Introduction
In December 2019, the first cases of people suffering from an unknown type of viral disease were identified in the Chinese city of Wuhan. On March 14, a state of emergency was declared in Spain and drastic quarantine measures were applied to all Spanish citizens. The Spanish population spent 47 days without leaving their home, with the only exceptions of purchase of food and medicine, assistance to health centers, travel to the workplace, return to habitual residence, care for dependents or travel to financial entities (RD 463/2020, BOE, 2020).
Loneliness is defined as an unpleasant experience or feeling associated with a lack of close relationships (de Jong Gierveld, 1998). It has two dimensions: social and emotional. According to Weiss (1973), social loneliness refers to a deficit in a person's social relations, social network, and social support; and emotional loneliness is a lack of closeness or intimacy with the other. Regarding the published studies on the impact on perceived loneliness in people in confinement due to COVID-19, the existing studies carried out in different countries concur that the situation of confinement aggravates feelings of loneliness. Okruszek et al. (2020) used a sample of 380 people from the Polish general population to analyze the relationship between loneliness and mental health during confinement and found that loneliness correlates positively with mental health symptoms. Mental well-being was examined with the 30-item version of the General Health Questionnaire (GHQ) (Frydecka, et al., 2010), which identifies five distinct factors corresponding to anxiety, feelings of incompetence, depression, difficulty in coping, and social dysfunction. Likewise, in a study carried out by our research team on the impact of COVID-19 in Spain, loneliness was one of the main predictors of symptoms of anxiety, depression and post-traumatic stress (González-Sanguino et al., 2020). Killgore et al. (2020) assessed the impact of social isolation due to COVID-19 on loneliness and mental health in the United States population. 93.6% of the sample reported that they were “sheltering-in-place”, and 61.5% endorsed feeling “socially isolated much of the time”. Lonely individuals were significantly more depressed than non-lonely. Regarding the relationship between loneliness and the age variable in the current pandemic, Losada-Baltar et al. (2020), used a sample of 1310 people from the general population and found that the younger they were, the greater perception of loneliness they had. Other studies found results in the same direction (Robb et al., 2020; Seifert & Hassler, 2020; van der Velden et al., 2021). The present study tries to evaluate the effects that COVID-19 emergency situation and quarantine have on the loneliness perceived in the Spanish population. In addition, the present study analyzes whether loneliness has increased or decreased in the Spanish general population and what its predictors are.
Method
Participants
The data collection was carried out by sending requests for participation to people who belonged to the databases of different institutions such as students and employees of public organizations like the Complutense University of Madrid and the Chair of Stigma; and private organizations such as the company Grupo 5 Respondents were requested to spread the survey in order to increase the sample to the maximum possible extent. The final sample consisted of 3480 people from the general population and some specific groups. The definitive sample included 3480 persons belonging to the general population and to some specific groups. The inclusion criteria were Being over 18 years of age; 2. Residing in Spain during the health emergency due to COVID-19.
Variables and instruments
The assessment included these variables and instruments:
-
Sociodemographic variables: ad hoc designed questions were used, age was gathered (posteriorly clustered: 18-30, 31-59, 60-80); sex; educational level (elementary studies, high school, vocational training, university, postgraduate); couple relationship (single, couple not sharing housing, and has couple and shares housing); profession (social-health, education, administration, business and others such as transport, communications or tourism); employment situation (working, unemployed, student, retired, unpaid domestic work, other situation); economic situation (subjective perception from very bad to very good); the presence of medical diagnosis (psychiatry and mental health, cardiovascular, neurological, respiratory or other diseases); the importance of religious beliefs.
Variables regarding to COVID-19: suffering symptoms (yes, no); having a negative or positive diagnosis; being hospitalized; family members or close relatives infected; living with someone infected; work situation (obliged to go to his/her place of employment or doing home-office); opinions about the information received during the state of emergency declaration (considering whether he/she received enough information, considering that he/she is overinformed).
Loneliness: measured by the 3-item version of the UCLA Loneliness Scale (UCLA-3) in its Spanish version (Velarde-Mayol et al., 2016), self-administered, and including the following items: 1. Since March 15, how often do you feel that you are short of company? 2. Since March 15, how often do you feel excluded? 3. Since March 15, how often do you feel isolated from others? The three items in Likert-type format with three possible responses (1 rarely, 2 sometimes, 3 often), address three dimensions of loneliness: relational connectedness, social connectedness and self-perceived isolation. A single item of loneliness is also included (Campaign to End Loneliness, 2015), “For the past week, have you been feeling lonely?”: Hardly ever (for example, less than 1 day); Sometimes or a small part of the time (for example, 1-2 days); Quite a long time (for example, 3-4 days); and All the time (e.g. 5-7 days). According to the data from the sample of the present study, Cronbach's α is .76.
