INTRODUCTION
Therapeutic dropout occurs with great frequency in health care services. Between 30% and 60% of psychotherapy clients drop out of treatment prematurely (the dropout average is 47%; Bados et al., 2007; Hamilton et al., 2011; Levitt, 1968; Shift et al., 2017; Vöhringer et al., 2020; Wierzbicki & Pekarik, 1993). However, there are significant difficulties among researchers in finding consensus on the definition of therapeutic dropout (Hamilton et al., 2011; Henzen et al., 2016; Kareckla et al., 2019; Wierzbicki & Pekarik, 1993). This lack of agreement may help to understand the inconsistency of results regarding dropout rates and the variables that relate to dropout (Bados et al., 2007; Hamilton et al., 2011; Swift et al., 2009; Wierzbicki & Pekarik, 1993).
Therapeutic dropout has been defined as non-compliance with the pre-scheduled number of sessions in protocolized treatments (Kareckla et al., 2019). Given that most psychological treatments do not have a predefined number of total sessions, other studies define dropout as the non-attendance to scheduled sessions or the non-programming by the user of future sessions (Hatchett & Park, 2003; Swift et al., 2009). Other authors consider dropout when a minimum number of sessions or months of treatment are not met (Bados et al., 2007; Beckham, 1992; Gunderson et al., 1989). On the other hand, the therapist's clinical judgment has historically been considered one of the best defining criteria for therapeutic dropout (Hamilton et al., 2011; Henzen et al., 2016; Pekarik, 1992; Shift & Greenberg, 2014; Wierzbicki & Pekarik, 1993). However, this criterion alone may be biased as it is a subjective criterion. Hatchett and Park (2003) add as criteria unilateralism on the part of the patient in the decision and noncompliance with therapeutic goals. Thus, therapeutic dropout would be considered to occur when the user decides to unilaterally terminate therapy without having fulfilled, in the therapist's criterion, most of the therapeutic goals set. This will be the criterion used for the present work. Cases derived to another center that better fits the characteristics of the demand or the needs of the user are not considered dropouts. Similarly, clients who give up therapy before the first session do not meet the dropout criterion. Therefore, therapeutic abandonment is considered from the first session onwards.
Therapeutic dropout seems to be a common occurrence in psychotherapy, but it can lead to negative repercussions for both the clients and the therapist. In the case of the therapist, there seems to be a tendency to make an internal attribution of therapeutic dropout. Many professionals may attribute the dropout to the type of treatment they have designed, considering that it has failed. Such attributions affect therapist confidence (Klein et al., 2003; Maslach, 1978; Pekarik, 1983, 1985; Sledge et al., 1990). However, research shows that therapeutic dropout is not always related to the characteristics of the treatment (Pekarik, 1983), and therefore sometimes it is beyond the therapist's ability to act and control. In the case of the clients, when they discontinue therapy before having achieved the goals, they are negatively affected (Gersh et al., 2017; Lopes et al., 2018; McMurran et al., 2010; Pekarik, 1983; Vöhringer et al., 2020). After therapeutic abandonment, clinical symptomatology may worsen (García-Cabeza et al., 1999; Verdoux et al., 2000), and many clients find it necessary to seek psychological assistance again (Bueno-Heredia et al., 2001).
Given the important consequences of therapeutic dropout, it is necessary to study and understand this phenomenon, which could help to design strategies to prevent it. For this reason, several authors have tried to study the variables that are related to premature termination of therapy. Various clinical variables have been studied as possible predictors of therapeutic dropout. Most studies have found that the dropout rate tends to be higher in people with severe initial symptomatology (e.g., Freire-Arteta, 1990; Kazdin, 1990; Poster et al., 2021; Sharf & Primavera, 2009; Verdux et al, 2000). Most previous studies explore the characteristics of those who continue treatment, and it is observed that they experience significant improvement at the time of termination of therapy (e.g., Bados et al., 2007; Lopes et al., 2018). This is to be expected since treatment presumably culminates when the therapeutic goals have been achieved. However, in some studies it has been observed that certain users who drop out of therapy have also experienced improvement prior to dropout (Pekarik, 1983, 1992; Persons et al., 1988). The authors consider that the experienced improvement could lead people to consider that they no longer need to continue therapy. In any case, it would be expected that this improvement would be less than the one experienced at the time of termination of therapy by users who complete it (Persons et al., 1988), but this aspect needs to be further explored.
