risk in postmenopausal women: a dose-response meta-analysis of prospective studies. Osteoporos Int 2016;27(1):319-30. DOI:10.1007/s00198-015-3351-3 [ Links ]
18. Sullivan SD, Lehman A, Nathan NK, Thomson CA, Howardet BV. Age of menopause and fracture risk in postmenopausal women randomized to calcium + vitamin D, hormone therapy, or the combination. Menopause 2017;24(4):371-8. DOI:10.1097/GME.0000000000000775 [ Links ]
19. Anagnostis P, Siolos P, Gkekas NK, Kosmidou N, Artzouchaltzi AM, Christou K, et al. Association between age at menopause and fracture risk: a systematic review and meta-analysis. Endocrine 2019;63(2):213-24. DOI:10.1007/s12020-018-1746-6 [ Links ]
20. Yoo JE, Shin DW, Han K, Kim D, Yoon JW, Lee DY. Association of female reproductive factors with incidence of fracture among postmenopausal women in Korea. JAMA Netw Open 2021;4(1):e2030405. DOI:10.1001/jamanetworkopen.2020.30405 [ Links ]
21. Rodríguez-García M, Gómez-Alonso C, Rodríguez-Rebollar A, Palomo-Antequera C, Martín-Vírgala J, Martín-Carro B, et al. Efecto de la fragilidad y la sarcopenia sobre el riesgo de caídas y de fracturas osteoporóticas en población no seleccionada. Rev Osteoporos Metab Miner 2020;12(3):81-6. DOI:10.4321/S1889-836X2020000300002 [ Links ]
Funding:
this original article was funded through a FEIOMM 2022 basic grant, with Carlos Gómez Alonso as the lead investigator.
This study has received partial funding from the European vertebral osteoporosis study (EVOS), E.U. (1991-1993); the European prospective osteoporosis study (EPOS), E.U. (BIOMED 93-95), the BMHI-CT 092-0182 (1993-1997); the Health Research Fund (FIS 94/1901-E); the Network of Renal Research (REDinREN) of ISCIII (RD06/0016/1013, RD12/0021/0023, RD16/0009/0017, RICORS2040 - Kidney Disease); the National R & D & I Plan 2008-2011, State R & D & I Plan 2013-2016, the European Regional Development Fund (ERDF), the Science, Technology, and Innovation Plan 2013-2017 and 2018-2022 of the Principality of Asturias (GRUPIN14-028, IDI-2018-000152, IDI-2021-000080), and Fundación Renal Iñigo Álvarez de Toledo (FRIAT).
Gómez Alonso C, Rodríguez García M, Naves López T, Llaneza Faedo M, Palomo Antequera C, Naves Mendívil L, Fernández Martín JL, Naves Díaz M. Should the FRAX tool include other variables to assess fragility-related osteoporotic fractures? Rev Osteoporos Metab Miner 2023;15(3):100-105
Received: June 01, 2023; Accepted: August 25, 2023











 texto em
texto em 