Social support: evaluated using the Multidimensional Scale of Perceived Social Support (EMAS), adapted to Spanish (Landeta & Calvete, 2002). It consists of 12 Likert-type items with 7 response alternatives (1 totally disagree to 7 totally agree), it measures the perceived levels of social support. According to the data from the sample of the present study, Cronbach's α is .91.
Spiritual well-being: was assessed using the Spanish version of the Functional Assessment of Chronic Illness Therapy Spiritual Well-Being (FACIT-Sp12) (Cella et al., 1998). The responses were Likert type from 0 (nothing) to 4 (a great deal). Higher scores denote greater well-being. According to the data from the sample of the present study, Cronbach's α is .84.
Mental health symptoms: these screening instruments were used to assess possible symptomatology:
-
Patient Health Questionnaire 2 (PHQ-2), in its Spanish version (Diez-Quevedo et al., 2001). A brief self-report questionnaire that focuses on the frequency of depressive symptoms. It contains 2 Likert-type questions ranging from 0 “never” to 3 “every day”. Higher scores are indicative of more symptomatology, providing a severity score of .6, and establishing the cut-off at >3 points as a possible case of depression (Muñoz-Navarro et al., 2017). According to the data from the sample of the present study, Cronbach's α is .74.
Generalized Anxiety Disorder Scale (GAD-2), Spanish version (Garcia-Campayo et al., 2014). The GAD-2 Questionnaire includes the first 2 items of the GAD-7 Likert format, with a top score of 6 points. The cut-off point, in this case, is 3, from which the likelihood of identifying potential cases of anxiety is signaled (Muñoz-Navarro et al., 2017). According to the data from the sample of the present study, Cronbach's α is .82.
Civilian version of the Post-traumatic Stress Disorder Checklist (PCL-C), reduced version (Lang & Stein, 2005; Lang et al., 2012), with two Likert-type items inquiring about the occurence of particular phenomena related to the traumatic experience. The answers range is from 0 (nothing) to 4 (a great deal). According to the data from the sample of the present study, Cronbach's α is .88.
Discrimination: it was rated using the Intersectional Day-to-Day Discrimination Index (InDI-D) (Scheim & Bauer, 2019), in its Spanish version, which was translated by the authors of this study. This scale provides a measurement of the intersectional discrimination that can be produced by different conditions: sex, ethnicity, mental health diagnosis, and in this case, the presence of COVID-19 was also included. We used the main scale formed by 9 Likert-type items with four response options (1 never – 4 often). The different questions assessed the existence of intersectional discrimination from the beginning of the state of emergency caused by the pandemic. The higher the score the more discrimination suffered. According to the data from the sample of the present study, Cronbach's α is .74.
Internalized stigma: was measured by two items adapted from the Internalized Stigma of Mental Illness scale (Boyd et al., 2014), relating to the emotional and social isolation dimension. The items were altered so that they could evaluate intersectional internalized stigma, i.e., the self-stigma that can be generated by various conditions, including being diagnosed with COVID-19. According to the data from the sample of the present study, Cronbach's α is .46.
Self-Compassion Scale (SCS) was used in its Spanish version (Garcia-Campayo et al., 2014). The scale rates the subject's performance towards him/herself in difficult situations and different dimensions. In this study, we use 6 items to explore the following three areas: self-love, common humanity and mindfulness. The items are Likert type (1 to 5). Higher scores indicate greater self-compassion. According to the data from the sample of the present study, Cronbach's α is .88.
-
Procedure
An online survey was elaborated to be completed using the Google Forms platform to reach the largest population possible. Since face-to-face interviews were not possible to conduct due to confinement, data was instead collected online. The form was designed by expert psychologists in mental health assessment from the Faculty of Psychology at the Complutense University of Madrid. The survey included 80 questions and the average time for completion was about 7 minutes. The form included an email address so that respondents could ask questions about it if necessary. The procedure for applying the form was the same for all age groups. Also, the survey included a section with information regarding the research. Furthermore, it included the consent form to participate in the study and acceptance of the data protection laws regarding regulation (EU) 2016/679 of the European Parliament and of the Council, of 27 April 2016, on the protection of personal data. The survey was launched on 21 March and data was collected until 28 March 2020. The study was approved by the Deontological Commission of the Faculty of Psychology of the Complutense University of Madrid with the reference “pr_2019_20_029”.