Regarding clinical problems, some studies have found that individuals with depressive symptoms (Bueno-Heredia et al., 2001; Hamilton et al., 2011; Henzen et al., 2016) tend to have lower dropout rates. However, other studies do not find this relation (Steel et al., 2000; Strakowski et al., 1998; Sharf & Primavera, 2009). On the other hand, there is a consensus regarding anxiety problems. Most studies show that the dropout rate among people with anxiety symptoms tends to be lower compared to other problems (Bados et al., 2007; Hamilton et al., 2011; Sharf & Primavera, 2009).
The aim of this work is to study the clinical variables that can influence therapeutic dropout. We will study the variables that previous research has related to dropout rates. Understanding the phenomenon of therapeutic dropout can help to detect vulnerable cases and to modify the therapist's actions to prevent the user from prematurely terminating therapy. This would favor the fulfillment of the goals set and therefore benefit the user and, presumably, the therapist's satisfaction, according to the findings of Klein et al. (2003), Maslach (1978), Pekarik (1983, 1985), and Sledge et al. (1990).
We will study the level of severity and evolution of the symptoms presented by the users at the moment of dropout, according to the therapist's assessment. For this purpose, the scores of the Global Assessment of Functioning Scale (GAFS; American Psychology Association; APA, 2000) at the beginning of therapy and at the moment of its termination will be taken as a criterion. This scale indicates the therapist's perception of the severity of symptoms and the consequent ability to adapt to the user's context.
First, we will compare the group who drop out of therapy and the group who complete therapy. It is expected that clients who complete treatment present a lower level of severity at the beginning of therapy than clients who drop out of the therapeutic process (Freire-Arteta, 1990; Sharf & Primavera, 2009; Verdux et al, 2000). We consider that a higher initial severity may cause clients to perceive changes easily and tend to abandon therapy earlier as they may consider that they have already improved sufficiently.
Secondly, we will conduct an intra-subject analysis. As we have mentioned, one of the possible reasons why people decide to drop out of therapy is because they already perceive a decrease in their distress compared to when they started therapy. Thus, we hypothesize that clients who drop out of therapy will show a significant improvement. Likewise, it is expected that at the time of dropout the clients' adaptation to their environment will be high enough to have a functional life (Sharf & Primavera, 2009). A score less than or equal to 60 on the GAFS (APA, 2000) implies a low level of adaptation, while those scores above 60 imply an adequate or high level. It is expected that most people who drop out do so with a GAFS above 60 so that, although they continue to have symptoms, they can function in their environment.
However, we expect to find significantly greater improvement in users who complete treatment. Since dropout occurs before therapeutic goals are met, the improvement will be lower in cases that do not complete treatment.
Finally, we formulated hypotheses related to the clinical problem identified by the therapist. We expect to find a lower dropout rate in users whose main problematic consists of anxious symptomatology (Hamilton et al., 2011; Sharf and Primavera, 2009) than in users presenting other clinical problems (such as mood disorders, adjustment disorders or interpersonal difficulties).
METHOD
Participants
The sample is made up of 298 clients (111 men and 187 women) of the Center of Applied Psychology of the Autonomous University of Madrid (CPA-UAM). The center has a database of clients. All cases that had given consent to participate in research work were selected. The nationality of the users is Spanish. The age ranged from 18 to 77 years, with a mean age of 29 years (standard deviation of 11 years).
Instruments
Global Assessment of Functioning Scale (GAFS; APA, 2000)
The GAFS (APA, 2000) allows the assessment of the client's severity and evolution during therapy. It is an instrument to be filled out by the therapist. The score range varies from 0 to 100. A value of 100 indicates that the person shows an absence of symptoms and a full adjustment to his or her environment. Values close to 0 indicate high severity and no adaptation to the environment, the person's own life or that of those around him/her being in danger. The GAFS shows high reliability (Cronbach's alpha = 0.98; Söderberg et al., 2005) and validity (Schwartz [2007] found that the Functional Assessment Rating Scale [FARS; Ward & Dow, 1994] significantly predicted the GAFS scores [F4,165 = 26.8, p <.001]).
Diagnosis
Each therapist recorded a unique diagnosis for each case based on the client's main problem. The therapists employed the diagnostic criteria of the DSM-IV-TR manual (APA, 2000). If the user's problem does not fit the diagnostic criteria for any specific disorder, they should indicate the category “other”. In our study, the categories reported in the database were as follows:
PROCEDURE
The sample was obtained from a University center dedicated to clinical and research based on a cognitive-behavioral approach. All of the therapists had master's degree in clinical psychology, although most of them had less than 5 years of experience. Users may come directly or by recommendation from other centers. Sessions have a cost, but the center have lower fees than other non-university centers. There are no specific admission criteria, since the center's therapists have the capacity and experience to attend users with different psychological problems. However, if a therapist considers that a user cannot receive adequate care at the center, the user will be derived to the service best suited to its characteristics (for example, cases that require medical attention before starting psychological therapy).
The users who participated in the study were those who signed, before the start of therapy, an informed consent form in which they accepted that their data could be used for research purposes. On the other hand, therapists assigned a score on the GAFS (APA, 2000) at the beginning and the end of the therapy. Also, the therapists made a diagnosis for each case taking into account the user's main problem.
For this work, data were analyzed for both users who dropped out of therapy and those who completed therapy and were discharged from therapy. The IBM SPSS Statistics 24 package was used for data management and statistical analysis.
RESULTS
First, we explored the dropout rate in the sample. Out of a total of 299 people, 88 (29.4%) dropped out of treatment before completion.
First, we studied the level of severity at the beginning of therapy, measured from the GAFS (APA, 2000) of the group of users who drop out (M = 56.82; SD = 15.45; N = 84) and the group of users who do not drop out (M = 6 1.11; SD = 12.98; N = 214). Student's t-test was significant: t (25) = -2.32, p = .017 < .05. Thus, there are significant differences in the GAFS at the time of initiation of therapy between the dropout group and the group that completes the treatment, i.e., the dropout group has higher initial symptom severity, as hypothesized.
Secondly, we compared the score obtained in the GAFS by the dropout group at the beginning of therapy with the score obtained in this index at the moment of premature termination of therapy (T-test for related samples). The GFA mean value of the dropout group at the beginning of therapy is 59.39 (SD = 16.36) and, as expected, it is observed that they improve significantly, given the score they show in the GFA at the moment of dropout (M = 71.15; SD = 14.92; t (61) = -6.94, p < .01). Also, as hypothesized, the estimated level of adaptation to the environment is, on average, higher than 60 points at the time of dropout.
When studying the differences in the level of improvement between the dropout group and the group that completes the treatment, we observed that users who drop out of therapy present a lower improvement index (M = 11.67; SD = 13.28) based on the GAFS (APA, 2000) than those who do not drop out (M = 28.73; SD = 19.28). The difference is significant (t (232) = -6.35, p < .01), as expected.
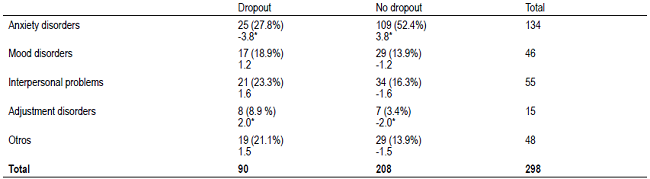
Finally, we employed a Pearson's Chi-square test to compare dropout rates between people with a diagnosis of anxiety and people with other clinical problems (Table 1). The statistic was significant (χ² (1, N = 298) = 15.91, p < .001). As expected, people with a diagnosis of anxiety tend to drop out of therapy to a lesser extent. It is also observed that people with adjustment disorders tend to drop out of therapy to a greater extent.
DISCUSSION
Therapeutic dropout is a phenomenon that occurs with some frequency in psychotherapy. The aim of this work was to study some of the most relevant clinical variables that have been linked to therapeutic dropout, with the particularity that we studied it in a type of center with certain specificity: a university clinic.
The dropout rate observed in the sample of this study is 29.5%, a level close to the one found in other studies, which ranges between 30% and 60%, and in any case lower than the average, which is 47% (Wierzbicki & Pekarik, 1993). We would like to highlight the study by Bados et al. (2007) since it was carried out with a university sample, similar to the one used in the present work. Bados et al. (2007) observed that 43.8% of users dropped out of therapy, a higher percentage than that found in the present study.
Our research aimed to find clinical factors associated with higher dropout rates. It has been observed that the presence of severe symptoms at the beginning of therapy, as estimated by the therapist, is associated with a higher dropout rate. In line with Freire-Arteta's (1990) findings, users who continue therapy seem to be those who are more adapted to their context, under the therapist's criteria, at the beginning of treatment.