Analysis
Descriptive statistics were calculated for socio-demographic and psychological variables. Frequencies and percentages are reported for categorical variables and means (with 95% CI) and standard deviations for numerical variables. The relationships between each variable in the study and loneliness measures (UCLA-3 and the single item of loneliness) were reported as a univariate R2 value, coefficients B (with a 95% CI), and standardized coefficients, B(std). For categorical variables, the reference level is indicated in the results tables. The significance of both R2 and coefficients is indicated with the traditional asterisk (* = p < .05, ** = p < .01, *** = p < .001).
In addition, linear regression models were estimated for each loneliness variable measure (UCLA-3 and the single item of loneliness) to test the predictive value of socio-demographic and psychological variables. Models were calculated by Least Squares and built with a theory-driven forward modeling approach (testing the R2 increase). Reports include coefficients B, standardized coefficients, B(std), adjusted R2 and the significance F test. Statistical analysis was performed using R (3.6.3).
Results
Loneliness
The scores on the UCLA-3 Loneliness scale averaged 4.55 (SD = 1.63), and the single item of loneliness reported mean scores of 1.52 (SD = .75). The results indicate that after 14 days of confinement, 8% of the people in the sample have felt alone 3 or 4 days, 34% have sometimes felt that they lacked company, 20% have sometimes felt excluded and 37% have sometimes felt isolated from others.
Sociodemographic data and loneliness
The sample (N = 3487) contained a majority of women (75%), 35.3% of whom were aged 18-30, 58.9% 31-59 and 5.8% 60-80. The average age was 37.92. Moreover, 52.6% of the participants declared that they had a partner and shared their home with their partner. 41% of the participants had children and 37.4% had university studies. 58.7% considered their economic situation as good or very good. 62.9% were actively working at the time of the interview. 84.2% of the people in the sample had not been diagnosed with a previous illness, with 6.1% having some previous mental health diagnosis. Table 1 and 2 shows the sociodemographic characteristics of the sample.
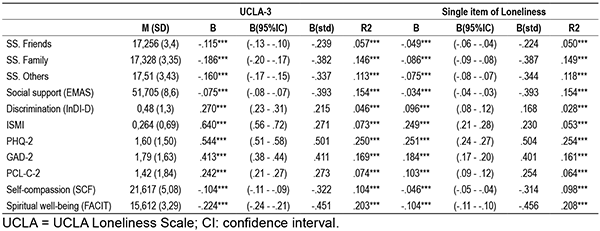
Table 1. Association between sociodemographic variables and loneliness variables (UCLA-3 and the single item of loneliness) during coronavirus (COVID-19) outbreak.

UCLA = UCLA Loneliness Scale; CI: confidence interval.
Being a woman had a positive relationship with the UCLA-3 (BSTD = .109) and a positive relationship with the single item of loneliness (BSTD = .117). Being older was significantly negatively related to UCLA-3 (BSTD = -.604), and the single item of loneliness (BSTD = --.174), compared to the younger age group (18-30). Furthermore, having a partner and sharing a house was associated with less loneliness, both in the UCLA-3 (BSTD = -.494) and in the single item of loneliness (BSTD = -.572).
Having children (BSTD = -.404; BSTD = -.451), university studies (BSTD = -.330; BSTD = -.377), being retired or working (BSTD = -.500; BSTD = -.453; BSTD = -.435; BSTD = -.299), placing quite a lot of value on religion (BSTD = -.189; BSTD = -.081) were significantly negatively related to UCLA-3 and to the single item of loneliness. Mixed results were found for some variables. In this regard, rating personal financial status as good to very good was significantly negatively related to UCLA-3 (BSTD = -.590), and significantly positively related to the single item of loneliness (BSTD = .542). Working as commercial or social health professional was significantly negatively related to UCLA-3 (BSTD = -.196; BSTD = -.209), and significantly positively related to the single item of loneliness (BSTD = .280; BSTD = .247). Being married was significantly negatively related to UCLA-3 (BSTD = -.521), and significantly positively related to single item of loneliness (BSTD = .395). On the contrary, having previous mental health problems was found to be positively related with UCLA-3 (BSTD = .628) and with 1-item loneliness (BSTD = .682).