In addition, dropout usually occurs at a time when the client has significantly improved his or her adaptation to the environment. At the time of dropout, the level of adaptation to the environment is, on average, above 70 points, indicating the presence of mild symptoms and moderate difficulties. Contrary to what one might think, dropout does not seem to be due to a termination of treatment derived from a lack of improvement but could be explained by the client's perception of improvement. When such a change is achieved, clients who initiate therapy with a high level of severity tend to drop out prematurely. This could be since they perceive that their symptomatology has improved, compared to the time when they started therapy, and consider that the change is sufficient. Therapists should pay special attention to the severity level of users, and the GAFS instrument (APA, 2000) can be useful in this regard. If scores on this instrument are close to 0, it indicates poor adaptation and, therefore, a high level of severity. The lower the score, the more effort the therapist will have to make to prevent dropout.
It is important to highlight that clients who drop out of therapy show a lower rate of improvement and a lower level of final adaptation (based on the GAFS; APA, 2000) than those who do not drop out. Thus, although the dropout group experience improvement, this does not mean that they have reached as high a level of improvement as if they had continued in therapy, nor that their therapeutic goals have been met. The latter does occur in the group that completes treatment since they achieve a significantly greater improvement than the group that drops out of therapy.
These results are decisive when establishing clinical recommendations to avoid dropout, and lead us to contemplate two direct implications for practitioners: implications for improving psychological care for users, and direct implications for professionals.
On the one hand, the results have implications for the therapist's own performance in relation to the users. Knowing these results, therapists should make an effort to educate their patients about how therapy works, especially patients who start treatment with severe symptomatology. The therapist should explain that clinical change takes time, and that it is common that, when experiencing some improvement, users consider that therapy can be done without. However, consolidating changes takes time, and finishing therapy prematurely can have negative long-term effects. At this point, it may be useful to explain that, according to the results of the literature, premature terminations may result in the need for more sessions in the future than would have been necessary if therapy had been completed.
On the other hand, the results presented have implications for the type of attributions that professionals make about their performance since, as indicated in the introduction, therapeutic dropout often has repercussions on the confidence of these professionals. In particular, these results are useful for professionals working in university clinics. In this type of clinics, it is common that most of the therapists are not experts. Non-expert therapists are the ones who tend to have the most doubts about their own performance, and the therapeutic dropout of patients can have a greatest effect. Our results show that university clinics also have an important percentage of dropouts, although in our study the percentage is not particularly high. We cannot conclude on the causal value of the clinical variables that we have linked to dropout, but it is clear that therapeutic dropout does not seem to depend directly on the therapist. Thus, we recommend that professionals take these results into account when alluding to the reasons why their patients do not continue in therapy, as they will undoubtedly help to offer an explanation with an adjusted effect on the professional. A patient dropping out does not necessarily mean that the therapist is not performing correctly. In fact, we have observed that some users drop out of treatment after experiencing some improvement, which means that the therapist's performance is going in the expected direction. Knowing the variables linked to therapeutic dropout, professionals can try to prevent it, but they must be aware of the extent of their ability to control the possibility of a patient leaving therapy prematurely.
Regarding clinical diagnosis, as hypothesized, the dropout rate is lower in clients with anxiety disorders than in those with other problems. Anxiety symptoms can become very incapacitating, which may make users with these symptoms more motivated to seek psychological help and complete treatment. Although no hypotheses were formulated about other clinical problems, it has been observed that the dropout rate is higher in users with adjustment disorders. These disorders appear when a negative event occurs in a person's life, provoking an excessive and disabling reaction. Perhaps, users with this type of problem expect to find an improvement or a resolution of their problems more quickly, and when they do not find it, they abandon therapy prematurely. Another possible explanation is based on the spontaneous disappearance of the negative event that was causing the person's discomfort, making therapy unnecessary. However, further studies will be necessary to contrast this possible explanation. In any case, these results allow us to add recommendations for therapists. It will be especially important for them to take actions to prevent therapeutic dropout in users with adjustment disorders (and, as we have seen above, therapists should pay special attention if these cases present severe symptoms at the beginning of therapy). For this type of cases, it will be also important for therapists to explain how therapy works and to emphasize the importance of meeting the established objectives. It may be useful for therapists to review the degree of compliance with the objectives at different points in the therapy, using graphs and providing estimates of the therapy time required until treatment termination. It may also be useful to explain that if the symptomatology is produced by a stressful event and this disappears, they may experience improvements, but in order to consolidate the changes and prevent future problems, it will be necessary for them to trust the therapist's judgment regarding the completion of therapy.
We consider that the main achievement of this work is to help provide useful information for professionals (mainly professionals from university clinics) with the aim of preventing therapeutic abandonment. The main practical implications are summarized and synthesized as follows. Therapists need to direct their efforts primarily to cases with higher initial severity and to cases with adjustment disorders, as these factors have been linked to higher dropout rates. We recommend therapists to educate users on how therapy works and dedicate time at different points in treatment to review the percentage of goal attainment so that users are aware of their progress and are aware that they have not yet reached all the goals they initially agreed upon with the therapist. It will also be important to convey to clients that, even if they experience improvement, it is necessary to continue therapy and consolidate the changes. On the other hand, we consider that therapists should be careful about the type of attributions they make regarding therapeutic dropout, since this is a complex phenomenon that cannot always be controlled by the therapist.
The main limitation of this study lies in the sample. The study participants are users of a university center, a context of a certain specificity. Likewise, most of the users are women. To be able to make generalizations, it would be necessary to obtain data from larger and more representative samples. Another important limitation is the impossibility of establishing causal relationships due to the type of data available. Similarly, we do not have data from the user's self-report on his or her symptomatology and problems, but only the therapist's assessment. Likewise, in this study, we have not analyzed data on the therapist (e.g., age, gender, years of experience), nor have we obtained data on the therapeutic alliance. It would be appropriate to carry out new studies that include both user and therapist variables to obtain a more complete picture of therapeutic abandonment. It is necessary to try to collect data on socioeconomic variables (Schmidt et al., 2020; Vöhringer et al., 2020; Zimmerman et al., 2017), and data about the reasons why people drop out of therapy (Ormhaug & Jensen, 2018), whether for economic reasons, lack of motivation, failure to meet expectations, etc. Indeed, it is sometimes difficult for people who drop out of therapy to express their reasons, but this would help us to obtain a more complete view of the phenomenon, analyzing which variables are linked to each type of dropout.
On the other hand, we believe that, in future studies, this work should be complemented with others that address other relevant variables such as the therapeutic alliance or the therapists' expertise. The therapeutic alliance has been identified as a factor that may be linked to therapeutic dropout, although results are mixed, and studies are still needed to better understand the role of the therapeutic alliance (e.g. Anderson et al., 2019; Busmann et al., 2019; Gersh et al., 2017; Gulamani et al., 2020; McEvoy et al., 2014; Sharf et al., 2010). For example, in the study of McEvoy et al. (2014) it was observed a relationship between interpersonal problems and the risk of dropping out of therapy, but this relationship is not mediated by the therapeutic alliance. On the other hand, Anderson et al. (2019) found that therapeutic alliance plays a mediational role between some factors (distress and therapy format) and dropout. With regard to the therapists' expertise, specially in nonexpert therapists as the ones in a university clinic, several authors agree that supervision and training are the variables that favor success and reduce therapeutic dropout instead of experience over the years that we have traditionally valued as positive (Burlingame et al., 1989; Gersh et al., 2017; Luque et al., 2021; Stein y Lambert, 1995).
These types of studies use therapist self-report to assess the therapeutic alliance or the supervision satisfaction. However, these are complex variables, and we believe that different methodologies should be used to study it. Thus, we believe that future studies should employ an observational methodology to explore the therapeutic alliance and the expertise moment by moment and explore its relationship with outcomes, as well as lack of commitment to tasks and, eventually, with therapeutic dropout.
In short, in this study, it has been observed that dropout occurs to a greater extent in cases that start therapy with more severe symptomatology and a poorer adaptation to their environment, according to the therapist's criteria. Likewise, it occurs especially in cases diagnosed with adjustment disorders and to a lesser extent those related to anxiety problems. In addition, dropout tends to occur when the client has experienced a significant improvement and when he/she presents a high level of adaptation to his/her environment. This phenomenon could be considered one of the causes of dropout, so it would be important to study it in greater depth. However, as expected, the improvement is greater in those who complete the therapeutic process. Therefore, if therapists detect clients that meet the characteristic factors of dropout, it is recommended that preventive actions be carried out to avoid therapeutic dropout. In these cases, it would be advisable for the therapist to explain to the client what the therapeutic process is like and what can be expected from the improvement process, emphasizing the importance of meeting the objectives set and consolidating the changes. Finally, we consider that it would be interesting that the university clinics show the results of the present and similar studies in the training that they provide to their professionals. Presenting these results may favor a better performance of therapists, helping to prevent both dropouts and the effect of these on the therapists themselves.