COVID-19-related data and loneliness
Concerning COVID-19, .7% of the sample had been tested positive for COVID-19, 13.9% declared that they had suffered symptoms compatible with the disease, 2.7% had to live with an infected person, and 28.3% had a family member or close relative who had been diagnosed. About the information received about COVID-19, 57.5% stated that they had received sufficient information. Regarding the employment situation in relation to COVID-19, 43% of the sample could telework, and 16.4% had to go to the workplace.
Having current or previous symptoms compatible with the virus (BSTD = .246; BSTD = .340), or living with someone who was infected (BSTD = .341; BSTD = .246) was positively related to UCLA-3 and to the single item of loneliness, while receiving sufficient information was a protective factor in the appearance of loneliness (BSTD = -.290; BSTD = -.287).
In relation to the work situation and COVID-19, working face-to-face and teleworking were found to have a significantly negative association with UCLA-3 and with the single item of loneliness (BSTD = -.245; BSTD = --.207; BSTD = -.335; BSTD = -.311).
Psychosocial variables and loneliness
Depression, anxiety and PTSD (BSTD = .501; BSTD = .411; BSTD = .273) and discrimination (BSTD = .215; BSTD = .271) showed a significant positive relationship with the UCLA-3. Also, depression, anxiety and PTSD (BSTD = .504; BSTD = .401; BSTD = .254) and discrimination (BSTD = .168; BSTD = .230) showed a significant positive relationship with the single item of loneliness. While social support (BSTD = -.393; BSTD = -.393), well-being (BSTD = -.451; BSTD = -.456) and self-compassion (BSTD = -.322; BSTD = -.314) had a significantly negative relationship. Table 3 shows the results of psychosocial variables in more detail.
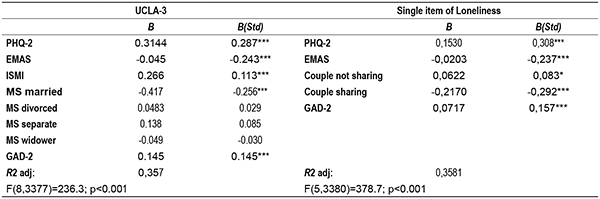
Regressions on loneliness
The model for the UCLA-3 was statistically significant, explaining 35.71% of the variance (F(8,3377)=236.3; p<.001). The significant variables were first depressive symptoms (BSTD = .287), followed by social support (BSTD = -.243), internalized stigma (BSTD = .113), married marital status (BSTD = -.256), and anxiety symptoms (BSTD = .145).
Concerning the single item of loneliness, the model was also statistically significant, explaining 35.81% of the variance (F(53380)=378.7; p<.001). The significant variables were depressive symptoms (BSTD = .308), social support (BSTD = -.237), having a partner but not sharing the same home (BSTD = .083), having a partner and sharing the same home (BSTD = -.292), as well as anxiety symptoms (BSTD = .157).
Table 4 shows the results of linear regressions.
Discussion
The present study shows the effects of the first weeks of state of alarm caused by COVID-19 on loneliness in the Spanish population, analyzing its relationship with mental health, social support and discrimination variables. The results indicate that after 15 days of confinement, 8% of the people in the sample have felt alone 3 or 4 days, 34% have sometimes felt that they lacked company, 20% have sometimes felt excluded and 37% have sometimes felt isolated from others. This represents an increase compared to previous data on our population, where 6% loneliness was found (European Quality of Life Survey, 2016).
In general, in relation to sociodemographic variables, being a woman, being diagnosed or having symptoms of COVID-19 and living with an infected person were associated with greater perceived loneliness. While being older, being married and sharing the house with your partner, having children, higher education, working and having enough information about the situation were protective against the appearance of loneliness. These results are consistent with the only study published at the moment in the scientific literature with a Spanish sample (Losada-Baltar et al., 2020), where they also found that women, younger age and living with other people had strong relationships with loneliness. In general, women present a greater emotional expressiveness, particularly for negative emotions (Deng et al., 2016), so they may show fewer difficulties in admitting and expressing their feelings of loneliness. Being married is a protective variable against loneliness if evaluated with the UCLA-3, but not when it was evaluated with the single item of loneliness. Living together as a couple is a protector factor against loneliness in 1-item loneliness. Having a good economic situation is negatively related to loneliness, in line with previous studies (Ausín et al., 2017, Cohen-Mansfield et al., 2016). Having a low income limits a person's ability to attend some social events. On the other hand, being discriminated, internalized stigma and having symptoms of anxiety, depression, or PSTD, and having previous diagnoses of mental health problems, is a predictor of loneliness. The association of loneliness with poorer mental and physical health has been demonstrated in previous studies (Courtin & Knapp, 2017; Leigh-Hunt et al., 2017) and also in a study conducted during confinement derived from COVID-19 (Killgore et al., 2020).
The main protective psychosocial variables we found was social support, spiritual well-being and self-compassion. During confinement, many of us will miss seeing family and friends and performing leisure and other regular activities. It is evident how important social relationships and connections with other people are in our lives and how difficult it can be when they are missing. Continuing to receive social support and promoting coping strategies that involve self-pity is essential for avoiding the appearance of unwanted loneliness. Spiritual well-being is also a clear protector, highlighting the importance of beliefs that perhaps help us to face situations with greater serenity, or even make us feel part of a community and not see ourselves alone in the face of the crisis.
In regression models, depression and social support are revealed as fundamental predictors of loneliness. Depressive symptomatology and its relationship with loneliness have occupied a relevant place in research up to now, with the relationship between both of them frequently being bidirectional (Ausín et al. 2017; Cohen-Mansfield et al., 2016; Courtin & Knapp, 2017; Leigh-Hunt et al., 2017; Losada et al., 2012). On the other hand, social support turned out to be the greatest protector against unwanted loneliness. While confinement has forced us to isolate ourselves and create a physical social distance, information and communication technologies and other traditional networks can foster social support to deal with loneliness. Online technologies (Armitage and Nellums, 2020; Brooke & Jackson, 2020, Jones & Keynes, 2020, Eghtesadi, 2020) could be leveraged to provide social support networks and a sense of belonging, even in groups most affected by technological illiteracy. These authors indicate the convenience of training older people in the use of digital resources, and the usefulness of interventions that involve more frequent telephone contact with significant people, close family and friends, voluntary organizations or health professionals, or community projects that provide support during the confinement situation. Furthermore, cognitive-behavioral approaches could be administered online to decrease loneliness and improve psychological well-being. On the other hand, several specialized psychological care services have put in place online systems to serve the population (Zhang, Wu, Zhao, & Zhang, 2020; Xiao, 2020), underlining the importance of social support. However, Dahlberg (2021) notes that remote social contacts cannot fully compensate for the loss of physical contact.
Other relevant predictors in the model include being married, which is a protector when we used the UCLA-3 scores and having a partner and sharing housing as a protector for the single item of loneliness. Meanwhile, having a partner but not sharing housing is a predictor of greater loneliness for this same item, and having a partner but not living with them in this situation also turned out to be a predictor in this item. While UCLA-3 may have a greater component of perception of rejection or exclusion, the single item for loneliness directly refers to perceived loneliness and, in this sense, on many occasions, restrictive measures of confinement prevented couples from seeing each other by not keeping contact despite living in the same home, which increased loneliness, as it was not a chosen situation.
The main limitations of the study included the fact that, despite the effort in recruitment, the resulting sample is not exactly equivalent to the Spanish population. This fact does not distort the results found, since the objective is not to provide epidemiological information or prevalence data but to compare the averages obtained by various social groups in the variables of interest. In this sense, as long as the sample meets the requirements of the statistical tests used, we believe it is valid for the study. However, it is necessary to be careful in the interpretation of the results and understand that they are limited by the characteristics of the sample obtained. Additionally, the number of men and older participants was lower than that of women and younger participants, with these groups being underrepresented. Furthermore, given the limited length of the survey, other interesting variables possibly related to perceived loneliness during confinement, such as neuroticism, paranoia, death anxiety, or intolerance of uncertainty, collected in the study by McBride et al. (2021), were not included.
The stay-at-home order to deal with COVID-19 is necessary, although, during the first two weeks, an increase in unwanted loneliness has been observed in the Spanish population, especially among women and younger people. Measures that favour social support while maintaining social physical distance, as well as a greater study of loneliness in groups of older and probably more isolated people are necessary to avoid a greater impact on our mental health and well-being caused by the pandemic.